The Anesthetic Efficacy of Diphenhydramine and the Combination Diphenhydramine/Lidocaine for the Inferior Alveolar Nerve Block
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Clinical Research
The Anesthetic Efficacy of Diphenhydramine and
the Combination Diphenhydramine/Lidocaine
for the Inferior Alveolar Nerve Block
Jennifer Willett, DDS, MS,* Al Reader, DDS, MS,† Melissa Drum, DDS, MS,†
John Nusstein, DDS, MS,† and Mike Beck, DDS, MA‡
Abstract
The purpose of this prospective, randomized study was
to compare the degree of pulpal anesthesia obtained in
vital, asymptomatic teeth using 1.8 mL of 1% diphen-
T he inferior alveolar nerve block is the most frequently used injection technique for
achieving local anesthesia for mandibular restorative and surgical procedures. A
lidocaine solution is routinely used to achieve anesthesia. However, a patient may
hydramine with 1:100,000 epinephrine, 1.8 mL of 2% present to the practice with an allergy to several types of local anesthetics or recalls a
lidocaine with 1:100,000 epinephrine, and 3.6 mL of severe allergic reaction to an unknown anesthetic agent. Previous authors have advo-
2% lidocaine with 1:100,000 epinephrine combined cated the use of diphenhydramine for patients allergic to standard local anesthetics (1– 4).
with 1% diphenhydramine with 1:100,000 epinephrine The use of the antihistamine diphenhydramine in dentistry has been studied in
in inferior alveolar nerve blocks. We also studied injec- extraction models by a number of authors (1–5). When compared with a lidocaine or
tion and postinjection pain. An electric pulp tester was prilocaine solution, diphenhydramine was less effective (1–5). Its use in medicine for
used to test for anesthesia, in 4-minute cycles for 60 minor laceration repair has shown it was either less effective or equivalent to a lidocaine
minutes, of the second molars through the central solution (6 –10). No objective study has evaluated diphenhydramine for pulpal anes-
incisor. Anesthesia was considered successful when thesia. Therefore, it would be worthwhile to determine the effectiveness of diphenhy-
two consecutive 80 readings were obtained within 15 dramine if a patient allergic to local anesthetic agents presents for treatment and pulpal
minutes and the 80 reading was continuously sustained anesthesia is required.
through the 60th minute. Using the lidocaine solution, The inferior alveolar nerve block does not always result in successful pulpal
successful pulpal anesthesia ranged from 12% to 84%. anesthesia (11). Failure rates of 10% to 39% have been reported in experimental
For the combined lidocaine/diphenhydramine solution, studies (11). Clinical studies in endodontics (12–17) have found failure with the
successful pulpal anesthesia ranged from 4% to 60%. inferior alveolar nerve block occurring between 44% and 81% of the time. Therefore,
The diphenhydramine solution was irritating on injec- it would be advantageous to improve the success rate of the inferior alveolar nerve
tion and postinjection and resulted in a very low level block. Although Kim et al. (18) found that diphenhydramine blocked sodium channels
of anesthetic success. We concluded that a 1% diphen- in a similar manner to common local anesthetics, Nishizawa et al. (19) found it may
hydramine solution should be used cautiously for the have an anesthetic action that is independent of traditional binding sites, at least in
inferior alveolar nerve block. The combination lido- cortical synaptoneurosomes. Therefore, we wanted to explore if the addition of diphen-
caine/diphenhydramine solution was irritating postin- hydramine to a lidocaine solution would enhance the success of pulpal anesthesia in an
jection and was not as effective as a lidocaine solution inferior alveolar nerve block.
for pulpal anesthesia. (J Endod 2008;34:1446 –1450) The purpose of this prospective, randomized study was to compare the degree of
pulpal anesthesia obtained in vital, asymptomatic teeth using 1% diphenhydramine with
Key Words 1:100,000 epinephrine, 2% lidocaine with 1:100,000 epinephrine, and a combination
Diphenhydramine, inferior alveolar nerve block, lido- of 1% diphenhydramine with 1:100,000 epinephrine plus 2% lidocaine with 1:100,000
caine, local anesthesia epinephrine in an inferior alveolar nerve block. In addition, we also studied the pain of
injection and postinjection pain of the three solutions.
From *Private Practice, Columbus, Ohio; †Division of End- Materials and Methods
odontics and ‡Department of Oral Biology, The Ohio State Thirty adult subjects participated in this study. The subjects were in good health
University, Columbus, Ohio. and were not taking any medications that would alter their perception of pain. Exclusion
Address requests for reprints to Dr Al Reader, DDS, MS,
Department of Endodontics, College of Dentistry, The Ohio
criteria were as follows: younger than 18; older than 65 years of age: allergies to
State University, 305 W 12th Avenue, Columbus, OH 43210. diphenhydramine, local anesthetics, or sulfites; pregnancy; history of significant med-
E-mail address: reader.2@osu.edu. ical conditions; taking any medications that may affect anesthetic assessment (nonste-
0099-2399/$0 - see front matter roidal anti-inflammatory drugs, opioids, antidepressants, and alcohol); active sites of
Copyright © 2008 American Association of Endodontists. pathosis in area of injection; and inability to give informed consent. The Ohio State
doi:10.1016/j.joen.2008.09.005
University Human Subjects Review Committee approved both the protocol and informed
consent document, and written informed consent was obtained from each subject.
The subjects randomly received each of three solutions in an inferior alveolar
nerve block at three separate appointments, spaced at least 1 week apart, in a crossover
design. The three solutions were 1.8 mL of 2% lidocaine with 1:100,000 epinephrine,
1.8 mL of 1% diphenhydramine with 1:100,000 epinephrine, and 3.6 mL of a combi-
1446 Willett et al. JOE — Volume 34, Number 12, December 2008Clinical Research
TABLE 1. Pain Ratings for Solution Deposition for the Three Solutions
Injection Phase None Mild Moderate Severe
Solution deposition
1% diphenhydramine 0% (0/10) 10% (1/10) 40% (4/10) 50% (5/10)
2% lidocaine 24% (6/25) 40% (10/25) 32% (8/25) 4% (1/25)*
1% diphenhydramine plus
2% lidocaine 16% (4/25) 28% (7/25) 40% (10/25) 16% (4/25)
n ⫽ 10 for the 1% diphenhydramine solution, n ⫽ 25 for the 2% lidocaine solution, and n ⫽ 25 for the 1% diphenhydramine plus 2% lidocaine solution.
*There was no significant (p ⫽ 0.074) difference between the lidocaine solution and combination diphenhydramine/lidocaine solution.
nation of 1.8 mL of 2% lidocaine with 1:100,000 epinephrine and 1.8 Each solution was prepared, under sterile conditions, as follows.
mL of 1% diphenhydramine with 1:100,000 epinephrine. However, be- For the lidocaine solution, 1.8 mL of a 2% lidocaine solution (Elkins-
cause of the irritating nature of the 1% diphenhydramine solution (Ta- Sinn, Inc, Cherry Hill, NJ), at a pH of 5 to 6, was drawn into a sterile 5-mL
bles 1 and 2) and the lack of anesthetic success (Table 3), this solution Luer-Lok plastic disposable syringe (Becton Dickinson Co, Rutherford,
administration was discontinued after 10 subjects. Thirty subjects ran- NJ) to which 18 L of 1:1,000 epinephrine (Luitpold Pharmaceuticals,
domly received each of two remaining solutions in an inferior alveolar Inc, Shirley, NY) was added using a calibrated Hamilton microsyringe
nerve block at two separate appointments, spaced at least 1 week apart, (Hamilton Microsyringe, Reno, NV). For the 1% diphenhydramine so-
in a crossover design. With the crossover design, there were 60 total lution, a 50-mg/mL (5%) solution of diphenhydramine HCL solution
injections administered for the lidocaine solution and combination di- (Steris Laboratories, Inc, Phoenix, AZ), at a pH of 5 to 6, was diluted
phenhydramine/lidocaine solution, and each subject served as his/her with sterile saline (Abbott Laboratories, North Chicago, IL) to achieve a
own control. Thirty block injections were administered on the right 1% solution. One and eight tenths milliliters of the 1% diphenhydramine
side, and 30 injections were administered on the left side. The same side solution was drawn into a Luer-Lok syringe to which 18 L of epineph-
randomly chosen for the first injection was used again for the second rine (1:1000) was added. The combination solution had each of the two
injection. The test teeth chosen for the experiment were the first and solutions prepared separately and then placed in a 5-mL Luer-Lok sy-
second molars, first and second premolars, and lateral and central ringe for a total volume of 3.6 mL. The solutions were prepared imme-
incisors. The contralateral canine was used as the unanesthetized con- diately before administration.
trol to ensure that the pulp tester was operating properly and that the At the beginning of each appointment and before any injections
subject was responding appropriately during each experimental por- were given, the experimental teeth and control contralateral canine
tion of the study. Clinical examinations indicated that all teeth were free were tested three times with the pulp tester (Kerr; Analytic Technology
of caries, large restorations, and periodontal disease; none had histo- Corp, Redmond, WA) to record baseline vitality. After the tooth to be
ries of trauma or sensitivity. tested was isolated with cotton rolls and dried with gauze, toothpaste
Before the experiment, the three solutions were randomly as- was applied to the probe tip, which was then placed midway between the
signed four-digit numbers from a random number table. Each subject gingival margin and the occlusal or incisal edge of the tooth. The current
was randomly assigned to each of the three solutions to determine rate was set at 25 seconds to increase from no output (0) to the maxi-
which solution was to be administered at each appointment. Only the mum output (80). The number associated with the initial sensation was
random numbers were recorded on the data-collection and postinjec- recorded. Trained research personnel performed all preinjection and
tion survey sheets to blind the experiment. After the diphenhydramine postinjection tests.
solution was discontinued, the random numbers for the two remaining Before the injection, each subject was instructed on how to rate the
solutions were used to determine the order of anesthetic administra- pain for deposition of anesthetic solution using a four-point scale. Zero
tion. was no pain. One was mild pain (pain that was recognizable but not
TABLE 2. Percentages and Discomfort Ratings for Postinjection Survey
Solution None Mild Moderate Severe
Day 0*
1% diphenhydramine 0% (0/10) 20% (2/10) 80% (8/10) 0% (0/10)
2% lidocaine† 68% (17/25) 24% (6/25) 8% (2/25) 0% (0/25)
Diphenhydramine plus lidocaine 12% (3/25) 36% (9/25) 36% (9/25) 16% (4/25)
Day 1
1% diphenhydramine 0% (0/10) 40% (4/10) 60% (6/10) 0% (0/10)
2% lidocaine† 80% (20/25) 16% (4/25) 4% (1/25) 0% (0/25)
Diphenhydramine plus lidocaine 4% (1/25) 64% (16/25) 28% (7/25) 4% (1/25)
Day 2
1% diphenhydramine 30% (3/10) 50% (5/10) 20% (2/10) 0% (0/10)
2% lidocaine† 88% (22/25) 12% (3/25) 0% (0/25) 0% (0/25)
Diphenhydramine plus lidocaine 24% (6/25) 64% (16/25) 12% (3/25) 0% (0/25)
Day 3
1% diphenhydramine 40% (4/10) 40% (4/10) 20% (2/10) 0% (0/10)
2% lidocaine† 100% (25/25) 0% (0/25) 0% (0/25) 0% (0/25)
Diphenhydramine plus lidocaine 40% (10/25) 52% (13/25) 8% (2/25) 0% (0/25)
n ⫽ 10 for the 1% diphenhydramine solution, n ⫽ 25 for the 2% lidocaine solution, and n ⫽ 25 for the 1% diphenhydramine plus 2% lidocaine solution.
*Rating at the time subjective numbness wore off.
†There was a significant (p ⬍ 0.001) difference between the lidocaine solution and combination diphenhydramine/lidocaine solution.
JOE — Volume 34, Number 12, December 2008 Diphenhydramine and Diphenhydramine/Lidocaine for Inferior Alveolar Nerve Block 1447Clinical Research
TABLE 3. Percentages and Number of Subjects Who Experienced Anesthetic Success with the Diphenhydramine, Lidocaine, and Combination Diphenhydramine/
Lidocaine Solutions
Solution
Diphenhydramine Lidocaine Diphenhydramine/lidocaine
Anesthetic success
Second molar 10% (1/10) 84% (21/25) 60% (15/25)
First molar 0% (0/10) 52% (13/25) 24% (6/25)
Second premolar 0% (0/10) 52% (13/25) 28% (7/25)
First premolar 0% (0/10) 68% (17/23)* 20% (5/23)*
Lateral incisor 0% (0/10) 36% (9/25) 20% (5/25)
Central incisor 0% (0/10) 12% (3/25) 4% (1/25)
n ⫽ 10 for the 1% diphenhydramine solution, n ⫽ 25 for the 2% lidocaine solution, and n ⫽ 25 for the 1% diphenhydramine plus 2% lidocaine solution.
*Two teeth were missing because of orthodontic extractions.
discomforting). Two was moderate pain (pain that was discomforting Five subjects in the combination diphenhydramine/lidocaine
but bearable). Three was severe pain (pain that caused considerable group did not return for subsequent appointments because of either the
discomfort and was difficult to bear). Immediately after the nerve block, painful injection or postinjection pain. Therefore, these five subjects
each subject rated the pain for anesthetic solution deposition. were removed from the data analysis, and because equal numbers were
All subjects received a conventional inferior alveolar nerve block required for statistical comparison, the corresponding five subjects
as described by Jorgensen and Hayden (20). The needle used for all were also removed from the lidocaine group.
injections was a 27-gauge 1½-inch needle (Monoject; Sherwood Med- One hundred percent of the subjects used for data analysis had
ical, St Louis, MO). All three anesthetic solutions were administered at profound lip anesthesia. The 10 subjects receiving the 1% diphenhy-
a rate of 1.8 mL/min. All injections were given by the senior author (JW). dramine also had profound lip numbness. Anesthetic success is pre-
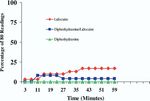
At 1 minute after each block was given, the first and second molars sented in Table 3. For the 1% diphenhydramine solution, only one
were pulp tested. At 2 minutes, the first and second premolars were tested. subject achieved success (second molar); the other teeth had no anes-
At 3 minutes, the lateral and central incisors were tested. At 4 minutes, the thetic successes. The lidocaine solution had successful anesthesia rang-
contralateral canine was pulp tested, and the subject was asked if his/her lip ing from 12% to 84%. For the combination diphenhydramine/lidocaine
was numb. This cycle of testing was repeated every 4 minutes for 60 minutes. solution, successful anesthesia ranged from 4% to 60%. Figures 1
At every third cycle, the control tooth, the contralateral canine, was tested by through 6 present the incidence of pulpal anesthesia (80 readings) for
a pulp tester without batteries to test the reliability of the subject. If profound the three anesthetic solutions. With all evaluation time periods com-
lip numbness was not recorded within 20 minutes, the block was consid- bined for each tooth, logistic regression showed significant differences
ered unsuccessful and the subject was reappointed. All testing was stopped (p ⬍ 0.015) between the lidocaine solution and combination diphen-
at 60 minutes after injection. hydramine/lidocaine solution for each of the six teeth. The 1% diphen-
All subjects completed postinjection surveys after each inferior alveo- hydramine solution had a low incidence of pulpal anesthesia for all the
lar nerve block administered. The subjects rated pain in the injection area, teeth (Figs. 1– 6).
using the identical scale previously described, immediately after the numb- The postinjection pain ratings are summarized in Table 2. The 1%
ness wore off and again each morning upon arising for 3 days. diphenhydramine solution had 80% of the subjects experience moderate
No response from the subject at the maximum output (80 reading) pain when the anesthesia wore off, with 60% experiencing moderate pain on
of the pulp tester was used as the criterion for pulpal anesthesia. Anes- day 1 and 20% on days 2 and 3. The combination diphenhydramine/lido-
thesia was considered successful when two consecutive 80 readings caine solution had a higher incidence of moderate to severe pain, when
were obtained within 15 minutes and the 80 reading was continuously compared with the lidocaine solution, when anesthesia wore off and for days
sustained through the 60th minute (ie, for most restorative procedures, 1 to 3. There were significant differences (p ⬍ 0.001) between the lido-
we would want the patient numb within 15 minutes and to remain numb
through the 60th minute). With a nondirectional alpha risk of 0.05 and
a power of 80%, a sample size of 25 subjects for each solution was
required to demonstrate a difference of ⫾25% in anesthetic success.
Comparisons between the lidocaine solution and the combination
diphenhydramine/lidocaine solution for differences in the incidence of
pulpal anesthesia (80 readings), for all evaluation time periods com-
bined for each tooth, were evaluated using logistic regression. Pain
rating differences for solution deposition and postoperative pain were
assessed using the Wilcoxon matched-pairs, signed-ranks test. Compar-
isons were considered significant at p ⬍ 0.05.
Results
Thirty adult subjects, 7 women and 23 men aged 20 to 29 years
with an average age of 26 years, participated.
The discomfort ratings of solution deposition for the three solu-
tions are presented in Table 1. Moderate to severe pain was experienced
by 90% of the subjects receiving the 1% diphenhydramine solution. Figure 1. The incidence of second molar anesthesia as determined by the lack
There was no significant (p ⫽ 0.074) difference between the lidocaine of response to electrical pulp testing at the maximum setting (percentage of
solution and combination diphenhydramine/lidocaine solution. 80/80’s) at each postinjection time interval for the three solutions.
1448 Willett et al. JOE — Volume 34, Number 12, December 2008Clinical Research
Figure 2. The incidence of first molar anesthesia as determined by the lack of
Figure 4. The incidence of first premolar anesthesia as determined by the lack
response to electrical pulp testing at the maximum setting (percentage of 80/
of response to electrical pulp testing at the maximum setting (percentage of
80’s) at each postinjection time interval for the three solutions.
80/80’s) at each postinjection time interval for the three solutions.
caine solution and combination diphenhydramine/lidocaine solution for all
istration of the diphenhydramine solution based on these findings. Pre-
postinjection days.
vious authors (1–5), using extraction models, have found diphenhy-
dramine when compared with a lidocaine or prilocaine solution to be
Discussion less effective. In the current study, all the subjects had lip numbness with
We based our use of the pulp test reading of 80 (signaling maxi- the injection of 1% diphenhydramine, but pulpal anesthesia was very
mum output) as a criterion for pulpal anesthesia on the studies of poor (Table 3 and Figs. 1– 6). Because lip numbness occurs with di-
Dreven et al. (21) and Certosimo and Archer (22). These studies (21, phenhydramine, previous authors (1–5) may have concluded that pul-
22) showed that no patient response to an 80 reading ensured pulpal pal anesthesia would also occur. Obviously, lip numbness does not
anesthesia in vital asymptomatic teeth. Additionally, Certosimo and Ar- always indicate pulpal anesthesia.
cher (22) showed that electric pulp test readings less than 80 resulted Diphenhydramine’s use as an anesthetic agent in medicine for
in pain during operative procedures in asymptomatic teeth. Therefore, minor laceration repair has shown it was either less effective or equiv-
using the electric pulp tester before beginning dental procedures on alent to a lidocaine solution (6 –10). Studies by Green et al. (9) and
asymptomatic vital teeth will provide the clinician a reliable indicator of Ernst et al. (6, 10) for minor laceration repair have also shown that the
pulpal anesthesia. Because all subjects felt profound lip numbness but injection of diphenhydramine caused more pain than the injection of a
pulp testing revealed that subjects did not always have pulpal anesthesia lidocaine solution, with one report of skin necrosis (7). Clause and
(80 readings), asking the patient if the lip is numb only indicates soft- Zach (23) reported an adverse postoperative reaction to the maxillary
tissue anesthesia but does not guarantee successful pulpal anesthesia. anterior injection of 1.8 mL of 1% diphenhydramine with 1:100,000
We had originally intended to study the use of 1% diphenhydra- epinephrine in a dental patient allergic to local anesthetics. Facial
mine in all 30 subjects. However, the overall pain caused during anes- edema, extensive nasal swelling with complete occlusion of the nasal
thetic solution deposition (Table 1), the moderate pain ratings for passageway, and infraorbital ecchymosis occurred, which resolved by 2
postinjection discomfort (Table 2), and the lack of anesthetic success weeks. From the results of the current study, a 1% diphenhydramine
(Table 3 and Figs. 1– 6), the injection of 1% diphenhydramine alone solution appears to be quite irritating. The Drug Information Handbook
was discontinued. It would have been unethical to continue the admin-
Figure 3. The incidence of second premolar anesthesia as determined by the Figure 5. The incidence of lateral incisor anesthesia as determined by the lack
lack of response to electrical pulp testing at the maximum setting (percentage of of response to electrical pulp testing at the maximum setting (percentage of
80/80’s) at each postinjection time interval for the three solutions. 80/80’s) at each postinjection time interval for the three solutions.
JOE — Volume 34, Number 12, December 2008 Diphenhydramine and Diphenhydramine/Lidocaine for Inferior Alveolar Nerve Block 1449Clinical Research
a young adult population, the results of this study may not apply to
children or the elderly.
We concluded that a 1% diphenhydramine solution should be used
cautiously for the inferior alveolar nerve block. The combination lido-
caine/diphenhydramine solution was irritating postinjection and was
not as effective as a lidocaine solution for pulpal anesthesia.
References
1. Meyer RA, Jakubowski W. Use of tripelennamine and diphenhydramine as local
anesthetics. J Am Dent Assoc 1964;69:112–7.
2. Welborn JF, Kane JP. Conduction anesthesia using diphenhydramine HCL. J Am Dent
Assoc 1964;69:706 –9.
3. Gallo WJ, Ellis E III. Efficacy of diphenhydramine hydrochloride for local anesthesia
before oral surgery. J Am Dent Assoc 1987;115:236 – 6.
4. Uckan S, Guler N, Sumer M, Ungor M. Local anesthetic efficacy for oral surgery:
comparison of diphenhydramine and prilocaine. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 1998;86:26 –30.
Figure 6. The incidence of central incisor anesthesia as determined by the lack 5. Malamed SF. Diphenhydramine hydrochloride. Its use as a local anesthetic in den-
of response to electrical pulp testing at the maximum setting (percentage of tistry. Anesth Prog 1973;20:76 – 82.
80/80’s) at each postinjection time interval for the three solutions. 6. Ernst AA, Anand P, Nick T, Wassmuth S. Lidocaine versus diphenhydramine for
anesthesia in the repair of minor lacerations. J Trauma 1993;34:354 –7.
7. Dire DJ, Hogan DE. Double-blinded comparison of diphenhydramine versus lido-
for Dentistry (24) does not recommend using diphenhydramine for caine as a local anesthetic. Ann Emerg Med 1993;22:1419 –22.
infiltration or block injection because of its irritating properties. There- 8. Ernst AA, Marvez-Valls E, Mall G, Patterson J, Xie X, Weiss SJ. 1% lidocaine versus
0.5% diphenhydramine for local anesthesia in minor laceration repair. Ann Emerg
fore, because of its very low rate of anesthetic success and irritating Med 1994;23:1328 –32.
properties, diphenhydramine should be used cautiously to achieve pul- 9. Green SM, Rothrock SG, Gorchynski J. Validation of diphenhydramine as a dermal
pal anesthesia in dental patients allergic to local anesthetics. local anesthetic. Ann Emerg Med 1994;23:1284 –9.
For anesthetic solution deposition, the combination diphenhydra- 10. Ernst AA, Marvez-Valls E, Nick TG, Wahle M. Comparison trial of four injectable
anesthetics for laceration repair. Acad Emerg Med 1996;3:228 –33.
mine/lidocaine solution was not significantly more painful when com- 11. Nusstein J, Reader A, Beck M. Anesthetic efficacy of different volumes of lidocaine
pared with the lidocaine solution (Table 1) but was significantly more with epinephrine for inferior alveolar nerve blocks. Gen Dent 2002;50:372–5.
painful for all postinjection days (Table 2). Apparently, the irritating 12. Cohen HP, Cha BY, Spangberg LSW. Endodontic anesthesia in mandibular molars: a
nature of the diphenhydramine was still present in the postinjection clinical study. J Endod 1993;19:370 –3.
periods even though the solution was diluted by the addition of lido- 13. Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supple-
mental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg
caine. Anesthetic success was lower with the diphenhydramine/lido- Oral Med Oral Pathol Oral Radiol Endod 1997;84:676 – 82.
caine solution (Table 3), and logistic regression showed significant 14. Nusstein J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the supple-
differences (p ⬍ 0.015) between the lidocaine solution and combina- mental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irre-
tion diphenhydramine/lidocaine solution for each of the six teeth. The versible pulpitis. J Endod 1998;24:487–91.
15. Kennedy S, Reader A, Nusstein J, Beck M, Weaver J. The significance of needle
diphenhydramine and lidocaine solutions were believed to be compat- deflection in success of the inferior alveolar nerve block in patients with irreversible
ible because both are water soluble with similar pH values. No precip- pulpitis. J Endod 2003;29:630 –3.
itate or chemical change appeared to occur when the solutions were 16. Claffey E, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of articaine for
combined. In general, the less effectiveness of the combination solution inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod
may indicate a similar binding site for diphenhydramine and lidocaine 2004;30:568 –71.
17. Bigby J, Reader A, Nusstein J, Beck M. Anesthetic efficacy of lidocaine/meperidine for
or the diphenhydramine may change the binding site for lidocaine. inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod
Although Nishizawa et al. (19) found that diphenhydramine may have an 2007;33:7–10.
anesthetic action that is independent of traditional binding sites, this 18. Kim YS, Shin YK, Lee C, Song J. Block of sodium currents in rat dorsal root ganglion
action may not be operable for the inferior alveolar nerve block. There- neurons by diphenhydramine. Brain Res 2000;881:190 – 8.
19. Nishizawa Y, Gusovsky F, Daly JW. Local anesthetics: comparison of effects on batra-
fore, the addition of 1.8 mL of 1% diphenhydramine with 1:100,000 chotoxin-elicited sodium flux and phosphoinositide breakdown in guinea pig cere-
epinephrine to 1.8 mL of 2% lidocaine with 1;100,000 epinephrine does bral cortical synaptoneurosomes. Mol Pharmacol 1988;34:707–13.
not enhance anesthetic efficacy. 20. Jorgensen NB, Hayden J Jr. Premedication, local and general anesthesia in dentistry.
Generally, the conventional inferior alveolar nerve block had sim- 2nd ed. Philadelphia, PA: Lea & Febiger; 1967.
ilar rates of anesthetic success as other studies of the inferior alveolar 21. Dreven L, Reader A, Beck M, Meyers W, Weaver J. An evaluation of the electric pulp
tester as a measure of analgesia in human vital teeth. J Endod 1987;13:233– 8.
nerve block (11). For example, Nusstein et al. (11) found success rates 22. Certosimo A, Archer R. A clinical evaluation of the electric pulp tester as an indicator
ranged from 44% to 53% for the first molar, 61% to 67% for the first of local anesthesia. Oper Dent 1996;21:25–30.
premolar, and 32% to 35% for the lateral incisor. These are similar to 23. Clause DW, Zach GA. Reaction to diphenhydramine hydrochloride (Benadryl) used
the success rate of 52% for the first molar, 68% for the first premolar, as a local anesthetic. Gen Dent 1989;37:426 –7.
24. Wynn RL, Meiller TF, Crossley HL. Drug information handbook for dentistry. 10th ed.
and 36% for the lateral incisor in the current study (Table 3). The Hudson, OH: Lexi-Comp, Hudson; 2006:451.
lidocaine solution did not provide complete pulpal anesthesia for the 25. Parente SA, Anderson RW, Herman WW, Kimbrough WF, Weller RN. Anesthetic effi-
mandibular teeth (Table 3 and Figs. 1– 6), which could present mean- cacy of the supplemental intraosseous injection for teeth with irreversible pulpitis. J
ingful clinical problems because the teeth may not be numb for proce- Endod 1998;24:826 – 8.
dures requiring complete pulpal anesthesia. Practitioners should con- 26. Nusstein J, Kennedy S, Reader A, Beck M, Weaver J. Anesthetic efficacy of the supple-
mental X-tip intraosseous injection in patients with irreversible pulpitis. J Endod
sider supplemental techniques, such as intraosseous (13, 14, 25–27) 2003;29:724 – 8.
or periodontal ligament injections (12) when a lidocaine solution fails 27. Bigby J, Reader A, Nusstein J, Beck M, Weaver J. Articaine for supplemental intraosse-
to provide pulpal anesthesia for a particular tooth. Because we studied ous anesthesia in patients with irreversible pulpitis. J Endod 2006;32:1044 –7.
1450 Willett et al. JOE — Volume 34, Number 12, December 2008You can also read