The Nightingale Exeter Story - Devon's Phoenix from the Flames
←
→
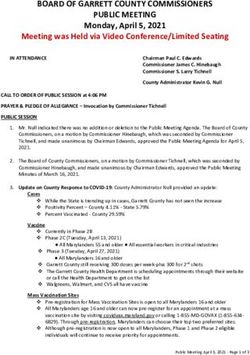
Page content transcription
If your browser does not render page correctly, please read the page content below
UK’s response to a global
pandemic – 24th March 2020
“This will be a model of care never needed or seen before in this country, but our specialist doctors are in touch with their counterparts
internationally who are also opening facilities like this, in response to the shared global pandemic”
- NHS chief executive Sir Simon StevensBackground of Nightingale Hospitals:
• 24/03/2020: 4000 Critical Care Beds – Response to images coming from Italy
• 1 Month later: Announcement that final 2 hospitals of 7 Nightingale hospital to
inc Exeter
But what had we been learning and what do we need to do now?This
To
What changed ?
• Clinical model was changing
• Nightingales had offered little in the way of flexibility of care
• Hospitals were becoming over stretched by ward acuity
COVID: 10-15% required ITU or HDU levels of care.
• Westpoint conference centre was probably too large and was
only available until March 2021- we decided to move to a
smaller facility which offered an opportunity for long term
use- a former Homebase storeChallenges of System Working
• The Nightingale Exeter was commissioned as a system asset to Devon and the wider South West. We
were given 6 weeks!
• RD&E were happy to host the facility but wanted to share the responsibility around commissioning
and staffing the unit. But there were obvious tensions;
– Rapid decision making from a System led team versus normal governance
– RD&E Board were the legal entity accountable for a safe building and for patient care / CQC
– A fear that RDE would be left with diluted staffing at its base hospital or residual costs
Handling – Gold and Silver Teams
• Gold team were strategic directors from the wider Devon system to commission the NHE, with a robust
clinical model ensuring clear patient criteria, fair access and fair contribution of staffing/funding.
• Silver team were operationally focussed and would manage the unit – sign off of design / SOPs / staffing
levels. Ended up being RDE based which provided confidence.
• Assurance to RDE Board managed separately by RDE Deputy CEO based on a scheme of delegation and
external assurance via NHSE scrutiny.
• Inevitable tensions around the choice of site, speed, cost, risk management and who was accountable to
NHSE/DH – but we managed it by using a number of agreed team working principles.Commissioning and Stand-by
National Clinical and Estates approval finally achieved : 6th July 2020
( 4 weeks later than planned due to change of site and more complex design)
Q - How could the Nightingale best now help
Support our NHS ?
(Devon ICS consistently record < 5 COVID Inpatients)
13th July 2020 – First diagnostic list
c.4000 diagnostic scans
c.600 Novavax COVID vaccine trails
c.100 oversea nurses re validation course completedJuly – November 2021
Standby & preparation for the second wave
All Nightingales faced 2 fundamental challenges:
1. Staffing
2. Clinical safety at a remote site with limited facilities
Most clinicians had a preference to retain patients at the base site rather than
dilute staffing levels and did not expect the Nightingale to be used.Staffing • Ward-based structure • A wide recruitment drive • Training days for all volunteers, on site • Webinars and updates → Enough staff to form a core on which to build • Challenges: COVID had gone, staff could not be released, no certainty they would come when called
Clinical Planning
Patients would only be transferred to NHE if their care and
treatment would at least match that which they would have
received in their base hospital
• Clinical plans had informed the design
• Staff, expertise, equipment on site, protocols
• Transfer
• Contingency planning (what if?)
• Engagement with referring clinicians and hospitals
• IT
• Relationship with host trust (RD&E)Stand-up: November 2020
The surge in admissions led to a request to mobilise – this needed a
strong case to NHSE/DH as it was the only Nightingale to be used for
COVID
April NovemberNov 26th 2020 – Feb 24th 2021
• 247 admissions,
• Transferred from 8 hospitals (Devon, Somerset and Dorset)
• 37 deaths (average age 85 years, range 72 – 99)
• Maximum bed occupancy 62, 3 wards
(Total beds 116 on 5 wards)
• Non-invasive ventilation, no invasive ventilation (ie not full ITU)
• 4 patients required emergency transfer back into a main hospitalNHE Bed Occupancy
MPH Dorset
RDE RDE
UHP
ND
TSD Yeovil
50
Nov Jan Feb
26th 29th 24thCOVID at NHE: summary • We had a superb facility and a convergence of extraordinary motivation and expertise – showed system working at its best • We had planned well but were also lucky – Time to plan, recruit and train before the second wave struck – The region’s hospitals were pressured at different times – We had superb team, clinical and non-clinical • NHE provided good clinical care and important support to the wider region • The least expensive Nightingale Hospital and one that was used • A potential legacy for future recovery
Purchase and Options post COVID • All Nightingales needed to be decommissioned - DH funding set aside • With support from Regional colleagues, this funding was re-purposed to enable purchase. • Created interesting accounting questions as to whether costs were revenue or capital, and also how to treat the impairment on valuing the asset. • Underwriting of Ongoing Revenue Costs - RDE Board needed assurance from system. • The Devon ICS re-established a Programme Board and commissioned an options appraisal as to the future use.
Devon’s Accelerator Pilot: Testing the future model of care
Waiting times for elective care ? March 2021 – c.5 million patients awaiting treatment with 10% waiting > 52 weeks. Orthopaedics and ophthalmology have the largest national waiting lists (620,000 and 512,000) Nightingale perfect opportunity to host an Accelerator Pilot: Aim was to deliver activity at 120% of 19/20 level by July 2020 Twin bid made in concert with UHP modular theatres. Devon requested that the £11.3m of funding on offer was converted into capital, to create capacity for • Orthopaedic • Ophthalmology • Diagnostics
A System Catalyst
• Opportunity for innovation and partnership
Standardise best in class clinical pathways ( GIRFT)
Test of Change for Protected Elective Care Unit
Submissions to NHSX for digital enhancements
Integrated digital sharing across the Devon ICS
‘Surgicube’ virtual ophthalmic theatre
Managed Equipment Services
• System test of change driven by enthusiastic clinical
engagement- had to move quickly so a bit bumpy at first!Orthopaedic Accelerator Facility
• Restoration of elective work / waiting list recovery / winter capacity
• Centre for proof of concept
– System facility for elective care /Collaborative working of four Trusts
– Working patterns
– Standardised pathways for patient selection, prehabilitation, preadmission,
anaesthetic, discharge and recovery
• Centre for test of change
– Short stay hip and knee replacement, and spinal surgery
– Digitising the “lifetime” patient pathway and putting patients in control
• Lifestyle, prevention and health optimisation
• Shared decision making / patient education
• Pre-operative assessment and preparation
• Hospital episode / integration with EPR
• Recovery and optimisationSpecialist Outpatient:
High Flow / Low Complexity
Rheumatology
Ophthalmology:
• Optimising
• High flow cataract surgery
operational capacity
using innovative SurgiCube
• Consolidation to
(50% + list efficiencies)
single site / template
• 2 high flow diagnostic and
• Increased throughput
data acquisition with virtual
through co-location
reporting (on or off site)
Community Diagnostic Hub:
(Year 1 - Accelerator Site)
• Richard’s Report
• Increased elective diagnostic provision
• Developing one-stop pathways
(complimenting Rheumatology and Orthopaedics)
• Year 2 – 5 expansion of Hub
• Incorporating diagnostic AI
developments and innovation
Co-location of complimentary services to create
efficiencies, shared resource and hub for innovationThe Nightingale Exeter has been an incredible experience for so many
staff & contractors across Devon
Our challenge is now to provide a legacy for future generationsYou can also read