Personalized care of obstructive sleep apnea with hypoglossal nerve stimulation - Oxford Academic Journals
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
SLEEPJ, 2021, S1–S3
doi: 10.1093/sleep/zsab055
Editorial
Editorial
Downloaded from https://academic.oup.com/sleep/article/44/Supplement_1/S1/6253813 by guest on 02 November 2021
Personalized care of obstructive sleep apnea with
hypoglossal nerve stimulation
Patrick J. Strollo1,* and Ryan J. Soose2
Department of Medicine, University of Pittsburgh, Pittsburgh, PA and 2Department of Otolaryngology,
1
University of Pittsburgh, Pittsburgh, PA
*Corresponding author. Patrick J. Strollo, Department of Medicine, University of Pittsburgh, UPMC Montefiore, Suite S639.11, 3459 Fifth Avenue, Pittsburgh,
PA 15213. Email: strollopj@upmc.edu.
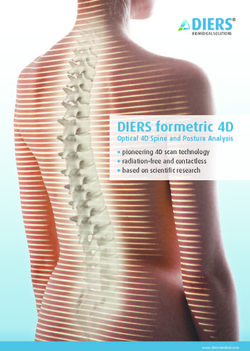
Hypoglossal Nerve Stimulation (HNS) is an option for pa- in many instances to assess the treatment response with lower
tients with obstructive sleep apnea who cannot accept or ad- cost and more ecologically valid home sleep testing strategy.
here to positive pressure therapy (PAP) [1]. Unilateral phasic Using the algorithm presented in the text, well-treated and
HNS during sleep has been demonstrated to effectively adherent patients (Green Pathway) can be readily identified, and
treat obstructive sleep apnea. The Inspire Medical Systems sub-optimally treated patients (Yellow Pathway) can be categor-
HNS device is approved by the United States Food and Drug ized based on the nature of the problem- be it suboptimal adher-
Administration and in the Europe Economic Area by a CE ence (Type 1), inadequate control of sleep-disordered breathing /
marking. This technology includes a hypoglossal nerve cuff persistent symptoms (Type 2), or both (Type 3).
electrode, impulse generator, and a pressure sensor that are Targeted interventions are discussed based on the type of
surgically implanted. The patient allows for turning on/off, problems encountered. As with the management of PAP pa-
pausing therapy, and adjusting HNS amplitude during the tients, there are device-specific interventions, adjunctive sur-
sleep period (Figure 1). Over 10,000 devices have been im- gical interventions, and medical interventions [5–7]. To fully treat
planted in over 400 centers in the United States and Europe. a given patient, it is essential to holistically address a patient’s
The Centers for Medicare and Medicaid Services and most needs. It is important to troubleshoot and make focused adjust-
Commercial Insurers cover HNS in all 50 states and the ments to the device as well as to be able to provide hypnotics,
District of Columbia in the United States. cognitive behavioral therapy for insomnia, positional therapy,
Research reports to date have focused primarily on the im- lifestyle modifications, stimulants, and other adjunctive treat-
plantation technique and the initial activation of HNS as well ments when indicated. Approximately one-third of patients
as the safety and efficacy of treatment from carefully designed with OSA have comorbid insomnia and approximately 10% have
trials and a research registry [1–3]. As this therapeutic option residual daytime sleepiness despite adequate treatment of OSA
has become more available, strategies to address treatment suc- [8–10]. These data highlight the need for the Sleep Surgeon and
cess on a patient level are necessary. The two papers included in the Sleep Physician to work collaboratively to personalize care.
this supplement provide additional insight for clinicians so that In the second paper, Johnson et al. utilize a biophysical com-
longitudinal care can be optimized. putational model to provide insight into how reconfiguring the
In the first paper, Soose and colleagues outline an approach stimulation settings of the HNS cuff electrode can affect the
to care that focuses on the post-implant management [4]. An treatment response [11]. The clinical data from the STAR trial
algorithm informed by the experience of five high-performing were utilized to develop the model [1]. These data give the scien-
HNS programs is presented. The timing and the implementa- tific rationale for bipolar versus unipolar stimulation configur-
tion of device activation are reviewed. The insights provided by ations. They demonstrate that a unipolar configuration provides
office-based assessments in conjunction with cloud-based data more uniform axonal activation resulting in a lower stimulation
downloads (like PAP devices) have decreased the need for re- sensation and functional thresholds with less negative impact
peated “in-lab” adjustments of HNS settings. This has allowed if the HNS cuff rotates. The model also provides insight into
© Sleep Research Society 2021. Published by Oxford University Press on behalf of the Sleep Research Society.
All rights reserved. For permissions, please email: journals.permissions@oup.com
S1S2 | SLEEPJ, 2021, Vol. 44, No. S1
Downloaded from https://academic.oup.com/sleep/article/44/Supplement_1/S1/6253813 by guest on 02 November 2021
Figure 1. Hypoglossal nerve stimulation system. Adapted from Strollo et al. [1]. Copyright © 2014, Massachusetts Medical Society Reprinted with Permission.
how unipolar configurations may inadvertently activate tongue 4. Soose RJ, et al. Post-implant care pathway: lessons learned
retrusor muscles (Styloglossus and/or Hyoglossus) due to the and recommendations after 5 years of clinical implemen-
relatively high current densities at the nerve cuff end. tation of hypoglossal nerve stimulation therapy. Sleep.
This collection of papers gives us practical insights into the 2021;44(S1). doi:10.1093/sleep/zsaa279.
personalized management of HNS post-implantation. Ongoing 5. Chapman JL, et al. Residual daytime sleepiness in ob-
research will further enhance our understanding. Our team is structive sleep apnea after continuous positive airway
currently collecting qualitative data to better understand why pressure optimization: causes and management. Sleep Med
some patients may not use HNS the entire night (START Trial Clin. 2016;11(3):353–363.
6. Johnson DM, et al. Updated nasal surgery for obstructive
NCT 04768543). These data will help with the development of
sleep apnea. Adv Otorhinolaryngol. 2017;80:66–73.
additional educational interventions, the leveraging of digital
7. Lee JJ, et al. Severe obstructive sleep apnea treated with
health platforms, and the targeted treatment of comorbid sleep
combination hypoglossal nerve stimulation and oral appli-
problems. Research involving the refinement of selection cri-
ance therapy. J Dental Sleep Med. 2015;2:185–186.
teria with imaging (CT/MR) and physiologic phenotyping may
8. Gasa M, et al.; Scientific Council of the Sleep Registry of
also help improve initial and longitudinal response to HNS [12–
the French Federation of Pneumology-FFP. Residual sleepi-
15]. We still need to understand what constitutes an adequate ness in sleep apnea patients treated by continuous positive
treatment response. Should measures of cardiovascular risk airway pressure. J Sleep Res. 2013;22(4):389–397.
such as nocturnal blood pressure, hypoxic burden, and/or REM- 9. Luyster FS, et al. Comorbid insomnia and obstructive sleep
related sleep-disordered breathing be given more weight than apnea: challenges for clinical practice and research. J Clin
the apnea/hypopnea index? [16–18] Can HNS mitigate cardio- Sleep Med. 2010;6(2):196–204.
vascular risk? [19] There is undoubtedly more work to be done 10. Sweetman A, et al. Co-Morbid Insomnia and Sleep Apnea
so that we can further optimize this additional tool in our treat- (COMISA): prevalence, consequences, methodological con-
ment toolbox. siderations, and recent randomized controlled trials. Brain
Sci. 2019;9.
11. Johnson M, et al. Model-based analysis of implanted hypo-
glossal nerve stimulation for the treatment of obstructive
References sleep apnea. Sleep. 2021;44(S1). doi:10.1093/sleep/zsaa269.
1. Strollo PJ Jr, et al.; STAR Trial Group. Upper-airway 12. Carberry JC, et al. Personalized management approach for
stimulation for obstructive sleep apnea. N Engl J Med. OSA. Chest. 2018;153(3):744–755.
2014;370(2):139–149. 13. Lee CH, et al. Clinical radiographic predictors of response to
2. Heiser C, et al. Post-approval upper airway stimulation pre- hypoglossal nerve stimulation for obstructive sleep apnea.
dictors of treatment effectiveness in the ADHERE registry. Otolaryngol Head Neck Surg. 2020:194599820963141.
Eur Respir J. 2019;53. 14. Lee CH, et al. Therapeutic positive airway pressure
3. Woodson BT, et al. Upper airway stimulation for obstructive level predicts response to hypoglossal nerve stimu-
sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. lation for obstructive sleep apnea. J Clin Sleep Med.
2018;159(1):194–202. 2019;15(8):1165–1172.Strollo and Soose | S3
15. Schwab RJ, et al. Anatomic predictors of response and 17. Kwon Y, et al. Blood pressure monitoring in sleep: time to
mechanism of action of upper airway stimulation therapy wake up. Blood Press Monit. 2020;25(2):61–68.
in patients with obstructive sleep apnea. Sleep. 2018;41(4). 18. Mokhlesi B, et al. Obstructive sleep apnea during REM sleep
doi:10.1093/sleep/zsy021 and hypertension. results of the Wisconsin Sleep Cohort.
16. Azarbarzin A, et al. The hypoxic burden of sleep apnoea Am J Respir Crit Care Med. 2014;190(10):1158–1167.
predicts cardiovascular disease-related mortality: the 19. Gottlieb DJ. Does obstructive sleep apnea treatment re-
Osteoporotic Fractures in Men Study and the Sleep Heart duce cardiovascular risk?: It is far too soon to say. JAMA.
Health Study. Eur Heart J. 2019;40(14):1149–1157. 2017;318(2):128–130.
Downloaded from https://academic.oup.com/sleep/article/44/Supplement_1/S1/6253813 by guest on 02 November 2021You can also read