Primary Adrenal Lymphoma - A Rare Entity with Grave Prognosis
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Primary Adrenal Lymphoma Case Analyses
Primary Adrenal Lymphoma - A Rare Entity with
Grave Prognosis
Chen-Hsun Ho,1,2 Shih-Chieh Chueh,1 Yeong-Shiau Pu,1 Shyh-Chyan Chen,1 Hong-Jeng Yu,1
Kuo-How Huang1
1
Department of Urology, National Taiwan University Hospital, Taipei, Taiwan
2
Division of Urology, Department of Surgery, Buddhist Tzu Chi General Hospital, Taipei Branch, Taipei, Taiwan
Purpose: Primary adrenal lymphoma is extremely rare. We analyzed our cases to further illustrate the clinical charac-
teristics of this rare disease.
Methods: In the past 10 years, there have been three patients diagnosed as primary adrenal lymphoma in our institution.
There have been another three patients with secondary adrenal lymphoma, involving not only the adrenal glands but
also other organs or lymph nodes. The clinical and pathological characteristics of the six cases were compared and
analyzed.
Results: The three cases of primary adrenal lymphoma were characterized with old age, male-predominance, bilateral
adrenal involvement, adrenal insufficiency, and histological type of diffuse large B-cell lymphoma. All of them received
chemotherapy but died within half year of diagnosis: one died of disease progression; the other two died of complications.
The three cases of secondary adrenal lymphoma were relatively young. All had unilateral adrenal involvement and no
adrenal insufficiency. The pathological examinations revealed diffuse large B-cell lymphoma. The prognosis was better:
two of them have been disease-free after treatment; the other died of disease progression.
Conclusions: Primary adrenal lymphoma is extremely rare. It predominantly affects the elderly and men, mostly in-
volves the bilateral adrenal glands, and usually causes adrenal insufficiency. The majority of the cases are of diffuse large
B-cell lymphoma. The prognosis is poor, and most patients die within one year of diagnosis. With very limited experience,
the optimal therapeutic strategy remained unclear and required further studies. It is important to differentiate between
primary and secondary adrenal lymphoma since the clinical course is extremely different.(JTUA 20:168-72, 2009)
Key words: Adrenal, lymphoma, non-Hodgkin's, diffuse large B-cell.
INTRODUCTION patients, six patients presented with adrenal tumors
initially. Three of them had adrenal glands involvement
It has been reported that up to 25 percent of non- exclusively and were diagnosed as primary adrenal
Hodgkin's lymphoma has adrenal glands involvement lymphoma; the other three patients had not only adrenal
on autopsy.1 In contrast, primary adrenal lymphoma, glands but also other lymph nodes or organs involve-
defined as malignant neoplastic proliferation of the lym- ment, which were diagnosed as secondary adrenal
phoid cells exclusively in the adrenal glands, is very rare. lymphoma. We illustrated and analyzed the six cases
To date, there have been only about 100 cases in the with an effort to clarify the clinical and pathological fea-
literature review.2-15 The hypothesis for the origin of these tures of primary adrenal lymphoma.
tumors is hematopoietic tissue rests in the adrenal gland.
With very limited experience, we know little about the PATIENTS AND METHODS
clinical characteristics of this disease.
In the past 10 years, there have been 1,670 patients Between January 1996 and December 2006, a total
with non-Hodgkin lymphoma in our institution. Of these of 1,670 patients were diagnosed as non-Hodgkin lym-
phoma and received treatment in our institution. Among
them, 846 patients were of diffuse large B-cell
Address reprint requests and correspondence to:
Kuo-How Huang, M.D. lymphoma. The ratio of male to female was 1.3. The
Department of Urology, College of Medicine, National Taiwan mean age was 55 ± 18.7 years. Six patients initially pre-
University, No. 7, Chung-Shan South Road, Taipei, Taiwan 100 sented with adrenal tumors. Three of the six patients
TEL: +886-2-23123456#65952 FAX: +886-2-23219145
Email: khhuang123@ntu.edu.tw were diagnosed as primary adrenal lymphoma, and the
NSU JTUA 2009 20 No. 4C. H. Ho, et al
other three patients were diagnosed as secondary adre- the diagnosis.
nal lymphoma. The medical records of the six patients Patient 2 received chemotherapy with two cycles of
were analyzed retrospectively. The age, gender, clinical BOMES (BCNU, vincristine, methotrexate, etoposide,
presentations, pathological characteristics, and progno- and methylprednisolone). The treatment was compli-
sis were illustrated and analyzed. cated by febrile neutropenia, and he died of sepsis three
The diagnosis of primary adrenal lymphoma was months after the diagnosis. Patient 3 was treated with
made by pathologically confirmed lymphoma in the ad- two cycles of R-COP (rituximab, cyclophosphamide,
renal glands without evidence of other organs or lymph vincristine, and prednisone). The treatment was also
nodes involvement. If there was involvement of other complicated by neutropenic fever, and he died of sepsis
lymph nodes or organs, it was classified as secondary two months after the diagnosis.
adrenal lymphoma.
Secondary adrenal lymphoma
RESULTS
During the same period, we had another three pa-
Primary adrenal lymphoma tients presenting with retroperitoneal lymphoma with
involvement of the adrenal glands (Patient 4, 5, and 6).
Between January 1996 and December 2006, a total The clinicopathological characteristics were shown in
of three patients were diagnosed with primary adrenal Table 1. The three patients had distinct clinical courses
lymphoma in our institution. The clinicopathological and outcomes.
characteristics of the three patients (Patient 1, 2, and 3) The ages at diagnosis were 48, 25, and 76 respe-
with primary adrenal lymphoma were listed in Table 1. ctively. All the three patients were male in gender. The
The age at diagnosis was 79, 60, and 79 respectively. initial presentations were fever (Patient 4) and abdomi-
All the three patients were male in gender. nal pain (Patient 5). Patient 6 was asymptomatic and
The initial presentations included several constitu- was found to have an adrenal tumor incidentally. On
tional symptoms: anorexia, poor appetite, body weight CT, the adrenal tumor was homogenous and hypodense
loss, and fever. All of them had involvement of bilateral in Patient 4; it was heterogenous and hypodense in Pa-
adrenal glands exclusively. The three patients all had tient 5. The angiography of Patient 5 demonstrated a
adrenal insufficiency. All the 3 patients had no leuke- hypervascular tumor. On the magnetic resonance imag-
mic pictures in complete blood count or bone marrow. ing (MRI), the tumor of Patient 6 was of high signal-
For making a diagnosis, two of them underwent unilat- intensity in T2-weighted images and low signal-inten-
eral adrenalectomy (Patient 1 and 2), while the other sity in T1-weighted images. The diagnostic procedures
(Patient 3) one received CT-guided biopsy. On the com- included adrenalectomy in Patient 4 and 5, and CT-
puted tomography (CT), the lesions were either heter- guided biopsy without further surgery in Patient 6. All
ogenous (Patient 1 and 2) or homogenous (Patient 3); the pathological examinations revealed diffuse large B-
all were hypodense. Grossly, the tumors were white-gray cell lymphoma.
and partially necrotic. The pathological findings were similar to the group
The pathological examinations revealed malignant of primary adrenal lymphoma. The patient 4 had dis-
lymphoid cells with increased mitosis infiltrated and ease at the left adrenal gland and lymph nodes in the
replaced the adrenal medullary and cortical tissue. Based mediastinum and the retroperitoneum. He received four
on the immunostatining, all the three cases were diffuse cycle of CHOP and another one cycle of ESHAP
large B-cell lymphoma. (etoposide, methylprednisolone, cytarabine, and
The clinical course of Patient 1 was characterized cisplatin). He died of disease progression six months
by persistent disease progression and treatment failure. after the diagnosis.
The chemotherapy regimen included one cycle of COP The patient 5 had disease involving the right adre-
(cyclophosphamide, vincristine, and prednisolone), two nal gland, right kidney, right psoas muscle, and right
cycles of COP with bleomycin, one cycle of CNOP retroperitoneal lymph nodes. He underwent radical sur-
(cyclophosphamide, mitoxantrone, vincristine, and gery including adrenalectomy, nephrectomy,
prednisolone), one cycle of EPOCN (etoposide, lymphadenectomy, and excision of the involved psoas
prednisolone, vincristine, cyclophosphamide, and muscle 10 years ago. Postoperatively, he received eight
mitoxantrone). Rituximab (anti-CD20 monoclonal courses of CHOP (cyclophosphamide, doxorubicin,
antibody) was also prescribed after chemotherapy failed. vincristine, and prednisone). He had been disease-free
Patient 1 died of disease progression five months after for four years before recurrence at the para-aortic lymph
JTUA 2009 20 No. 4 NSVPrimary Adrenal Lymphoma
nodes. He then received one cycle of ESHAP and two stem cells transplantation). He has been disease-free
cycles of BOMES. He then received high-dose BEAM thereafter and is still alive.
chemotherapy (BCNU, etoposide, cytarabine, and Patient 6 had disease involving the right adrenal
melphalan) and autologous PBSCT (peripheral blood
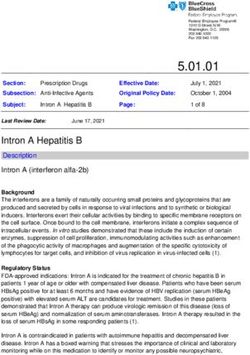
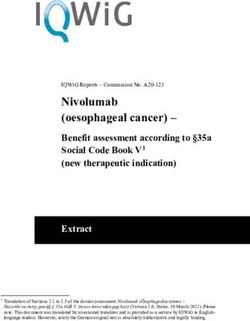
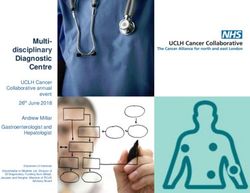
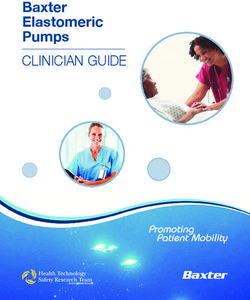
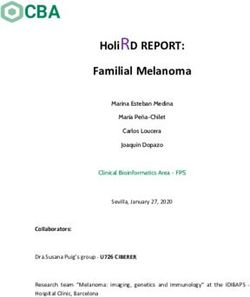
Table 1. Clinicopathological characteristics of the six patients with adrenal lymphoma
Patient #1 #2 #3 #4 #5 #6
Adrenal Lymphoma Primary Primary Primary Secondary Secondary Secondary
Age at diagnosis 79 60 79 48 25 76
Gender M M M M M M
Adrenal laterality Bilateral Bilateral Bilateral Left Right Right
Disease involvement Bilateral adrenal Bilateral adrenal Bilateral adrenal Left adrenal Right adrenal Right adrenal
glands glands glands gland, paraaortic gland, right gland,
Initial presentations Anorexia, malaise, Fever, anorexia, Anorexia, malaise, Fever Abdominal pain Incidental finding
body weight loss body weight loss body weight loss
Diagnostic Adrenalectomy, Adrenalectomy, CT-guided biopsy, Adrenalectomy, Adrenalectomy, CT-guided biopsy,
procedures left left left left right right
Diagnostic image CT CT CT CT CT, angiography MRI
Image findings Left adrenal gland: Right adrenal mass: Right adrenal mass: Left adrenal mass: Right adrenal mass: Right adrenal
10×8 cm, Right 8×5 cm; 4.8×2.5 cm; 3×3 cm, 5×6 cm, mass: 7×5 cm,
adrenal gland: Left adrenal mass: Left adrenal mass: homogenous, heterogenous, high signal intensity
2×3 cm, 6×5 cm, 5×2.8 cm, hypodense hypodense, in T2W image;
heterogenous, heterogenous, homogenous, hypervascular low signal intensity
hypodense hypodense hypodense in T1W image
Leukemic pictures (-) (-) (-) (-) (-) (-)
Comorbidities Hypetension, atrial No Peptic ulcer Anemia No Peptic ulcer
fibrillation
Pathology DLBCL DLBCL DLBCL DLBCL DLBCL DLBCL
IHC staining CD45 (+) CD45 (+) CD45 (+) CD45 (+) CD45 (+) CD45 (+)
CD20 (+) CD20 (+) CD20 (+) CD20 (+) CD20 (+) CD20 (+)
CD3 (-) CLA (+) CD3 (-) CLA (+) CD3 (-) S-100 (-)
S-100 (-) CD3 (-) CLA(+) c-kit (+) S-100 (-) cytokeratin (-)
cytokeratin (-) NSE (-) CK (-) CD 3(-) cytokeratin (-) NSE (-)
NSE (-) EBER (-) S-100 (-) NSE (-)
CK (-)
Adrenal Insufficiency Yes Yes Yes No No No
Symptoms-to-Diagnosis, 12 3 1 2 5 1
months
Chemotherapy regimens COP (1) BOMES (2) R-COP (2) CHOP (4) CHOP (8) R-CHOP (3)
COP + ESHAP (1) ESHAP (1)
bleomycin (2) BOMES (2)
CNOP (1)
EPOCN (1) High-dose BEAM
Rituximab and Auto-PBSCT
Cause of Death Disease Sepsis (complication Sepsis (complication Disease Alive Alive
progression of treatment) of treatment) progression
Diagnosis-to-Death, 5 3 2 6 120 (alive) 15 (alive)
months
CLA:Common leukocyte antigen, CK: cytokeratin, EBER: Epstein-Barr virus encoded RNA, NSE: neuron specific enolase; COP (cyclophosphamide, vincristin,
and prednisolone), CNOP (cyclophosphamide, mitoxantrone, vincristine, and prednisoloneand), EPOCN (etoposide, prednisolone, vincristine, cyclophospahmide,
and mitoxantrone), BOMES (BCNU, vincristine, methotrexate, etoposide, and methylprednisolone), R-COP (rituximab, cyclophosphamide, vincristine, and prednisone),
ESHAP (etoposide, methylprednisolone, cytarabine, and cisplatin), BEAM (BCNU, etoposide, cytarabine, and melphalan).
NTM JTUA 2009 20 No. 4C. H. Ho, et al
gland and suprarenal lymph nodes. diagnosis.
He received three cycles of rituximab and CHOP. With very limited experience in the literature, the
He had complete remission and has been alive. optimal therapeutic modality is poorly defined. Surgery
is more a diagnostic procedure than a therapeutic
DISCUSSION intention. Long-term survival has been rarely reported
with either adrenalectomy followed by chemotherapy
Primary adrenal lymphoma is an extremely rare or adrenalectomy followed by radiotherapy.13,14 How-
disease. The present study is the largest series in a single ever, the result of either strategy has been disappointing;
institute despite of the small patient numbers. To illus- most patients died of the disease or its complications
trate the distinct clinical presentations and courses of within one year of diagnosis in the literature review.13
primary adrenal lymphoma, we also compared the pri- The choices of treatment modalities should be balanced
mary cases with the secondary cases. The clinical pic- between effects and side effects.
tures of the three cases of primary adrenal lymphoma The prognosis is grave with the survival period less
generally accords with previously published litera- than 5 months in the group of primary adrenal lymphoma.
ture.2-15 Primary adrenal lymphoma predominantly af- All the three cases of primary adrenal lymphoma had
fects the elderly and men.13,14 Wang J et al13 reviewed 55 involvement of the bilateral adrenal glands, and unilat-
cases which had been reported in the literature. The eral adrenalectomy simply meant a diagnostic procedure.
median age was 68 and the male to female ratio was 2.2 It is unclear whether a radical surgery (bilateral adrena-
to 1. Of these patients, 40 (73%) patients had involve- lectomy) combined with chemotherapy can achieve a
ment of bilateral adrenal glands; 20 (36%) had adrenal better survival. In the three patients with secondary ad-
insufficiency. In our series, all the three patients with renal lymphoma, the outcomes were distinctly better in
primary adrenal lymphoma had bilateral involvement comparison with the three primary cases. Even with more
and adrenal insufficiency. extensive involvement, Patient 5 and 6 had a long-term
In the present study, all the three patients with pri- survival after surgery and chemotherapy. It remained
mary adrenal lymphoma had diffuse large B-cell unclear what causes the extremely different courses be-
lymphoma, concurring with the report of Wang J et al13, tween primary and secondary adrenal lymphoma.
in which 71% of the patients had diffuse large B-cell
lymphoma. Other less common histological types in- CONCLUSIONS
cluded mixed large and small cells, small non-cleaved
cells, undifferentiated, and others. The majority of the Primary adrenal lymphoma is very rare. It predomi-
reported cases were of B cell type with only two cases nantly affects the elderly and the men. It tends to in-
of T cell type (2/55). Some studies mentioned that poor volve the bilateral adrenal glands and usually causes
prognostic factors include advanced age, large tumor, adrenal insufficiency. The majority are of diffuse large
the presence of adrenal insufficiency, and a high plasma B-cell type. The outcome is very ominous, and most
LDH level.3,5,8,13,14 In our series, all the patients with pri- patients die of disease progression of treatment compli-
mary adrenal lymphoma had a high serum level of LDH, cations within one year of diagnosis. It is prudent to dif-
involvement of bilateral adrenal glands, and adrenal ferentiate between primary and secondary adrenal lym-
insufficiency. The three patients had a distinctly poor phoma since the clinical course is extremely different.
prognosis in comparison with the other three patients Although the secondary cases have a more exten-
with secondary adrenal lymphoma. The cause may be sive disease, the patients have a significantly better
due the distinctly special disease entity or other factors outcome. The treatment modalities for primary adrenal
including older age, larger size of tumor and adrenal lymphoma include surgery, chemotherapy, radiotherapy,
insufficiency, which remained much to be explored in or combinations. With very limited experience, the op-
the future. timal therapeutic strategy remained unclear and required
All the six patients, either with primary or second- further studies.
ary adrenal lymphoma, presented with adrenal tumor
initially. The differential diagnosis included poorly dif- REFERENCES
ferentiated adrenal cortical carcinoma, metastatic
carcinoma, primary or metastatic malignant melanoma 1. Rosenberg SA, Diamond HD, Jaslowitz B, Craver LF.
and malignant pheochromocytoma.6,7,10,13 It is difficult Lymphosarcoma: a review of 1269 cases. Medicine
to make a diagnosis according to the image study. It re- 1961;40:31-84.
2. Bauduer F, Delmer A, Le TA et al. Primary adrenal
quires pathological examinations to make the final lymphoma. Acta Haematol 1992; 88: 213-5.
JTUA 2009 20 No. 4 NTNPrimary Adrenal Lymphoma
3. Feldberg MA, Hendriks MJ, Klinkhamer AC. Massive 10. Kato H, Itami J, Shiina T et al. MR imaging of primary
bilateral non-Hodgkin's lymphomas of the adrenals. Urol. adrenal lymphoma. Clin. Imaging 1996;20:126-8.
Radiol 1986;8:85-8. 11. Sasagawa I, Sadamori N, Itoyama T et al. Primary ad-
4. Harris GJ, Tio FO, Von Hoff DD. Primary adrenal renal lymphoma with chromosomal abnormalities. Acta
lymphoma. Cancer 1989;63:799-803. Haematol. 1995;94:156-62.
5. Lu JY, Chang CC, Chang YL. Adrenal lymphoma and 12. Serrano S, Tejedor L, Garcia B, Hallal H, Polo JA,
Addison's disease: report of a case. J. Formos. Med. Alguacil G. Addisonian crisis as the presenting feature
Assoc 2002;101:854-8. of bilateral primary adrenal lymphoma. Cancer 1993;
6. Zhang LJ, Yang GF, Shen W, Qi J. Imaging of primary 71:4030-3.
adrenal lymphoma: case report and literature review. 13. Wang J, Sun NC, Renslo R et al. Clinically silent pri-
Acta Radiol 2006;47:993-7. mary adrenal lymphoma: a case report and review of
7. Varez-Castells A, Pedraza S, Tallada N, Castella E, Gifre the literature. Am. J. Hematol. 1998;58:130-6.
L, Torrents C. CT of primary bilateral adrenal lymphoma. 14. Wu HC, Shih LY, Chen TC, Chu SH, Tsai CC. A patient
J. Comput. Assist. Tomogr 1993;17:408-9. with bilateral primary adrenal lymphoma, presenting with
8. Choi CH, Durishin M, Garbadawala ST, Richard J. Non- fever of unknown origin and achieving long-term dis-
Hodgkin's lymphoma of the adrenal gland. Arch. Pathol. ease-free survival after resection and chemotherapy.
Lab. Med 1990;114:883-5. Ann. Hematol. 1999;78:289-92.
9. Curry NS, Chung CJ, Potts W, Bissada N. Isolated lym- 15. Ohsawa M, Tomita Y, Hashimoto M, Yasunaga Y, Kanno
phoma of genitourinary tract and adrenals. Urology H, Aozasa K. Malignant lymphoma of the adrenal gland:
1993;41:494-8. its possible correlation with the Epstein-Barr virus. Mod.
Pathol 1996;9:534-43.
NTO JTUA 2009 20 No. 4You can also read