Deliveries in maternity homes in Norway: results from a 2-year prospective study
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Acta Obstet Gynecol Scand 2002: 81: 731–737 Copyright C Acta Obstet Gynecol Scand 2002
Printed in Denmark . All rights reserved
Acta Obstetricia et
Gynecologica Scandinavica
ISSN 0001-6349
ORIGINAL ARTICLE
Deliveries in maternity homes in Norway:
results from a 2-year prospective study
NINA SCHMIDT1, BIRGIT ABELSEN2 AND PÅL ØIAN3
From 1Alta Maternity home, Alta, 2Finnmark College, Alta, and the 3Department of Obstetrics and Gynecology,
University Hospital of Tromsø, Tromsø, Norway
Acta Obstet Gynecol Scand 2002; 81: 731–737. C Acta Obstet Gynecol Scand 81 2002
Background. The study aims to report the short-term outcome for the mothers and
newborns for all pregnancies accepted for birth at maternity homes in Norway.
Methods. A 2-year prospective study of all mothers in labor in maternity homes, i.e. all
births including women and newborns transferred to hospital intra partum or the first week
post partum.
Results. The study included 1275 women who started labor in the maternity homes in
Norway; 1% of all births in Norway during this period. Of those who started labor in a
maternity home, 1217 (95.5%) also delivered there while 58 (4.5%) women were transferred
to hospital during labor. In the post partum period there were 57 (4.7%) transferrals of
mother and baby. Nine women had a vacuum extraction, one had a forceps and three had a
vaginal breech (1.1% operative vaginal births in the maternity homes). Five babies (0.4%)
had an Apgar score below 7 at 5 min. There were two (0.2%) neonatal deaths; both babies
were born with a serious group B streptococcal infection.
Conclusion. Midwives and general practitioners working in the districts can identify a low-
risk population (estimated at 35%) of all pregnant women in the catchment areas who can
deliver safely at the maternity homes in Norway. Only 4.5% of those who started labor in the
maternity homes had to be transferred to hospital during labor.
Key words: centralization of births; low-risk births; maternity homes.
Submitted 23 July, 2001
Accepted 4 January, 2002
Centralization of births in larger hospitals has oc- formal medical leader. There are no obstetricians,
curred in many European countries, and conse- pediatricians, anesthetists or surgeons present, and
quently a number of small rural maternity homes there are no facilities for emergency cesarean sec-
have been closed (1,2). In sparsely populated areas tions.
there should be a balance between the efficiency of It has been argued that it is difficult to predict
larger hospitals and accessibility of care to all in birth complications, and as a consequence, the
smaller units. The general trend in Europe seems centralization of deliveries to larger departments,
to be in favor of the first alternative. In Norway, where all available medical support is at hand, has
there has been a strong centralization of births been cited as safer for both the mother and baby
over the past 25 years. In 1971 there were 158 insti- (3–6). This argumentation is, however, based on
tutions providing birth care, while the number is scarce scientific evidence. In Norway, 500 births
now approximately 60. The numbers of maternity per year are considered to be the minimum level of
homes have been reduced from 30 in 1980 to 10 at activity for birth institutions. If women are to have
present. However, Norway still has approximately a choice in their place of delivery, the maternity
30% more birth institutions than Sweden and Fin- services should provide a safe and acceptable range
land. A maternity home is a delivery unit run by of options. The debate over the place of birth
midwives with a general practitioner (GP) as the raises many fundamental questions about the gen-
C Acta Obstet Gynecol Scand 81 (2002)732 N. Schmidt et al.
eral management of labor, patient satisfaction, and
Maternity homes in Norway
women’s right to choose their preferred kind of
care. The most essential question is, however, are Norway is a sparsely populated country where
we able to select high risk from low risk? mountains and fjords, in addition to a harsh cli-
The present study aims to document the practice mate in many locations, result in considerable dif-
at the maternity homes in Norway and address ficulties in transporting women in labor. Six of the
whether the maternity homes provide a safe deliv- 10 maternity homes in Norway are located in the
ery service for women in labor. We report the re- north of the country where the population density
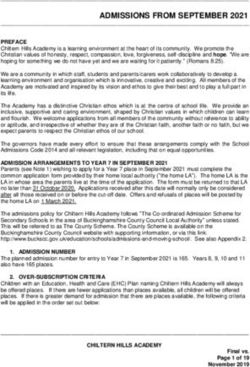
sults from a 2-year prospective study including all is quite low (Fig. 1). The size of the three north-
pregnant women admitted for birth (i.e. all births ernmost counties is 115 000 km2 (35% of Norway,
and all women and newborns transferred to hospi- and approximately three times larger than
tal intra partum or the first week post partum) at Denmark) and the number of annual births is ap-
all maternity homes in Norway. proximately 7000 (12% of all births in Norway).
Fig. 1. Localization of the 10 maternity homes and regional hospitals (indicated by capital letters) in Norway.
C Acta Obstet Gynecol Scand 81 (2002)Deliveries in maternity homes 733
Some characteristics of the maternity homes are At some of the maternity homes, low-risk primip-
given in Table I. arous women are allowed to give birth. Six of the
The distance between the maternity homes and 10 maternity homes have a cardiotocograph
the nearest hospital varies from 70 to 250 km, al- (CTG), used mainly for door step CTG.
though distance is not a good indicator of trans- Traditionally, obstetricians in hospitals have
port time because of ferry crossings and mountain shown little interest in the activity of maternity
passes in some instances. The transport time by homes. Among the 10 maternity homes in full op-
ambulance varies between 2 and 3 h (Table I). All eration, five have regular visits from specialists in
the maternity homes except one use airplanes or obstetrics. These visits vary from once a week to
helicopters in emergency situations, reducing the 3–4 times a year. The specialists usually perform a
transport time to approximately 1 h. regular ultrasound examination at 18 weeks and
Most of the maternity homes are part of a com- out-patient treatment.
munity health service center. The chief GP has the
formal responsibility for running the maternity Materials and methods
homes. In another study we found that GPs are
involved in organizing the work, but participate We analyzed data from deliveries registered at
very little in daily labor care. They are called in to every maternity home in Norway in the 2 years be-
4.6% of all birth at maternity homes, for reasons tween 15 June 1995 and 14 June 1997. The follow-
such as fetal distress, hemorrhage and large peri- ing pregnancies and deliveries were registered: all
neal tears (7). The GPs routinely examine the new- women accepted for birth and admitted at the mat-
borns in the maternity homes. ernity homes, i.e. those with intention to deliver.
Midwifes and GPs in collaboration provide This includes those who delivered there and those
antenatal care. In a normal pregnancy, the woman who were transferred to hospital during labor, and
would attend approximately 12 times. Midwives those who gave birth (unplanned) at a maternity
are responsible for the majority, whereas GPs have home. The main reasons were bad weather con-
3–4 consultations. Midwives are responsible for ditions or an increased risk of a birth in transit. We
monitoring deliveries in maternity homes, and they report the outcome for those women or newborns
also accompany laboring women to hospital. All transferred to hospital within the first week after
maternity homes except one offer postnatal care delivery. Data on accidental out-of-hospitals births
for women who have delivered in an obstetric unit. near maternity homes were registered (Table II).
During the pregnancy there is a continuous selec- The study excluded the following:
tion process for the women who plan their deliver-
ies at the maternity home. The midwife makes the 1) Laboring women who came to the maternity
final decision when the woman in labor arrives at home to be examined before transport to a
the maternity home. The following criteria recom- planned birth in hospital
mended by the Norwegian health authorities (8) 2) Women not accepted for birth at arrival at the
have to be met: maternity home, such as women with a breech
presentation
1) At least one previous normal delivery
2) Delivery between 37 and 42 weeks gestation The study has a descriptive research design. A
3) Actual pregnancy is uncomplicated, and a nor- questionnaire consisting mainly of closed ques-
mal delivery is expected tions was designed and filled out for every birth.
Table I. Some characteristics of all maternity homes in Norway
Maternity home No. of beds No. of deliveries Distance to the Travel time to the nearest
(arbitrary) in the study period nearest hospital (km) hospital by ambulance (h)
1 3 59 150 2
2 4 258 145 2
3 8 202 70 3
4 7 284 170 2
5 6 102 100 3
6 2 43 165 2
7 2 24 120 2
8 5 115 230 3
9 2 17 240 3.5
10 6 101 100 2
C Acta Obstet Gynecol Scand 81 (2002)734 N. Schmidt et al.
Table II. Data on births from maternity homes for those transferred to an obstetric department and for accidental out-of-hospital births near the maternity homes
Admitted to birth in the maternity home (nΩ999)
During transportation
Planned (nΩ999) Unplanned (n218) Transferals (n58) or unplanned at home (n40)
n % n % n % n %
Spontaneous delivery 992 99.3 215 98.6 40 69.9 40 100.0
Forceps 0 0.0 1 0.5 2 3.5 0 0.0
Vacuum extraction 7 0.7 2 0.9 6 10.3 0 0.0
Cesarean section 0 0.0 0 0.0 10 17.2 0 0.0
Apgar score ⬍ 7 at 5 min 5 0.5 0 0.0 1 1.7 2 5.0
Blood loss Ω 500 mL 65 6.5 18 8.3 1 1.7 1 2.5
Primipara 94 9.4 45 20.6 21 36.2 5 12.5
Median birth weight 3640 g 3610 g 3495 g 3420 g
Range 2260–5200 2040–5240 2670–4860 2500–5060
The registration also includes information for and 1 after 10 min. The baby was transferred to
those women transferred intra partum or in the a hospital immediately but died after 4 days. An
post partum period to a hospital (Table II). Regis- autopsy showed massive signs of infection. The
tration was performed immediately after each de- other mother had a normal first and second stage
livery, and was updated 1 week after delivery by the of labor and therefore the low Apgar score of 2
midwife responsible for the birth. Data collection after 1 and again after 5 min was unexpected. This
was anonymous. baby was also transported to hospital but died the
The data were analyzed using descriptive statisti- next day (birth weight 4175 g). Again, an autopsy
cal methods such as frequency distributions and showed massive signs of infection.
measurements for central tendency and variation. Of the 1217 women who gave birth in the mat-
Data handling was carried out using SPSS version ernity homes, 139 (11.4%) were primigravidas
9.0 (9). (Table II). Ninety-four (68%) of these were ac-
cepted for birth at the maternity homes, while the
remaining 45 (32%) delivered there for various rea-
Results
sons, such as rapid progress or difficult weather
During the 2-year study period there were approxi- conditions for transport.
mately 3800 pregnant women in the catchment The median birth weight among the babies born
areas of the maternity homes. Of these women, in the maternity homes was 3640 g (2040–5240 g).
1275 (33.6%) started labor in a maternity home Ten babies (0.8%) had a birth weight of less than
in Norway, which accounts for 1% of all births in 2500 g and 50 (4.1%) babies had a birth weight
Norway during this period. Of the 1275 women, over 4500 g. Six babies (0.5%) were small for ges-
1217 (95.5%) gave birth at the maternity homes tational age. All were planned to take place in the
and 58 (4.5%) were transferred to central hospitals maternity home, and none needed any further
during labor. Additionally, 40 women had their de- treatment or were transferred to hospital after
liveries registered at the maternity homes, but had birth.
accidental out-of-hospital-births during transport
between their homes and hospital (18), while at Apgar scores
home waiting for the ambulance and midwife (19),
or in a smaller health institution without a matern- Twenty-seven (2.2%) of the newborns had an Ap-
ity home (3). gar score below 7 after 1 min, 5 (0.4%) after 5 min,
and 3 (0.2%) after 10 min. One newborn had
multiple malformations, and the two other new-
Deliveries in the maternity homes
born were those who died.
There were two (0.2%) early neonatal deaths in two
different maternity homes. Both babies were born Operative vaginal delivery at maternity homes
with a group B streptococcal infection. Neither of
the mothers had any sign of intrauterine infection. Nine women had a vacuum extraction (Table II).
One gave birth immediately after admission; no fe- Seven of these deliveries were planned to take place
tal heart rate was heard at the time. The birth in the maternity home. One woman had a forceps
weight was 2310 g. Apgar score was 0 after 1 min delivery. This delivery was not planned but trans-
C Acta Obstet Gynecol Scand 81 (2002)Deliveries in maternity homes 735
port to hospital was not possible because of mation and suspected infection, was the reason for
stormy weather. Three women (0.2%) had a va- 36 (63.2%) of the transferals. In one case the trans-
ginal breech delivery. The breech presentations feral occurred because of problems with both the
were not diagnosed before arrival at the maternity mother (a third-degree tear) and the baby (slight
home and they were too far in labor for transport. breathing problems).
All three were uncomplicated deliveries. Midwives
performed most of the operative deliveries, with Discussion
only three being delivered by GPs.
The majority of women in Norway, as in many
European countries, do not have a choice regard-
Hemorrhage
ing their place of delivery: 98% of all deliveries in
A blood loss of less than 500 ml was observed in Norway are in hospital (10), and the remainder are
1114 women (91.5%), and 102 (8.4%) had a blood divided between home (0.6%), during transport
loss between 500 and 1000 ml. One woman (0.1%) (0.3%) or in a maternity home (1.1%).
lost 1500 ml of blood and was transferred to the We have studied a ‘selection’ in those parts of
obstetric unit of the county hospital after delivery. the country where women do have a choice be-
She received two units of blood and was dis- tween a maternity home and a hospital. Identify-
charged the next day. ing a low-risk population is a process that starts
early in pregnancy and ends on admission in the
maternity home when the woman is in labor. Ap-
Transferal to an obstetric department during labor
proximately 35% of the women in the catchment
Fifty-eight (4.5%) women were transferred to an area of the maternity homes delivered in the mat-
obstetric department during labor because of : ernity homes. A few of these underwent operative
deliveries (1%), and a few babies had a low Apgar
1) Prolonged rupture of membranes (over 24 h score (0.4% had Apgar score ⬍7 after 5 min). Only
without established labor) (15 women) 4.5% of the women had to be transferred to hospi-
2) Prolonged first stage of labor (14 women) tal during labor. Of those transferred to hospital
3) Unstable fetal heart rate or other signs of poss- 31% had an operative delivery, but the Apgar
ible fetal distress (thick meconium) (eight scores were satisfactory, indicating that none had
women) long periods of asphyxia during transport. The
4) Unstable lie (four women) two neonatal deaths are probably not related to
5) Maternal need for more pain relief (epidural) birth at the maternity home. Within the first week
(three women) after delivery, 4.7% of the women and/or newborns
6) Bleeding (three women) were transferred from the maternity home to hos-
7) Other reasons (11 women) pital.
The debate on the place of delivery and its safety
Of these women 40 (69.0%) had a spontaneous de- is not new, but has intensified in Norway with the
livery, including one birth during air transport; the publication of a policy document (11). The Nor-
others had operative deliveries as indicated in wegian Board of Health suggests birth institutions
Table II. at three different levels:
The median birth weight among the transferals
was 3495 g (2670–4860 g). After 1 min, three babies 1) Level 1 is hospitals with more than 1500 deliv-
had an Apgar score below 7. One baby had an eries per year with obstetric, pediatric and anes-
Apgar score of 5 and 7 at 5 and 10 min, respec- thetic departments with doctors on duty all the
tively. The remaining babies had Apgar scores of 9 time
or 10 after 5 min. There were no neonatal deaths 2) Level 2 is hospitals with 500–1500 deliveries per
among those transferred. year and with one obstetrician and one anesthe-
tist on call duty
3) Level 3 is maternity homes. It is suggested that
Transferals to hospital after birth
maternity units in institutions with less than 4–
In 57 (4.4%) cases mother and baby were trans- 500 deliveries per year should be called matern-
ferred to hospital after birth, mainly because of ity homes
minor complications. In 20 (35.1%) of these the
transferal was because of problems related to the This splitting into three levels was recently (June
mother. Four (0.3%) of the 1217 women had a 2001) confirmed by the Norwegian parliament
third-degree anal sphincter tear. The babies’ health (Stortinget). At present, several small obstetric de-
condition, such as jaundice, congenital malfor- partments have less then 500 deliveries per year
C Acta Obstet Gynecol Scand 81 (2002)736 N. Schmidt et al.
(11). If a cut-off level of 450 deliveries per year is sainen et al. (17) but was based on a register study.
accepted by politicians, 17 of the smallest obstetric In our study, the women were followed prospec-
departments should be closed down (centralized) tively and comprise a substantial fraction of all
or transformed to maternity homes (presently pregnant women in the catchment areas.
covering 5000 deliveries or 8% of the births in Nor- Recently, an analysis from the Medical Birth
way). We believe that there is a place for maternity Registry of Norway was published showing that
homes in Norway in the future. during a 25-year period the relative risk of neo-
In the study period, 1% of all births in maternity natal death in low-risk pregnancies was 2.1%
homes in Norway resulted in an uncomplicated higher (95% confidence interval 1.6–2.8) for mat-
vacuum or forceps delivery, while the total operat- ernity units with less than 100 births per year com-
ive delivery rate in Norway is approximately 20% pared with units with 2000–3000 deliveries (18).
(10). Many small hospitals in Norway, with less Almost a similar increase in relative risk for neo-
then 500 deliveries per year, that are supposed to natal death was observed for units with more than
only admit low-risk pregnancies have 20–30% of 3000 deliveries per year. As with all retrospective
operative deliveries. We find it difficult to under- analyses, the interpretation of these results is dif-
stand why such a high operative delivery level is ficult. The groups studied were not comparable,
necessary, although these institutions are not di- there has been no attempt to classify the neonatal
rectly comparable to the maternity homes in this deaths as possible avoidable or unavoidable, and
study. information on risk factors is uncertain. The single
Most would agree that close supervision and page form sent to the Medical Birth Registry for
monitoring of high-risk pregnancies is beneficial, every birth in Norway has only one open line to
and that women with complicated pregnancies are be completed for chronic diseases or complications
best cared for in large and well-equipped medical during pregnancy, and the information given has
centers. However, the application of the same cri- never been validated.
teria to low-risk pregnancies has been questioned. The selection process made by midwives and
There is some evidence to suggest that there is GPs seems to identify a low-risk population that
more intervention in labor and higher maternal can deliver safely at the maternity homes in Nor-
morbidity if a low-risk woman is cared for in an way. We believe that obstetric departments could
obstetric department than in a maternity home have something to learn in identifying and han-
(12). Obstetric departments that have high cesar- dling a low-risk population. For pregnant women
ean section rates among high-risk pregnancies also in rural areas there would be three alternatives in
have high cesarean section rates for ‘normal’ the future labor care system. The first is that to-
primipara (13). day’s practice continues: healthy pregnant women
There are few studies from developed countries can give birth at maternity homes near their homes
reporting results from births outside central hospi- with a 4–5% risk of needing transfer during labor.
tals. In New Zealand, a country with many simi- A second alternative would be that women stay at
larities to Norway, decentralized birth is common, home until labor begins and are then transported
and they report good results from institutions or- to the nearest consultant unit, a trip of 2–3 h. This
ganized in the same way as our maternity homes would imply that nearly every woman would be
(14). There may, however, be biases, as transfers travelling while in labor. A third alternative would
between hospitals are not evaluated as in our re- be that all women travel to the consultant unit 2–
port. In the Netherlands approximately 30% of all 3 weeks before they are due, and await the onset
births are home births (15), but the difference in of labor. In this scenario a woman may then risk
population density and geography make their re- being away from her family for up to 5 weeks.
sults somewhat incomparable to Norwegian Whether a decentralized birth organization should
studies. However, transfers during labor in 5% of be offered to a low-risk population is in our opin-
cases, as in our study, is lower than reported from ion more of a political question than a medical
midwife-managed delivery units within hospitals in problem.
the UK and in the Netherlands (12, 15). This is
probably because of a more rigid selection process.
Acknowledgments
Rooks et al. (16) have demonstrated the safety and
low intervention rates at free standing birth clinics We wish to thank the midwives at all the maternity homes that
in a very large US sample. However, the women helped us with this study.
were highly selected and did not comprise as large
a proportion of all women as in our study. The References
safety of well-selected births at small units in re-
mote areas has previously been indicated by Vii- 1. Bergsjø P, Daltveit AK. Fødeinstitusjoner og fødsler i nor-
C Acta Obstet Gynecol Scand 81 (2002)Deliveries in maternity homes 737
ske fylker i begynnelsen av 1990-årene. [Birth Institutions ities, equipment and staff)]. Oslo: The Norwegian Board of
Births Counties Norway Early 1990 (In Norwegian with Health. Number 1, 1997.
English abstract.) Tidsskr Nor Lægeforen 1996; 116: 1591– 12. Hundley VA, Cruickshank FM, Lang GD et al. Midwife
4. managed delivery unit: a randomised controlled compari-
2. Kamper-Jørgensen F, Bakketeig L, Bergsjø P, Biering G, son with consultant led care. Br J Obstet Gynaecol 1994;
Hartikainen-Sorri A-L, Larsen JF et al. Perinatal omsorg i 309: 1400–4.
de nordiske lande-svangrekontrol, føde-og neonatalordn- 13. Cleary R, Beard RW, Chapple J et al. The standard primi-
inger. [Perinatal care in the Nordic countries. Prenatal, para as a basis for inter-unit comparisons of maternity
birth and neonatal care organisation] (in Norwegian, care. Br J Obstet Gynaecol 1996; 103: 223–9.
Danish and Swedish.) Copenhagen: DIKE, 1986. 14. Rosenblatt RA, Reinken J, Shoemack P. Is obstetrics safe in
3. House of Commons Social Services Committee on Peri- small hospitals? Evidence from New Zealand’s regionalised
natal and Neonatal Mortality. Second Report. London: perinatal system. Lancet 1985; ii: 429–32.
HMSO, 1980. 15. Eskes TKAB. Home deliveries in the Netherlands – Peri-
4. Tew M. Place of birth and perinatal mortality. J R Coll natal mortality and morbidity. Int J Gynecol Obstet 1992;
Gen Pract 1985; 35: 390–4. 38: 161–9.
5. Anonymous. What future for small obstetric units? Lancet 16. Rooks JP, Weatherby NL, Ernst EKM, Stapleton S, Rosen
1985; ii: 423–4. D, Rosenfield A. Outcomes of care in birth centers. N Engl
6. House of Commons Health Committee on Maternity Ser- J Med 1989; 321: 1804–11.
vices. Second report for the session 1991–2. London: 17. Viisainen K, Gissler M, Hemminki E. Birth outcome by
HMSO, 1992. level of obstetric care in Finland: a catchment area based
7. Schmidt N, Abelsen B, Eide B, Øian P. Fødestuer i Norge analysis. J Epidemiol Community Health 1994; 48: 400–5.
[Maternity homes in Norway]. (In Norwegian, English 18. Moster D, Lie RT, Markestad T. Relation between size of
summary). Tidsskr Nor Lægeforen 1997; 117: 823–6. delivery unit and neonatal death in low risk deliveries:
8. Sosialdepartementet. Perinatal omsorg i Norge [Depart- population based study. Arch Dis Child Fetal Neonatal Ed
ment of social affairs: Perinatal care in Norway]. Norges 1999; 80: 221–5.
Offentlige Utredninger (NOU). Oslo Universitetsforlaget,
1984: 17.
9. The Statistical Package for Social Sciences. SPSS for Win- Address for correspondence:
dows. Version 9.0. Chicago: SPSS Inc., 1999. Prof. Pål Øian
10. Medisinsk fødselsregister. Årsrapport 1997. [Annual Re- Department of Obstetrics and Gynecology
port. Medical Birth Registry of Norway]. Bergen, Norway, University Hospital
1997. N-9038 Tromsø
11. Statens helsetilsyn. Faglige krav til fødeinstitujoner [Pro- Norway
fessional standards for maternity care in institutions (local- e-mail: paaloian/online.no
C Acta Obstet Gynecol Scand 81 (2002)Copyright of Acta Obstetricia et Gynecologica Scandinavica is the property of Wiley-Blackwell and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
You can also read