Intraductal Carcinoma of the Prostate
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Intraductal Carcinoma of the Prostate
Brian Robinson, MD; Cristina Magi-Galluzzi, MD, PhD; Ming Zhou, MD, PhD
Na distinct
Context.—Intraductal carcinoma of the prostate (IDC-P) is
clinicopathologic entity, characterized by an expan-
of IDC-P are greatest. Morphologic criteria have been
proposed to distinguish IDC-P from several other lesions
sile proliferation of secretory cells within prostatic ducts and with similar histologic appearance such as high-grade pro-
acini that demonstrate marked architectural and cytologic static intraepithelial neoplasia, invasive cribriform prostate
atypia. Intraductal carcinoma of the prostate is strongly cancer, and urothelial carcinoma involving the prostate.
associated with high-grade and high-volume, invasive pros- Intraductal carcinoma of the prostate is an uncommon
tate cancer and a poorer prognosis than cases without IDC-P. finding in prostate biopsies, and it is even rarer as an
Objective.—To review the historic perspectives, patho- isolated finding without concomitant prostate cancer in
logic and genetic features, diagnostic criteria and differ- biopsies. However, patients with isolated IDC-P in biopsies
ential diagnoses, and the clinical significance of IDC-P. are recommended for either definitive treatment or
Data Sources.—Relevant studies indexed in PubMed. immediate repeat biopsy.
Conclusions.—It is critical to recognize IDC-P, especial- (Arch Pathol Lab Med. 2012;136:418–425; doi: 10.5858/
ly in prostate biopsies in which the clinical implications arpa.2011-0519-RA)
P rostate lesions with cribriform or solid architectures
range from benign and proliferative, such as central
zone glands, clear cell cribriform hyperplasia, and basal
well as the reporting of IDC-P in prostate biopsies is also
discussed.
cell hyperplasia, to invasive cribriform carcinoma. Infre- HISTORIC PERSPECTIVE
quently, cribriform or solid lesions comprise cytologically Although in earlier literature,3 the term intraductal
malignant cells spanning or filling glandular lumens and carcinoma of the prostate has been used variably to describe
yet preserve, at least focally, a basal cell lining. These the extension of prostatic acinar carcinoma, prostatic
atypical cribriform/solid lesions with basal cells represent ductal carcinoma, and urothelial carcinoma into prostatic
either cribriform high-grade prostatic intraepithelial neo- ducts and acini, currently IDC-P refers to a lumen-
plasia (HGPIN) or intraductal carcinoma of the prostate spanning proliferation of malignant cells within prostatic
(IDC-P). The distinction between these two is of para- ducts and acini caused by the spread of prostate cancer
mount importance, especially in prostate needle biopsy, cells within preexisting prostatic glandular structures. The
because IDC-P is usually associated with high-grade and first detailed analysis of such phenomenon was credited
high-volume prostate cancer (PCa). A diagnosis of IDC-P to Kovi et al,4 who studied 139 cases of PCa diagnosed on
in a biopsy mandates an immediate repeat biopsy or even transurethral resection, suprapubic prostatectomy, and
definitive therapy in the absence of documented invasive needle biopsy specimens and found the spread of PCa
PCa. In contrast, cribriform HGPIN is a type of putative cells into the preexisting prostate ducts and acini in 48%
neoplastic precursor lesion. Recent data have caused of PCa cases. Such ‘‘intraductal spread’’ was positively
researchers to question whether HGPIN on needle biopsy associated with both Gleason grade and tumor extent,
is associated with a significantly increased cancer risk in although only tumor extent, not Gleason grade, remained
subsequent biopsies and whether rebiopsy is necessary significantly associated with the intraductal spread in
within the first year after its diagnosis.1,2 the final multivariate analysis. The authors4 also depicted
This article reviews the historic perspective, histologic several morphologic patterns that represented various
features, diagnostic criteria, and molecular genetics of stages of the intraductal spread by PCa.
IDC-P. The clinical significance of finding IDC-P in both While studying cribriform PCa, McNeal et al5 found
radical prostatectomy and prostate biopsy specimens as that, in most cases, cribriform PCa was predominantly
located within prostatic ducts and acini with cancer cells
Accepted for publication December 16, 2011.
From the Department of Pathology, Weill Cornell Medical College,
following the normal duct contour or showing a basal
New York, New York (Dr Robinson); and the Pathology and Laboratory cell layer on morphologic examination or basal cell
Medicine Institute, Cleveland Clinic, Cleveland, Ohio (Drs Magi- immunostains. They found that the cribriform PCa with
Galluzzi and Zhou). Dr Zhou is now with the Department of Pathology, intraductal location was equivalent to Gleason patterns 4
New York University Langone Medical Center, New York. and 5 PCa prognostically and was associated with high-
The authors have no relevant financial interest in the products or grade and high-volume PCa in most cases. The term
companies described in this article.
Reprints: Ming Zhou, MD, Department of Pathology, New York intraductal carcinoma of the prostate was introduced to
University Langone Medical Center, 560 First Ave, TCH-461, New emphasize the unique histologic and clinical features of
York, NY 10016-6497 (e-mail: Ming.Zhou@nyumc.org). this lesion.
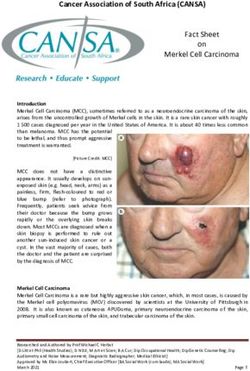
418 Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et alFigure 1. A, Intraductal carcinoma of the prostate, with cancer cells filling and expanding several prostatic ducts. B, Double immunostains for p63
and AMACR, with AMACR + staining in the proliferative cells and preserved basal cell layer (hematoxylin-eosin, original magnification 340 [A];
original magnification 340 [B]).
Because prostatic intraepithelial neoplasia (PIN) glands HISTOLOGIC FEATURES AND DIAGNOSIS OF IDC-P
also comprise cytologically atypical or malignant secreto- The hallmark of IDC-P is the expansile proliferation of
ry cells within prostatic ducts and acini, the relationship PCa cells within the native prostatic glands with an at least
between PIN and IDC-P was debated. Cribriform glands partially preserved basal cell layer (Figure 1, A and B).
lined with cytologically atypical secretory cells were McNeal and Yemoto8 first defined IDC-P as the ‘‘complete
considered to represent a part of the morphologic spec- spanning of the ductal or acinar lumen by several tra-
trum and, therefore, a histologic subtype of PIN,6,7 because beculae of malignant epithelial cells, with foci of trabec-
they were often present together with other types of PIN ular fusion’’8(p807) in radical prostatectomy specimens.
glands.6,7 However, some of these atypical cribriform More-proliferative, denser lesions with cribriform or
glands fit the morphologic criteria for IDC-P. McNeal et al5 solid architecture were also included in their definition.8
found that, in some cases, IDC-P was associated with Later studies refined the histologic features of IDC-P
HGPIN, with direct transition between the two or with (Table 1).10,11,14–17 Classic examples of IDC-P usually com-
both lesions adjacent to each other, suggesting that IDC-P prise many glands, often greater than 6 per radical pro-
arose primarily within ducts by evolution from the statectomy specimen,17 and the glands are larger than
premalignant PIN. normal peripheral zone glands,13,17 with irregular and
In a subsequent study, McNeal and Yemoto8 presented
evidence that IDC-P was different from PIN and suggest-
Table 1. Histologic Features That May Be Seen in
ed that it represented a distinct form of PCa with a Intraductal Carcinoma of the Prostate (IDC-P)
peculiar propensity for intraductal spread and growth.
They noted that the presence of cancer cells within IDC-P glands, No. Many; often .6 per prostate gland
Size Larger than normal glands; can be .1 mm
prostatic ducts and acini, or IDC-P, was almost never Ductal-lobular Native ducts and acini are expanded and
seen in the absence of invasive carcinoma, and the con- structure may show irregular and branching
comitant invasive component was usually high grade.8 contours
Furthermore, PCa with an IDC-P component had a Intraductal growth 1. Loose cribriform with cells forming
significantly worse prognosis than did PCa without an pattern narrow strands (often 2 cells thick);
spanning lumen without stromal support
IDC-P component. The authors concluded that IDC-P was
and intersecting randomly to form an
an entity with precisely defined histologic criteria and orderly lacework of empty spaces
unique biologic and clinical significance. Morphologically, 2. Micropapillary with cells forming
IDC-P and PIN could be reliably distinguished from each papillae with inconspicuous
other. fibrovascular cores
The concept that IDC-P represents intraductal growth of 3. Dense cribriform with cells forming
small, round ‘‘punched out’’ lumens that
advanced-stage PCa is supported by several subsequent comprise .50% of the luminal space
studies9–12 that also demonstrated the association of IDC-P 4. Solid cell mass
with other adverse pathologic features, such as higher Cytology 1. Cuboidal or low columnar
Gleason score, larger tumor volume, greater probability of 2. Significant nuclear atypia
extraprostatic extension, and poorer clinical outcomes. 3. Nuclei 6 times larger than adjacent
nonneoplastic nuclei
The current concept is that IDC-P represents intraductal 4. 2 cell populations with central small
extension of large-volume Gleason patterns 4 or 5 PCa. and uniform nuclei and peripheral
Rarely, IDC-P can be an isolated finding without a pleomorphic nuclei may be seen in
concomitant PCa and may represent a stage of prostate dense cribriform and solid patterns
carcinogenesis that is later than what is recognized as Comedonecrosis May be present
Basal cell layer Preserved, at least focally
HGPIN but before invasive PCa.13,14
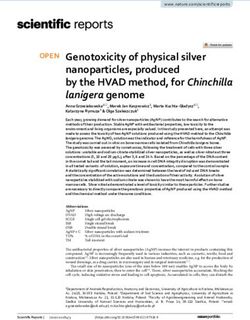
Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et al 419Figure 2. Histologic features of intraductal carcinoma of the prostate (IDC-P) include loose cribriform (A), dense cribriform (B), and solid growth patterns (C). Note the 2 cell populations with pleomorphic nuclei at the periphery and the smaller and more-uniform nuclei at the center (A and B). Nonfocal comedonecrosis (D) and marked nuclear pleomorphism with a size six times larger than the adjacent nonneoplastic cells (E) can also be seen. Two cell populations may be seen, with small and uniform nuclei in the center and pleomorphic nuclei at the periphery (F). Dense cribriform and solid patterns, nonfocal comedonecrosis, and marked pleomorphic nuclei are features diagnostic of IDC-P (hematoxylin-eosin, original magnifications [A through F]). 420 Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et al
Table 2. Diagnostic Criteria for Intraductal
Carcinoma of the Prostate
Malignant epithelial cells filling large acini and prostatic ducts,
with preservation of basal cells and:
N Solid or dense cribriform pattern
or
N Loose cribriform or micropapillary pattern with either
# Marked nuclear atypia: nuclear size 6x normal or larger
# Nonfocal comedonecrosis
Reprinted from 16Guo CC, Epstein JI. Mod Pathol. 2006;19(12):1528–
1535 with permission from the Nature Publishing Group.
branching contours (Figure 2, A).8,13,17 The neoplastic cells
in IDC-P grow in several architectural patterns, including
trabecular, loose cribriform (Figure 2, A), dense cribri-
form (Figure 2, B), and solid (Figure 2, C), which
represent progressive dedifferentiation, with a reciprocal
increase in proliferation and correlated with cancer stage,
grade, and clinical course.10 Neoplastic cells in classic
IDC-P are pleomorphic, some 6 times larger than adja-
cent nonneoplastic nuclei (Figure 2, E). Two cell popu-
lations may be seen, usually in the dense cribriform and
solid IDC-P, in which a central population of cells has
small and uniform nuclei, and the peripheral population
cells have pleomorphic nuclei (Figure 2, F). Comedone-
crosis is diagnostic of IDC-P but is only present in a sub-
set of cases (Figure 2, E).
Cohen et al13 proposed a set of criteria for diagnosing
IDC-P, which included 5 major and 3 minor criteria. The
first 4 major criteria are always present in IDC-P and
include (1) large-caliber glands that are more than twice
the diameter of normal peripheral zone glands, (2) pre-
served basal cells as identified with basal cell markers, (3)
cytologically malignant cells, and (4) an expansile cell
mass that spans the glandular lumen. The fifth major Figure 3. A prostate biopsy containing an atypical cribriform lesion
criterion, central comedonecrosis, is diagnostic of IDC-P with loose cribriform architecture (A) lined with atypical cells (B). Such
but is not always present. Minor criteria include glands a lesion is not diagnostic of intraductal carcinoma of the prostate (IDC-
with (1) right-angle branching or (2) smooth, rounded P) but may represent part of a morphologic spectrum of IDC-P. It
should, therefore, be diagnosed as atypical cribriform lesion, IDC-P
outlines; and (3) 2 cell populations with an outer perimeter cannot be ruled out (hematoxylin-eosin, original magnifications 340
cell group composed of tall, pleomorphic, and mitotically [A] and 3200 [B]).
active cells that stain poorly for prostate-specific antigen
(PSA), and a central group that is cuboidal, monomorphic,
and quiescent, with abundant cytoplasm containing
DIFFERENTIAL DIAGNOSIS OF IDC-P
abundant PSA and occasional extracellular mucin.
In 2006, Guo and Epstein16 proposed diagnostic criteria Intraductal carcinoma of the prostate should be differ-
for IDC-P in prostate biopsies (Table 2), which were entiated from other prostate lesions with cribriform and/
subsequently used in a larger study of IDC-P from the or solid architecture, which range from normal histologic
same institution.14 In these 2 studies, in addition to the structures or benign lesions to premalignant lesions and
presence of malignant epithelial cells filling large acini frank malignancies (Table 3).
and prostatic ducts with preservation of basal cells, the
diagnosis of IDC-P required the presence of (1) a solid or Normal Prostatic Structures and Benign Lesions
dense cribriform pattern (Figures 1 and 2, B and C), where Normal histologic variations, such as central zone pro-
punched-out, luminal spaces account for less than 50% of state glands, and benign glandular proliferations, such as
the central cellular mass; or (2) marked nuclear atypia, cribriform clear cell hyperplasia and basal cell hyperpla-
where the nuclei are at least 6 times larger than adjacent, sia, can be present as cribriform or, rarely, as solid struc-
benign nuclei (Figure 2, E); or (3) nonfocal comedonecro- tures. However, nuclear atypia, mitotic figures, and
sis (Figure 2, D). Lesions that fell short of these criteria but comedonecrosis are absent.
were still felt to be more ominous than HGPIN were
labeled atypical intraductal proliferations (Figure 3, A and B) High-Grade PIN
when the differential diagnosis was between HGPIN and The distinction of isolated IDC-P from cribriform
IDC-P. This diagnostic approach is summarized in HGPIN in prostate biopsy is the most important differen-
Figure 4 and provides specific and reproducible criteria tial diagnosis because management for these 2 conditions
for the diagnosis of IDC-P. is considerably different.
Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et al 421loose cribriform and micropapillary patterns, other cyto-
logic features are required, such as markedly enlarged and
pleomorphic nuclei (.6 times that of adjacent nonneo-
plastic glands) and nonfocal comedonecrosis.
These criteria can reliably distinguish IDC-P and
HGPIN in most cases. However, some IDC-P glands have
morphologic features that overlap with HGPIN. In 2
recent studies, Shah et al17 and Han et al18 demonstrated
that some IDC-P glands that were intermixed and shared
the same TMPRSS2-ERG gene fusion with invasive PCa
were architecturally and cytologically similar to the
HGPIN glands that were distant from the invasive PCa
and lacked the TMPRSS2-ERG gene fusion. Both comprise
small cribriform glands with round and smooth contours
and are lined with low-grade nuclei. These findings
suggest that IDC-P can occasionally exhibit a ‘‘low grade’’
morphology that overlaps with HGPIN and does not fit
the diagnostic criteria for IDC-P. Therefore, any cribriform
or lumen-spanning, atypical lesion may represent IDC-P,
and its presence in prostate needle biopsies merits
aggressive workup.
High-grade PIN and IDC-P share immunohistochemi-
cal profiles, including positive staining for PSA, a-
methylacyl-coenzyme A racemase (AMACR), and basal
cells. However, none of the stains is helpful in the
differential diagnosis of these two entities.
Invasive Cribriform Acinar Adenocarcinoma of Prostate
Infiltrating cribriform acinar adenocarcinoma (Gleason
patterns 4 or 5, depending on whether comedonecrosis is
present) closely mimics cribriform IDC-P. Invasive cribri-
form cancer, unlike IDC-P, lacks a basal cell lining. In
Figure 4. Diagnostic algorithm for prostate biopsy containing atyp- some cases, the contour and branching pattern of normal
ical cribriform lesions. Abbreviation: IDC-P, intraductal carcinoma of duct architecture distinguishes IDC-P from infiltrating
the prostate. cribriform acinar adenocarcinoma. The distinction be-
tween invasive, high-grade PCa and IDC-P, however, is
Both HGPIN and IDC-P represent the presence of not critical because IDC-P is usually associated with a
cytologically atypical or malignant cells within prostatic high-grade and high-volume PCa. Most cases of IDC-P
ducts and acini, although the architectural and cytologic would be diagnosed as cribriform acinar adenocarcinoma
atypia is always more pronounced in IDC-P. Cribriform if immunohistochemistry for basal cells is performed.
HGPIN is rare. The glands are small with smooth and
round contours, and the cells are relatively uniform Ductal Adenocarcinoma of the Prostate
without marked nuclear pleomorphism or necrosis in Ductal adenocarcinoma is an aggressive form of PCa
cribriform HGPIN. Loose cribriform and micropapillary and may occasionally arise in the peripheral zone, and
patterns can be seen in both HGPIN and IDC-P, but dense ordinary acinar prostate carcinoma may have features of
cribriform, solid patterns, and comedonecrosis are not ductal adenocarcinoma focally. It is defined by morpho-
seen in HGPIN. To establish the diagnosis of IDC-P in the logic features, including tall, pseudostratified, columnar
Table 3. Differential Diagnosis of Intraductal Carcinoma of the Prostate (IDC-P)
Cribriform or Urothelial Carcinoma
Feature IDC-P HGPIN Solid PCa Involving the Prostate
Ductal-lobular structure Expanded Preserved Distorted Preserved (usually)
Gland size Increased (.2 times size of Normal Variable Variable
normal glands)
Lumen-spanning cell mass Present Present in cribriform Present Present
HGPIN
Absent in other types
Intraductal growth pattern 1. Micropapillary/trabecular 1. Micropapillary 1. Cribriform 1. Solid (typically)
2. Cribriform (loose, dense) 2. Cribriform (loose) 2. Solid 2. Cribriform
3. Solid 3. Flat
4. Tufting
Comedonecrosis 6 2 6 6
Basal cells + + 2 +
Abbreviations: HGPIN, high-grade prostatic intraepithelial neoplasia; PCa, prostate cancer.
Modified from 24Henry PC, Evans AJ. J Clin Pathol. 2009;62(7):579–583, with permission from the BMJ Publishing Group Ltd.
422 Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et alepithelium, arranged in cribriform patterns with slitlike lost loci were 8p22 and 16q23.1-qter. In IDC-P with asso-
spaces and/or true papillary fronds. The papillae in ciated Gleason grade 4 invasive carcinoma, the authors
ductal adenocarcinoma have true fibrovascular cores, and reported 16 instances of LOH, 12 (75%) of which were not
the cells may show significant nuclear atypia with a high seen in the invasive tumor component. Similarly, of the 9
mitotic rate and extensive necrosis. Nuclei are large, instances of LOH recorded in Gleason grade 4 cancers, 5
mostly elongated or oval, and often contain a single (56%) were not seen in the IDC-P from the same patient.
macronucleolus. In contrast, IDC-P has cuboidal cells, The single case of PIN with LOH (at 2 loci) shared both of
cribriform pattern with rounded lumina, and micropapil- those losses with the coexistent IDC-P.
lary tufting without fibrovascular cores. Bettendorf and colleagues20 analyzed 77 radical prosta-
Similar to other high-grade and high-volume prostate tectomy specimens for LOH of the tumor suppressor
cancers, ductal PCa is also prone to intraductal spread. genes TP53, RB1, and PTEN, and they investigated IDC-P
Residual basal cells are, therefore, often found in ductal and PIN for chromosomal anomalies using comparative
PCa.19 Ductal PCa with basal cells is mechanistically IDC- genomic hybridization. During comparative genomic
P, and Cohen et al13 proposed to classify ductal PCa as hybridization analysis, 73% of IDC-P cases (8 of 11)
IDC-P. However, ductal PCa is not synonymous with IDC- showed several chromosomal imbalances, which is in
P because IDC-P has characteristic morphologic features. stark contrast to PIN, wherein no comparative genomic
Furthermore, not all ductal PCa cases have residual basal hybridization changes were found. Five chromosomal
cells and, therefore, are not ‘‘intraductal carcinomas.’’ gains and 19 chromosomal losses were detected in IDC-P:
21q23–q32, 25p, 26cen–q22, +7p, +7q, 28p, +8q21.1–qter,
Urothelial Carcinoma Involving the Prostate 210p, 210q, 210q21–qter, 213q, 213q14–qter, 216q,
Intraductal spread of urothelial carcinoma, either from a 216q13–qter, 217p, 218q, +19p, and +19q. Alterations of
bladder primary tumor or, in rare cases, from a prostate 7p, 7q, and 10q were previously identified as ‘‘late events’’
primary tumor, may mimic IDC-P. Urothelial carcinoma associated with recurrent or metastatic cancer. On the
cells may fill and distend the lumen of the prostatic ducts, other end, loss at 8p is recognized as an early genetic
and central necrosis may occur, imparting a morphology change, which seems to link IDC-P to the PCa progression
similar to IDC-P. However, urothelial carcinoma is typi- pathway involving PIN.21 Loss of heterozygosity for PTEN
cally more pleomorphic than IDC-P is cytologically, and was found in 44% of PIN lesions, 48% of IDC-P, 49% of
urothelial carcinoma often has a dense pink, ‘‘hard’’ cyto- organ-confined (OC) PCa, and 50% of non-OC PCa. Loss
plasmic quality. A panel of immunostains can often of heterozygosity for TP53 was found in 30% of PIN, 60%
resolve the diagnostic ambiguity. Intraductal carcinoma of IDC-P, 40% of OC PCa, and 66% of non-OC PCa. Loss
of the prostate stains positive for prostate-specific mark- of heterozygosity of RB1 was detected in 53% of PIN, 81%
ers, including PSA, prostate-specific acid phosphatase, of IDC-P, 60% of OC PCa, and 78% of non-OC PCa. Loss of
prostate-specific membrane antigen, and P501S, whereas heterozygosity of both tumor suppressor genes TP53 and
stains for basal cells, such as CK5/6, 34bE12, and p63, are RB1 was found in 52% of IDC-P compared with 19% of
positive only in the basal cells at the periphery of the PIN, 24% of OC PCa, and 44% of non-OC PCa.20
cancer glands. In contrast, urothelial carcinoma is negative To better understand the molecular and biologic basis of
for prostate specific markers (PSA and prostate-specific distinction between cribriform HGPIN and IDC-P, Han
acid phosphatase) and is positive in two-thirds of cases for et al18 assessed ETS gene alterations using a break-apart
markers that recognize the prostate basal cells (cytokeratin fluorescence in situ hybridization assay. They found no
34bE12 and p63). ERG rearrangement in isolated cribriform HGPIN, where-
as ERG was rearranged in 75% of IDC-P (36 of 48), of
Metastatic Adenocarcinoma which 65% (23 of 31) were through deletion. The authors
Metastatic adenocarcinoma from other sites, in partic- found 100% concordance of ERG gene fusion status
ular, colorectal adenocarcinoma, may have extensive between IDC-P and adjacent invasive PCa, suggesting
necrosis and mimic IDC-P. On hematoxylin-eosin stains, that IDC-P is clonally related to the latter.
the presence of ‘‘dirty’’ necrosis, a columnar appearance The allelic instability reported in IDC-P clearly distin-
of cells with basally located nuclei, and mucus secretions guishes it from PIN. Although there is morphologic evi-
are features that suggest the enteric origin of the lesion. dence that PIN can progress to IDC-P, the number and
Clinical history and prudent use of immunostains (CDX-2, frequency of molecular changes in IDC-P (36 of 48), as
CK20, and b-catenin for colorectal adenocarcinoma) can compared with PIN, indicate that the former is a
lead to a correct diagnosis. malignant progression far removed from PIN. Intraductal
carcinoma of the prostate, in most cases, likely represents
MOLECULAR GENETICS OF IDC-P intraductal spread of nearby, well-established, invasive
Molecular evidence to support the classification of IDC- carcinoma and a late event in prostate carcinogenesis.
P as a discrete entity comes from studies assessing loss of
heterozygosity (LOH) at microsatellite loci often affected CLINICAL SIGNIFICANCE OF IDC-P
in PCa. Studies have established that IDC-P represents an
Dawkins et al15 studied allelic instability in prostate aggressive form of PCa and is an adverse pathologic
cancers to define the position of IDC-P in PCa progression. parameter in both radical prostatectomy and needle bio-
They compared the patterns of allelic loss in PIN, PCa psy specimens.
with Gleason grade 3 and 4 patterns, and IDC-P. They Since the initial studies by Kovi et al4 and McNeal et al,8
observed no LOH in Gleason grade 3 carcinomas, and several other studies have investigated IDC-P in radical
only a single example in PIN (1 of 11; 9%). In contrast, 60% prostatectomy and consistently found that the presence of
of IDC-P cases (12 of 20) and 29% of Gleason grade 4 IDC-P correlated with other adverse pathologic features,
cancers (15 of 17) demonstrated LOH. The most frequently including higher Gleason score, larger tumor volume, and
Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et al 423greater probability of extraprostatic extension, seminal of prostate carcinogenesis that is greater than what we
vesicle invasion, and pelvic lymph node metastasis. It also recognize as HGPIN morphologically but develops before
correlated with decreased progression-free survival and invasive cancer.
with postsurgical, biochemical recurrence.10–12,15,17 Based on their studies of needle biopsy with IDC-P and
Only a few studies to date have examined the signifi- previous studies in the literature that demonstrated
cance of IDC-P in needle core biopsy specimens, and, in 2 consistent association of IDC-P at radical prostatectomy
of these studies, IDC-P was present without associated with multiple adverse prognostic factors, Robinson and
invasive carcinoma in the biopsies,14,16 an exceedingly rare Epstein14 recommend definitive therapy in men with IDC-
finding, involving less than 0.06% of all prostate biopsy P on needle biopsy, even in the absence of pathologically
specimens. documented, invasive PCa.
Cohen et al9 studied a small series of radical prostatec-
tomy specimens with matching preoperative needle REPORTING OF IDC-P IN PROSTATE BIOPSY
biopsy specimens and found that the inclusion of IDC-P Because of its frequent association with high-grade and
in prostate biopsies in a preoperative model could im- high-volume PCa, as well as its adverse prognostic signifi-
prove the prediction of the pathologic stage of the radical cance, IDC-P should be reported in prostate biopsy reports.
prostatectomy specimens. Furthermore, the presence of In most cases, IDC-P is identified with a concomitant,
IDC-P on biopsy correlated strongly with biochemical invasive PCa that usually contains cancer with Gleason
failure.9 This study also found that serum PSA levels patterns 4 or 5. In these cases, reporting on the IDC-P is of
correlated with tumor volume only when IDC-P was not questionable value. Nevertheless, we recommend the
present in the biopsy, similar to results in an earlier IDC-P be reported in these cases because IDC-P may
study.22 These findings suggest that IDC-P identified in provide additional prognostic information.
prostate biopsy is a very powerful parameter that coun- Rarely, IDC-P is seen on a biopsy with PCa of only a
teracts the predictive values of other commonly used
Gleason pattern 3. In those cases, it is imperative to
clinicopathologic parameters, including serum PSA and
document the presence of IDC-P, and that can be done in 2
biopsy Gleason score. This has potentially profound clini-
ways. IDC-P can be regarded as, and graded like, invasive
cal significance because virtually all nomograms for pre-
PCa (Gleason patterns 4 or 5, depending on the absence or
dicting prostate cancer stage and outcome include serum
presence of solid architecture and/or necrosis, respective-
PSA as a variable, yet none takes into account the presence
of IDC-P as potentially masking a high-volume, high- ly). Alternatively, one can grade only the invasive PCa
stage tumor with relatively low serum PSA. Similarly, a Gleason pattern 3 and then mention in a comment the
recent study by O’Brien et al23 found that inclusion presence of IDC-P and its clinical significance.
of several new pathologic variables, including IDC-P, When IDC-P is identified on prostate biopsy without
significantly improved the predictive accuracy of a concomitant invasive PCa, pathologists should report the
postoperative nomogram that used preoperative clinico- presence of IDC-P with a comment stating that IDC-P is
pathologic variables to predict PSA recurrence after usually associated with a high-grade and high-volume
radical prostatectomy. These studies strongly suggest that PCa and that definitive therapy is indicated for those
the presence of IDC-P in prostate biopsies should be patients.14,16 However, some pathologists may still recom-
reported, even when it is associated with an extensive, mend immediate repeat biopsy, instead of definitive
high-grade PCa because it may provide additional prog- therapy, in these rare situations.
nostic information. Finally, any cribriform lesion comprising cytologically
Guo and Epstein16 initially reported a small series of atypical cells that do not satisfy the diagnostic criteria for
cases of IDC-P without invasive carcinoma on biopsy, and IDC-P but that exceed the criteria for HGPIN should be
more recently, Robinson and Epstein14 updated and reported as atypical cribriform lesion, with a recommenda-
expanded that series to include 66 patients. Both studies tion for an immediate repeat biopsy because it may
found that the presence of IDC-P, even in the absence of represent IDC-P.
documented invasive carcinoma, was associated with an
aggressive clinical course. In the more contemporary of CONCLUSIONS
the 2 studies, 8 of 66 patients (12%) developed disease Intraductal carcinoma of the prostate is a distinct
progression after definitive treatment, including 4 patients clinicopathologic entity. Morphologically, it is character-
with distant metastasis at a mean of 22 months after ized by lumen-spanning or solid proliferation of malig-
diagnosis, and another 4 patients with PSA recurrence at nant cells that expand the preexisting ducts and acini.
a mean of only 8 months following definitive therapy. Intraductal carcinoma of the prostate is strongly associat-
Furthermore, in patients who underwent radical prosta- ed with aggressive PCa with a high Gleason grade and a
tectomy, all prostate cancers had Gleason scores equal to large tumor volume. Therefore, it is critical for patholo-
or more than 7, and nearly one-half of the cases (9 of 21) gists to recognize and report this lesion in prostate speci-
contained some Gleason pattern 5 components. Tumors mens, especially in prostate biopsy reports, for patient
were also of relatively high volume (mean, 2.85 cm3; range, management. Morphologic criteria have been proposed
0.05-13.1 cm3 ). Eight of 21 men (38%) had extraprostatic to distinguish IDC-P from several other lesions with
extension (pT3a), and another 3 (14%) had seminal vesicle similar histologic appearance, such as HGPIN, invasive
invasion (pT3b). Nodal metastasis was seen in 1 (5%) of cribriform PCa, and urothelial carcinoma involving the
the men. Two patients (10%) had IDC-P only at radical prostate.
prostatectomy, without an invasive PCa component. This Reference
latter finding suggests that IDC-P does not always 1. Epstein JI, Herawi M. Prostate needle biopsies containing prostatic
represent intraductal spread of an invasive, high-grade intraepithelial neoplasia or atypical foci suspicious for carcinoma: implications
carcinoma. In at least some cases, IDC-P represents a stage for patient care. J Urol. 2006;175(3, pt 1):820–834.
424 Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et al2. Montironi R, Mazzucchelli R, Lopez-Beltran A, Scarpelli M, Cheng L. 15. Dawkins HJ, Sellner LN, Turbett GR, et al. Distinction between intraductal
Prostatic intraepithelial neoplasia: its morphological and molecular diagnosis and carcinoma of the prostate (IDC-P), high-grade dysplasia (PIN), and invasive
clinical significance. BJU Int. 2011;108(9):1394–1401. prostatic adenocarcinoma, using molecular markers of cancer progression.
3. Catalona WJ, Kadmon D, Martin SA. Surgical considerations in treatment of Prostate. 2000;44(4):265–270.
intraductal carcinoma of the prostate. J Urol. 1978;120(2):259–261. 16. Guo CC, Epstein JI. Intraductal carcinoma of the prostate on needle biopsy:
4. Kovi J, Jackson MA, Heshmat MY. Ductal spread in prostatic carcinoma. histologic features and clinical significance. Mod Pathol. 2006;19(12):1528–
Cancer. 1985;56(7):1566–1573. 1535.
5. McNeal JE, Reese JH, Redwine EA, Freiha FS, Stamey TA. Cribriform 17. Shah RB, Magi-Galluzzi C, Han B, Zhou M. Atypical cribriform lesions of
adenocarcinoma of the prostate. Cancer. 1986;58(8):1714–1719. the prostate: relationship to prostatic carcinoma and implication for diagnosis in
6. Amin MB, Schultz DS, Zarbo RJ. Analysis of cribriform morphology in prostate biopsies. Am J Surg Pathol. 2010;34(4):470–477.
prostatic neoplasia using antibody to high-molecular-weight cytokeratins. Arch 18. Han B, Suleman K, Wang L, et al. ETS gene aberrations in atypical
Pathol Lab Med. 1994;118(3):260–264. cribriform lesions of the prostate: implications for the distinction between
7. Bostwick DG, Amin MB, Dundore P, Marsh W, Schultz DS. Architectural intraductal carcinoma of the prostate and cribriform high-grade prostatic
patterns of high-grade prostatic intraepithelial neoplasia. Hum Pathol. 1993; intraepithelial neoplasia. Am J Surg Pathol. 2010;34(4):478–485.
24(3):298–310.
19. Herawi M, Epstein JI. Immunohistochemical antibody cocktail staining
8. McNeal JE, Yemoto CE. Spread of adenocarcinoma within prostatic ducts and
(p63/HMWCK/AMACR) of ductal adenocarcinoma and Gleason pattern 4
acini: morphologic and clinical correlations. Am J Surg Pathol. 1996;20(7):802–814.
cribriform and noncribriform acinar adenocarcinomas of the prostate. Am J Surg
9. Cohen RJ, Chan WC, Edgar SG, et al. Prediction of pathological stage and
Pathol. 2007;31(6):889–894.
clinical outcome in prostate cancer: an improved preoperative model incorpo-
20. Bettendorf O, Schmidt H, Staebler A, et al. Chromosomal imbalances, loss
rating biopsy-determined intraductal carcinoma. Br J Urol. 1998;81(3):413–418.
10. Cohen RJ, McNeal JE, Baillie T. Patterns of differentiation and proliferation of heterozygosity, and immunohistochemical expression of TP53, RB1, and PTEN
in intraductal carcinoma of the prostate: significance for cancer progression. in intraductal cancer, intraepithelial neoplasia, and invasive adenocarcinoma of
Prostate. 2000;43(1):11–19. the prostate. Genes Chromosomes Cancer. 2008;47(7):565–572.
11. Rubin MA, de La Taille A, Bagiella E, Olsson CA, O’Toole KM. Cribriform 21. Ribeiro FR, Diep CB, Jeronimo C, et al. Statistical dissection of genetic
carcinoma of the prostate and cribriform prostatic intraepithelial neoplasia: pathways involved in prostate carcinogenesis. Genes Chromosomes Cancer.
incidence and clinical implications. Am J Surg Pathol. 1998;22(7):840–848. 2006;45(2):154–163.
12. Wilcox G, Soh S, Chakraborty S, Scardino PT, Wheeler TM. Patterns of 22. Cohen RJ, Haffejee Z, Steele GS, Nayler SJ. Advanced prostate cancer with
high-grade prostatic intraepithelial neoplasia associated with clinically aggressive normal serum prostate-specific antigen values. Arch Pathol Lab Med. 1994;
prostate cancer. Hum Pathol. 1998;29(10):1119–1123. 118(11):1123–1126.
13. Cohen RJ, Wheeler TM, Bonkhoff H, Rubin MA. A proposal on the 23. O’Brien BA, Cohen RJ, Wheeler TM, Moorin RE. A post-radical-
identification, histologic reporting, and implications of intraductal prostatic prostatectomy nomogram incorporating new pathological variables and interac-
carcinoma. Arch Pathol Lab Med. 2007;131(7):1103–1109. tion terms for improved prognosis. BJU Int. 2011;107(3):389–395.
14. Robinson BD, Epstein JI. Intraductal carcinoma of the prostate without 24. Henry PC, Evans AJ. Intraductal carcinoma of the prostate: a distinct
invasive carcinoma on needle biopsy: emphasis on radical prostatectomy histopathological entity with important prognostic implications. J Clin Pathol.
findings. J Urol. 2010;184(4):1328–1333. 2009;62(7):579–583.
Arch Pathol Lab Med—Vol 136, April 2012 Intraductal Carcinoma of the Prostate—Robinson et al 425You can also read