Person-centric clinical trials: defining the N-of-1 clinical trial utilizing a practice-based translational network
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Clinical Trial Perspective
& Ter-
Person-centric clinical trials: defining the
N-of-1 clinical trial utilizing a
practice-based translational network
A person-centric clinical trial is inclusive of both the investigator and the person and Frederick A Curro*,1, Dennis A
as such represents point-of-use data generated at the practice level and encompasses Robbins2, Frederick Naftolin3,
both health and disease. Raising the clinical encounter to a research encounter and Ashley C Grill4, Don Vena5
providing an infrastructure to support a level of quality assurance creates a synergy & Louis Terracio6
1
PEARL, Translational Network, 3 Powell
for efficiency for healthcare delivery. The interface of translational studies and clinical Road, Emerson, N.J. 07630; New York
research poses an opportunity, whereby person-centricity can support transparency, University, New York, NY 10010, USA
facilitate informed consent, improve safety, enhance recruitment and compliance, 2
PEARL, Translational Ethics & Policy,
improve dissemination of results, implement change and help close the translational 130 Evergreen Ave., Imperial Beach,
CA 91932, USA
gap. The model represents robust clinical data from persons of record allowing for 3
PEARL, New York University School
improved interpretation of drug/device side-effects and for regulatory reviewers to of Medicine, Department Obstetrics &
expedite the approval process. Gynecology 180 Varick Street, New York,
NY 10014, USA
Keywords: clinical trials • comparative effectiveness • healthcare infrastructure 4
PEARL, 421First Ave., New York,
• patient-reported outcomes • person-centric • regulatory change NY 10010, USA
5
The EMMES Corp., 401N. Washington
St., Rockville, MD 20850, USA
The US healthcare system is primarily focused this process for as a person he/she can and 6
PEARL New York University,
on managing disease and sickness, whereby a should self-determine and shape their choices 421 First Ave., New York, NY 10010, USA
*Author for correspondence:
person comes to a provider or provider organi- consistent with their self-interest. This shift
Tel.: +1 212998 9219
zation as a patient seeking care and treatment. in mindset moves the person from a perspec- fac3@nyu.edu
This defines the clinical encounter an event tive of sickness to a health-oriented paradigm.
that should be directed at the person/patient Self-determination logically entails personal
but has been compromised with administra- responsibility and is a consequence of a free
tive and financial demands. The incentive society. This is an essential component of
for improved health for some time has been person-centricity. Furthermore, an informed
misdirected, whereby the provider is paid on person is more likely to want to improve their
the basis of what services and procedures are own clinical outcomes and lives by partici-
performed, rather than on the quality or focus pating in clinical studies. This shared inter-
of the condition as well as behavioral changes est is core to the interface of practice-based
to avoid recurrence. Moreover, in many cases, healthcare delivery and in conducting clinical
persons seek medications to essentially allow studies. The person’s participation allows for
themselves to continue to pursue a lifestyle one on one interaction that keeps the person
that created the condition and need for treat- engaged as well as enhances their health lit-
ment in the first place. Additionally, the pro- eracy, transparency and self-determination.
cess is designed to virtually exclude the person This opportunity has obvious benefits to the
(patient) from responsibility in determin- person, clinician and researcher. Integrating
ing their health and treatment. It is, for the real-time clinical care with translational stud-
most part a passive process with the majority ies has profound implications for all stakehold-
responsibility falling on the provider limiting ers in closing the clinical and scientific gap
the clinical encounter with the person. The impacting the nation’s healthcare cost. Apply-
part of
person need not and should not be passive in ing this dynamic person-centric conceptual
10.4155/CLI.14.126 © 2015 Future Science Ltd Clin. Invest. (Lond.) (2015) 5(2), 145–159 ISSN 2041-6792 145Clinical Trial Perspective Curro, Robbins, Naftolin, Grill, Vena & Terracio
framework to the drug development process provides an son and is describing significant differences between the
operational model that includes the ‘person’ thus broad- patient and person. This shift is a significant departure
ening the data input, being inclusive of the person and from the passivity so often associated with the patient
the investigator, on the outcome of the clinical study. component of the doctor-patient (person) relationship
Issues of clinical research such as recruitment, compli- or even that of the consumer. The term consumer was
ance to ensure data integrity and drug safety and loss used for the person to be more discriminative about
to follow-up can be improved by considering the role of healthcare in a competitive market. Models of both
the person. Healthcare delivery manifested at the prac- patient and consumer engagement based thinking do
tice level has many parallels to clinical research and the not account for the complexity and comprehensiveness
‘person’ is pivotal in linking the two venues to optimize of what falls under the broader umbrella of the person.
similar clinical outcomes. Person-centric clinical trials The person who comes to us to seek care, respite, treat-
and its attendant infrastructure can provide a model ment or advice unwillingly becomes transformed into
that will provide real time point-of-use data (live ana- someone other than the person they really are. This
lytics) that will be more robust than that generated in a is seen in managing chronic conditions such as pain.
controlled environment as well as initiate the signaling Each person defines him/herself by their past, their
of drug side-effects, and in the long run, reduce black values, preferences and aspirations. While some may
box warnings. This paper discusses the rationale sup- find this approach ‘too philosophical,’ we contend that
porting the concept of person-centricity and its appli- we have been too un-philosophical by reducing the
cation to clinical research, its transition to healthcare person to how others perceive him/her in terms of a
and education and a proposal to include person-centric particular temporary status they are assigned such as
clinical trials in the clinical drug development program patient reducing the person to a billing number or code
for regulatory approval. Supporting the integration of further distancing the person toward anonymity.
the principles of clinical research to healthcare delivery The cynosure of our model is the person and we
can improve both quality and cost. Additionally, this contend that decision-making must be person-based
paper discusses the employment of a hybrid practice- and driven. People are more likely to change than
based translational network (PBTN) to support person- patients. It must be reflective of how we actually
centricity and to conduct clinical studies that are gen- make decisions rather than some artificially imposed
eralizable and suitable for regulatory submission as well template or construct. All that happens must revolve
as serve as a model infrastructure with the potential to around the person and in this sense rather than speak-
significantly influence healthcare delivery. The need to ing of a person-centered approach we have replaced
improve subject recruitment, accelerate the approval ‘centered’ with the more dynamic term ‘centric’ drawn
process and enhance safety is paramount to contain- from the Greek word sentrikos in which all either
ing cost. The cost/benefit ratio in healthcare is rapidly comes from or to the person as the regulating fulcrum
becoming a worldwide issue as budgets are constrained. as choice and circumstance dictate. Person-centricity
These concerns are exacerbated by rising costs of pre- is a dynamic and transformative concept supporting
ventable lifestyle related illness and non-compliance. the person as the regulating fulcrum from multiple
One attempt to address these multiple factors is illus- pathways to self-determine his/her future, choices and
trated in the Patient Protection and Affordable Care destiny consistent with his/her personal preferences,
Act (ACA) in the USA [1] . This piece of national leg- values, beliefs and aspirations. Engaging as a person
islation affects every citizen personally and financially. rather than a patient profoundly transforms how we
We have used the USA as an example to propose a new perceive and interact with our world around us. The
model that integrates clinical research, healthcare deliv- role of the clinician or health coach or trusted guide
ery and the concept of person-centric clinical trials. would help us define options and make more informed
We believe the model can be applicable for worldwide decisions. The person’s self-determination acutely rep-
healthcare systems reform. The model utilizes an exist- resents the essence of personal involvement and choice
ing infrastructure supporting the ‘person’ and merges much more profoundly than models of consumer or
the principles of clinical research with that of clinical patient empowerment, centeredness, engagement and
practice to create a continuous data base that facilitates activation.
best practice and the regulatory approval process. Previously in our efforts to clarify and define patient-
centered care we realized we needed to take the next
Evolution of patient-centered to step and move from patient to person, consistent with
person-centricity the dynamic and continuous way that is relative to the
The concept of patient-centered is evolving to accom- person’s life space [2] . This shifts the mindset away
modate the distinctiveness and importance of the per- from unidimensional models of consumer or patient
146 Clin. Invest. (Lond.) (2015) 5(2) future science groupPerson-centric clinical trials Clinical Trial Perspective
empowerment, which are too restrictive to accommo- clear. Unlike the research subject, the person is no lon-
date the breadth of the person. Person-centricity pro- ger a passive, anonymous participant without a voice.
motes enhanced decision-making resulting from both Furthermore, if we perform research in a practice-based
self- determination and good counsel from professional context dealing with familiar and known persons in
caregivers while ensuring that healthcare delivery is a given medical practice we can derive results more
consistent with the wishes and best interests of the per- reflective of what actually occurs in persons and popu-
son as they so choose, ultimately defined by the person lations rather than prefiltered subjects with restrictive
himself. This process also minimizes any ethical issues exclusion and inclusion criteria that are unreflective of
that are brought into question as we transition from the real world. The interface of translational studies
healthcare to health by continuously having the person and clinical research poses an opportunity, whereby
in the loop. the concept of person-centricity can be supportive of
We need to move to a more intensive healthcare par- transparency to facilitate the informed consent process
adigm and an immense need to change the trajectory for both clinical care and research. Patient-centricity
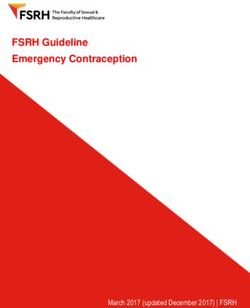
of the aftermath of poor health and healthy behaviors depends upon the triad of self-determination, trans-
in America. We contend that the core of these debates parency and healthcare literacy together supported
must include a rethinking of moving from the patient by an infrastructure that provides the person with the
to the person and changing the debate from discus- information to make an informed or shared decision
sions of sickness and healthcare to health and well- on their health or healthcare outcome (Figure 1) .
being. However, if our ultimate goal is to promote and The clinical drug approval process in the USA con-
sustain healthy living change and have an impact on sists of conducting a study against a placebo allowing
the rising trajectory of health and healthcare related for a large number of drugs available for prescribers to
costs we need to promote a rethinking of personal almost ‘personalize’ treatment. Although not cost-effec-
responsibility and personal choice and of changing the tive it is an advantage for the person and for pharma-
culture of healthcare towards a healthier solution. cological advancement [3] . For the treatment of hyper-
The prescription for health, centers on meaning- tension there are currently eleven therapeutic classes
ful changes in behavior in concert with person-centric totaling 65 antihypertensive medications (American
solutions rather than impersonal ones. This important Heart Association) [4] ; for treatment of diabetes there
person-centric nuance has significant implications for are eight therapeutic classes with a total of 20 diabe-
research as well. The difference between an anonymous tes drugs (American Diabetes Association) [5] ; and for
research subject versus a person is pretty intuitively pain management there are three therapeutic classes
Physical
Differentiating person-centric and patient-centered
Emotional
Mental/behavioral
Spiritual Health/wellness
Physicians
Readiness Personalized prevention
Treatment
Healthcare
Resilience Procedures
Social networks
Endurance Prevention Disease management
Physical and social environment
Mobile devices/telehealth
Self-determination Mobile devices/telehealth
Health literacy Research
Transparency Community infrastructire
Translational network infrastructure
Translational gap
Big data platform
Research/studies
Quality encounter
Comparative effectiveness
Figure 1. Person-centricity creates a more dynamic and involved approach to a person’s health and disease. When a person is
perceived as a patient, the focus is on the disease not the person who becomes passive with little or no participation in their health
and wellness outcomes.
future science group www.future-science.com 147Clinical Trial Perspective Curro, Robbins, Naftolin, Grill, Vena & Terracio
with a total of 74 analgesic drugs with NSAIDs alone PBRNs are survey oriented responding to local prac-
having three therapeutic classes totaling 61 medications titioner interests and for trend analysis and limited in
as an example (Arthritis Foundation) [6] . The numer- conducting clinical studies whose findings are gener-
ous drugs per category allows a prescriber the choice alizable as they do not follow the principles of Good
of a medication ultimately winding up with the most Clinical Practice (GCP).
effective drug that the person is compliant with to This paper addresses the formation of a hybrid net-
take, given the pharmacokinetics and side effects over work model that can conduct clinical studies that are
a period of time. This broad spectrum of choice is seen, generalizable and suitable for regulatory submission
for example, in nonsteroidal analgesics where in one as well as serve as a model infrastructure that has the
chemical class there may reside a number of different potential to change healthcare delivery in the USA and
compounds but each compound has its own effect on significantly influence the health of the nation.
that one person [7] . The wide choice of medications by
some can be construed as a form of personalized medi- Person-centric clinical trials: defining
cine where one can search for the drug with the best fit the N-of-1
or effect for that person. In some cases the multiplicity The ACA centerpiece term of ‘patient-centered care’
of medications defined alternative pathways, for exam- first described in the 1980s is limiting [12] . The term
ple, cox 2 inhibitors, to improve drug development as ‘patient’ places the person in a subservient position
in the case of analgesics and cardio protective medica- and for the most part does not invite or allow them
tions. However, it is the area of clinical outcomes that to participate in their own clinical outcome. Clinical
the focus of drug effectiveness is now manifested in the research now recognizes the importance of the person
term ‘comparative effectiveness research’ (CER). Clini- significantly contributing to their clinical outcome.
cal effectiveness research can be described as primary Having the principal investigator interpret the clinical
referring to direct generation through experimental data is one thing but to have them interpret for the
methodology or secondary by a systematic gathering person interjects a loss of objectivity from the person
and evaluation of primary research information [8] . to contribute to the outcome as to the effect the medi-
Pragmatic trials also measure effectiveness and the cation is having on them. Patient reported outcomes is
benefit the treatment produces in routine clinical prac- now recognized by the FDA and described in a guid-
tice and the term is often used interchangeably. Drug ance document for industry to make label changes of
efficacy in drug development is compared in the USA already marketed drugs [13] . Thus for the purposes of
against a placebo in the early phases and its effective- clinical research the person becomes part of the clini-
ness is determined once approved for market distribu- cal team but in the healthcare context the team sup-
tion in studies termed ‘comparative effectiveness stud- ports the person in challenging assumptions, weighing
ies.’ CER studies have been the mainstay of economies alternatives and identifying or suggesting best prac-
that have fixed cost national formularies such as in tices and best products. After evaluating options alter-
socialized countries in Europe. Every new drug must natives and counsel the person ultimately makes the
show its effectiveness over existing drug(s) in the for- decision. Without the person having ultimate author-
mulary and if approved less effective drugs are removed ity, the team concept is insufficient as a model for
to maintain or limit cost increases. For the purpose of person-centricity. The team can help but not absorb
this manuscript a ‘clinical trial’ is for a study that is part the person as an equal partner for the person always
of a drug development program for regulatory submis- trumps the team. A distinguishing characteristic from
sion and the term ‘clinical study’ is for an approved the clinical research environment where the person
drug in a Phase IV, pharmacovigilance or CER study. does not trump the principal investigator but their
Comparative effectiveness studies to determine best input is considered.
practice for already approved drugs are designed to The N-of-1 defines that ‘one person’ involved in
fit the criteria for practice-based research networks. a clinical trial or study and their clinical outcome
PBRNs were a concept initiated in the UK circa 1900 described for that person (personalized) which can be
and first presented in the USA by Dartmouth Medical summed for all persons in the study for a cumulative
School [9,10] . PBRNs gained interest in the late 70’s and effect. Person-centric clinical trials provides meaning
today there are over 150 PBRNs mainly with central to the N-of-1 study and places limits on the involve-
funding through American Healthcare Research Qual- ment of the person in a study while recognizing the
ity (AHRQ) [11] . The PBRNs work with practitioners in importance of getting directly from the person the
the community and respond to issues and/or questions effect of the drug and not an interpretation by the
raised by the practitioners usually through a medical investigator of that effect. It is inclusive of the person
school, university or health science center. Many of the and refers back to the statement of Hippocrates “It is
148 Clin. Invest. (Lond.) (2015) 5(2) future science groupPerson-centric clinical trials Clinical Trial Perspective
more important to know what sort of person has a disease cost only increases if toxicity is identified in the later
than to know what sort of disease a person has.” stages of clinical development. Incorporating the con-
The personalization of therapeutics although now cept of signaling early on in the clinical program can
being driven by cost and an enhanced understanding only be cost effective. Additionally, drug development
of how human genetic variation affects an individual’s should be including both predictive toxicology and
response to a drug or treatment may prove to be cost pharmacology to maximize cost savings. Many of the
effective. Developing therapeutics aimed at discrete side effects can only be seen at the clinical level, such
groups of patients appear to be particularly timely, as drug distribution and binding, metabolism, sensitiv-
given that an estimated 55% of drugs consumed in ity reactions etc. Any model designed to improve the
the USA, including as many as 80% of approved anti- current system should at least improve recruitment,
cancer therapies are thought to be ineffective in the lessen dropout rate, identify side effects early on in the
patients who receive them [14] . The estimated annual clinical process and allow for better interpretation of
cost for such unwarranted or ‘wasted’ care ranges from those side effects. People recruited from a practice have
$250 billion to $325 billion [15] . The primary goal of known medical histories reducing the subjective inter-
personalized therapeutics is to minimize side effects pretation by the investigator for what are a true drug
and optimize efficacy which will contribute to reduc- side effect and/or adverse event. Long-standing per-
ing healthcare costs. A personalized N-of-1 clinical sons of a practice have a sense of loyalty to the practice,
study requires that providers know intimately the per- which should improve lost-to-follow up and dropout
sons health history and record which is an advantage rates. Engaging the whole practice and their persons to
for practice-based conducted studies. assist in medical advancements only benefits the nation
Traditional definition of the N-of-1 trials in clini- as a whole.
cal medicine are for multiple crossover trials, usually The Patient Centered Outcomes Research Institute
randomized and often blinded, conducted in a single (PCORI) supports the ‘person’ with assuming a level of
patient. N-of-1 trials are a specific form of random- involvement, participation and responsibility for their
ized or balanced designs characterized by periodic treatment outcome in clinical research [20] . Person-
switching from active treatment to placebo or between centricity as applied to clinical studies should improve
active treatments (‘withdrawal-reversal’ designs) [16] . study compliance, a variable for a study considered for
Our definition of ‘person-centric’ as applied to clini- regulatory submission which should be at least 80%.
cal trials is inclusive of the traditional N-of-1 defini- However, the question remains how much compliance
tion. Person-centric clinical studies are a continuum of should there be in healthcare and what should be done
the study by the person beyond the time frame when for a person who is recalcitrant to comply? However,
they come in for data collection. It is the contribution the more meaningful the study is to the person, the
by the person to optimize the clinical study outcomes more likely they are to care about the outcome and
by being an active participant and adhering to study comply accordingly.
compliance. Person-centric clinical trials are exempli- The standards for conducting clinical research are
fied by studies for chronic conditions, studies assess- considered higher than for a practitioner practicing in
ing over-the-counter medications and any ambulatory their offices and the question remains should that be
study which requires the patient to continue the study the case. The difference between the two is that one
in an unsupervised environment. has accountability for treatment in an audit trail for
clinical research and responds to any questions arising
Person-centricity: fulcrum for clinical during the study and in its final assessment, as que-
research & health ries. However, practicing medicine has responsibilities
Patient recruitment is considered the most challeng- beyond the practitioner as it involves the government
ing aspect of conducting a clinical study (Lasagna’s and private payers for reimbursement. The variables
Law) [17] . Equally important is the dropout rates and may differ between clinical research and private prac-
lost-to-follow up for patients can be very costly. Attri- tice but the outcomes should have the same result. The
tion in drug development is still cripplingly high, patient/provider encounter should be defined by qual-
with approximately 16% of the compounds making it ity standards enough for that encounter to be uploaded
through, with toxicity the leading cause at all stages in the ‘big data concept.’ Why should the patient pro-
in the drug development pipeline [18] . It has been esti- vider encounter be any less than any other encounter
mated that a 10% improvement in predicting failure including a clinical research encounter using that as the
before the initiation of expensive and time-consuming gold standard? Accountable care organizations (ACOs)
clinical trials could save upwards of $100 million in involved in overseeing quality of the patient/provider
the costs associated with drug development [19] . This encounter provide administrative oversight designed to
future science group www.future-science.com 149Clinical Trial Perspective Curro, Robbins, Naftolin, Grill, Vena & Terracio
fill a void in the quality of that encounter and adds practice-based studies as they are already marketed
additional cost to the healthcare system. To date there products used for standard of care studies such as CER
are almost 500 public and private models of ACOs, and translational studies moving drugs/devices used
and increasing in number, whose focus is quality but by specialists to primary care providers to increase use
more often they operate on the less is more paradigm and reduce cost. This terminology is more descriptive
trying to limit costs. The goals of ACOs are to improve for the review process by Institutional Review Boards
quality outcomes, improve the experience of care and in facilitating the approval process for PBTN studies.
lower costs. ACO agreements are currently blended
into existing contractual relationships between payers PBTN: infrastructure for change
and providers and differentiate various health plans. The ACA has created to date, as part of the process of
ACOs are provider based where the financial and qual- change, many disparate sources and pieces of what is
ity responsibility lies in the hands of the people who are to become a new healthcare paradigm. In this selec-
delivering the care as opposed to those who are paying tion of the fittest, notwithstanding political lobbyists,
for it [21] . To complicate the matter as of 2012 a US it is hoped that a new healthcare to health system will
News & World Report analysis identified nearly 6000 emerge. Part of this change is the commoditization
health insurance plans marketed to individuals and of healthcare where cost will eventually influence the
their families differing in the types of coverage such as treatment outcome and where patients will be seen by
prescription drugs, maternity, etc. [22] . It is clear that clinics and/or pharmacies designed for screening and
the ‘person’ needs to step up and take control of their categorizing certain conditions from identifying HIV
own health [23] . The variables in private practice are infection to checking fertility levels to giving memory
accountability and controlling costs due in large part tests for early signs of Alzheimer’s by ancillary health-
to defensive medicine, waste, redundancy and espe- care personnel much like the CVS Minute Clinics that
cially fraud estimated to be some 65 billion per year presently exist [27] . The Nation can no longer view
[24] . Additionally, with the concept of ‘big data’ where healthcare as an infinite resource for the treatment of
clinical outcomes are based on a large number of clini- its populace. Moreover there are increasing discussions
cal inputs every person becomes accountable for their of changing our focus from sickness care to ways in
clinical outcome and treatment result [25] . If the con- which we can promote and sustain healthy behaviors
cept of shared decision making and/or responsibility is and lifestyle changes. Whatever shape, form or design
the focus then every person’s encounter, whether it is the new healthcare model takes there will be a need for
for research or an annual visit should be a data point an infrastructure to optimize and support a person’s
with ensured integrity. Such data manifested as clinical healthcare delivery, provide oversight for the treatment
outcomes for the patient would be worthy of real time outcomes, provide a means whereby a person’s data can
input into a ‘big data’ assessment and for its response be utilized for the greater good, provide continued sur-
as best practice at that moment for the patient. Stud- veillance of drugs for improved drug safety programs,
ies conducted for clinical research purposes follow the minimize fraud in the system and not be at odds with
principles of GCP as described in the Code of Federal the healthcare providers. What is this infrastructure
Regulations (CFR) [26] . Incorporating these principles and what role will it have in this new system is still to
into private practice would greatly improve the qual- be determined. We are proposing an infrastructure in
ity of medical records, accountability for treatment this manuscript for consideration and discussion but
by both provider and person which could lessen mal- whatever shape it takes some infrastructure needs to be
practice complaints and limit fraud, and overall set a in place such that persons, providers and payers can go
national standard of care that would be transparent for to for the resolution of treatment outcomes.
every practitioner. The goal would be that every medi- Originally a PBRN was defined as a group of ambu-
cal or healthcare encounter/event would be account- latory practices devoted principally to the primary care
able and usable as data for best practice outcome by a of the person, affiliated with each other (and often
big data platform. The person becomes the fulcrum for with an academic or professional organization) in
research and in health as well as in sickness and they order to investigate questions related to community-
become integral parts for the success of the treatment based practice. PBRNs typically draw on the experi-
outcome. Certainly, if the person is to be included in ence and insight of practicing clinicians to identify and
research protocols from start to finish then they can frame research questions whose answers can improve
be naturally and seamlessly included as part of their the practice of primary care. By linking these questions
own treatment. For our discussion the term subject is with rigorous research methods, the PBRN can pro-
used for a clinical trial describing the various phases duce research findings that are immediately relevant
of drug development. The term patient is used for to the clinician and, in theory, more easily assimilated
150 Clin. Invest. (Lond.) (2015) 5(2) future science groupPerson-centric clinical trials Clinical Trial Perspective
into everyday practice [28] . One aspect of PBRNs that group with the advantages of what a PBRN can deliver
has become a foundation for decision-making in clini- such as patients of record, interested practitioners in
cal practice and health policy are comparative effec- advancing the knowledge base for treatment and data
tiveness reviews. Comparative effectiveness reviews eligible for the ‘big data concept.’ This hybrid network
are summaries of available scientific evidence in which has also modified some terms to clarify its operations
investigators collect, evaluate and synthesize studies and expedite approval by local IRBs. The PEARL
in accordance with an organized, structured, explicit Network is the first PBTN built on the principles of
and transparent methodology. They provide clinicians GCP such that the studies it conducts are in compli-
with scientifically rigorous information for compar- ance with regulatory agencies and can be submitted to
ing the effectiveness and safety of alternative clinical satisfy drug development requirements primarily in
options. Further, they approach the evidence from a the spaces of Phase III and Phase IV. Design of stud-
patient-centered perspective; explore the clinical logic ies allows for the persons to have input in accordance
underlying the rationale for a service; cast a broad net with the FDA guidance document for patient reported
with respect to evidence; assure internal validity; and, outcomes including quality of life for person-centric
present benefits and harms for treatment and tests in assessment. N-of-1 person-centric clinical trials can
a consistent way [29] . The two operational phrases are be grouped by treatments since they are standard of
‘scientifically rigorous’ and ‘internal validity’ which care for equipoise and adopted to implement creative
becomes somewhat difficult to assure in a review. A changes in clinical design. Equipoise is reached when
network capable of conducting the study itself can a rational, informed person has no preference between
assure the science and validity of the data and when the two (or more) available treatments [31] .
practitioners generate the data than they have the con- PEARL has conducted some 20 studies over the
fidence to incorporate change in their practices. For a funding period ranging from observational, retrospec-
network to conduct a study to satisfy the above criteria tive, prospective and randomized controlled clinical
as well as generalizability it must have an infrastructure studies and has partnered/affiliated with other medi-
to ensure data integrity. cal/dental based PBRNs. It is presently conducting
The Practitioners Engaged in Applied Research & a practitioner/patient survey study with the FDA to
Learning (PEARL) Network was designed to incorpo- assess the use of an Opioid Patient Provider Agreement.
rate ‘rigorous research methods’ into the private prac- A designed infrastructure for healthcare can provide
tice setting by following the principals of GCP and regulatory agencies with assistance in their initiatives
screening and educating practitioners to conduct clini- to protect the populace. The FDAs Safe Use Initiative
cal studies capable for regulatory submission which is an example of how large-scale practitioner input can
is the benchmark for internal validity and rigorous make a difference in the amount of data collected to
research methods. Since the studies conducted are pri- make meaningful decisions [32] . The largest study to
marily standard of care the word ‘research’ was changed date that PEARL has conducted consisted of almost
to ‘translational’ as it is more relevant and descriptive 1900 patients and for the randomized controlled clini-
since the goal is to have the findings assimilated into cal studies it conducted had a patient compliance rate
everyday practice as well as technology translated from as high as 98%. The advantage of PEARL lies in its
specialists to primary care physicians. Other changes ability to recruit highly motivated practitioners who
include use of the term ‘person’ instead of subject and are screened to ensure no licensure limitations, recruit
defining the use of clinical trial versus clinical study. long-standing patients of record that have a known
Standard of care in this context is defined as the use of medical history to identify early side effects (signaling)
a drug, device or treatment that has regulatory approval and provide real-use data, which is more robust than
and a risk profile for use in ambulatory persons. that generated from a controlled environment.
The PEARL Network was initiated as a grant pro- PEARL’s scope broadened when it moved beyond
posal funded by the NIDCR/NIH in 2005 and was its origin and roots in dentistry to an interdisciplinary
supported for a total of 7 years [30] . The objective of the practice-based network which has expanded its infra-
grant was to build a Practice Based Research Network structure into healthcare with a published philosophy
(PBRN) for the dental profession similar to medi- based on the concept of Person-Centricity conduct-
cal PBRNs that were supported by AHRQ. The one ing Person-Centric Clinical Trials [33] . The PEARL
exception and point of differentiation was that the data infrastructure allows for every clinical encounter to be
generated by PEARL was to be ‘generalizable’ and that considered a data point [8] . PEARL is an added value
the practitioners be continuously engaged. entity that brings together persons and practitioners
The infrastructure of PEARL is designed by merg- with entities interested in advancing healthcare such
ing the merits of a pharmaceutical industry clinical as academic centers, payers and the pharmaceutical
future science group www.future-science.com 151Clinical Trial Perspective Curro, Robbins, Naftolin, Grill, Vena & Terracio
industry. The pivotal component of the model is that clinical testing process and accelerating the continu-
practitioners are themselves generating the data allow- ous process of drug safety especially by having a study
ing for them to be their own best advocate for change become a part of the sentinel program benefiting both
within their office environment. The collaboration the regulatory agency by early detection of side effects
may reduce the translational gap, allow academic cen- and the pharmaceutical company by lessening liability
ters to market a real-time curriculum reflective of treat- after the drug is marketed. In 2007, Congress passed
ments based on clinical evidence, develop a pool of the FDA Amendments Act (FDAAA), mandating the
practitioners interested in becoming faculty members, FDA to establish an active surveillance system for
benchmarking of the practitioners who participate in monitoring drugs, using electronic data from health-
a clinical study to improve their skills, conduct CER care information holders. The FDA launched the Sen-
studies, provide information dissemination to both tinel Initiative with the goal to build and implement
practitioners and patients and function as the infra- an active surveillance system that will eventually be
structure for healthcare delivery based on the principles used to monitor all FDA-regulated products. The
of Person-Centricity: self-determination, transparency program, it is hoped, may reduce the size and scope
and healthcare literacy. of late stage clinical trials and of post-approval stud-
PBTN creates an opportunity for continuous learn- ies consistent with the goals of person-centric clinical
ing for both clinicians and students. If students are studies [35] .
trained with the concept of quality integrated into The current system of the clinical trial approval pro-
each encounter, it is a natural next step to base deci- cess resides in negotiating with the regulatory agency
sions on patient specific measures. Providers trained on the design of the Phase III studies. Currently two
with the understanding that every person has a basic randomized controlled clinical trials are required to
right to n = 1 treatment, beyond the public health establish safety and efficacy. The safety component is
prevention model which would support the founda- continuous and on-going but may be missed in a con-
tion of a healthy community. The individual’s health trolled study that is limited and does not reflect real
responsibility needs to be acknowledged, translated use data. The efficacy component as well may not be
and communicated for improved outcomes. To accom- reflective of real use as every aspect of the study is opti-
plish this, there is a need for collaboration throughout mized and controlled from the investigator, patient and
the health industry beginning with the schools. Cli- healthcare environment, again not reflective of how the
nicians practicing under the concept proposed should drug may be ultimately used in a practice setting. The
strengthen the educational aspect of training for both randomized controlled trial (RCT) designs and hege-
shared decision making and a quality person provider mony around systematic reviews have worked well to
encounter. Generating continuous data for improve- create an initial body of research but have not worked
ment in both treatment and healthcare delivery would for producing replicable results that matter or trans-
produce a more concerned provider and in the process late [36] . The system that has been built stifles creativity
create a reservoir of potential clinical faculty for the and thinking by holding that efficacy RCTs are always
medical center [34] . the highest or only type of evidence considered [37] .
The infrastructure of a PBTN can function as the
Person-centric clinical trials: drug operational structure to suggest some changes and
development, regulatory change & early improvements in the Phase III and IV requirements
signaling for drug safety of the clinical development process. For the Phase IV
Accelerating the time frame and improving the qual- postmarketing commitment that a company has with
ity of clinical trials has been an elusive but sought a regulatory agency to conduct drug safety surveillance
after goal and the profession/industry has not chal- reported by the annual reports having a network that
lenged the present model proposed by regulatory providers can continuously monitor their patients and
agencies. Change can be limiting as the temporal and be discriminative about the quality of the drug side
side effects of the drug can vary. The pharmaceutical effects becomes essential to data integrity support-
companies are not in a position to challenge govern- ing the package insert and in monitoring of the drug.
ment agencies as they oversee every aspect of the drug The percentage of marketed drugs approved and out
being approved as well as marketed. Change in the of Phase IV compliance is estimated to be more than
clinical drug development process can be in quality 70% [38] . Pharmaceutical companies will be able to
of the data collected, improvement in patient recruit- complete their Phase IV commitments and be in com-
ment and in the kind of patients being recruited to the pliance with government agencies. Phase IV studies on
study, the ability to collect robust data in real-time, the already approved drugs become standard of care are in
ability to improve ‘signaling’ of side effects during the the domain of a PBTN.
152 Clin. Invest. (Lond.) (2015) 5(2) future science groupPerson-centric clinical trials Clinical Trial Perspective
The process of a Phase III commitment becomes trolled by the principles of GCP, and most likely will
contingent upon the risk potential of the drug, predic- identify drug side effects earlier compliant with the
tive pharmacology of the molecule and overall safety FDA sentinel program and lessen postmarketing issues
of the drug to be allowed use in a practice setting. We for the pharmaceutical industry. Safety is the essential
are suggesting that a more robust presentation of the directive for a study to be considered for a practice-
safety and efficacy of the drug being reviewed by regu- based network. The combination for one randomized
latory agencies would be better served by conducting controlled clinical study plus a practice-based clini-
one traditional randomized clinical trial and the sec- cal study offers advantages over the existing protocol
ond study to be conducted by a GCP practice-based for drug development for regulatory agencies such as
network. Variations of this combination of studies can the FDA. The model should shorten the clinical time
be further constructed with the PBTN study eventu- in development, identify side effects more efficiently,
ally confirming the robustness of the RCT data gener- make practitioners aware of the drug prior to market
ated. A practice-based network study can be viewed as and be cost effective by reducing the size of the RCT
the antithesis of the RCT in that it uses a large number Phase III studies due to their broad based clinical
of investigators each recruiting a relatively small num- design to capture adverse side effects.
ber of patients, whereas the RCT uses a small number Operationally a practice-based translational study
of investigators each recruiting a large number of sub- requires a central infrastructure to ensure that regu-
jects. During the early phases of drug development the latory requirements are being adhered to, protocol
RCT takes precedence but for later phases of clinical compliance is maintained such as randomization and
development where a large amount of safety and robust patient blinding. Randomization is best performed by
point of use data can be generated the pendulum shifts the data coordinating center but can be done with an
to conducting a PBTN study (Table 1) . The same prin- experienced site. Some studies randomize the sites if
ciples (GCP) apply to limit bias and ensure data integ- the outcome is based on a procedure, device or a spe-
rity as in an RCT study. cific drug that a physician may prescribe. The bound-
PBTN clinical studies can be viewed as comple- ary parameter for a PBTN study is standard of care.
mentary to the traditional RCT and of adding value Patients are asked if they want to participate in a study
in generating a large robust dataset that is quality con- and each patient is formally enrolled as per the proto-
Table 1. Relative differences between the operations of a randomized controlled clinical trial versus
practice-based translational network conducted clinical trial.
RCT PBTN
Number Investigators Limited Less limited
Sample size Smaller Larger
Population Restricted Broader base
Medical history Not always known Typically known
Clinical outcome Efficacy Efficacy/effectiveness
Generalizability Lesser Greater
Data source Controlled Point-of-care
Data integrity GCP procedures GCP procedures
Bias prevention Blinding Blinding (patient and practice
level)
Outcomes Limited Broader
Type of study Investigator centered Person-centered
Scope of study Low margin of drug safety High margin of drug safety
Safety data Limited Broad
Adverse drug reactions/events Many unexplained Explained/known history
Screen failures Greater Lesser
Recruitment Public Practice
Study commitment/compliance Lesser Greater
GCP: Good Clinical Practice; PBTN: Practice-based translational network; RCT: Randomized controlled trial.
future science group www.future-science.com 153Clinical Trial Perspective Curro, Robbins, Naftolin, Grill, Vena & Terracio
col. Blinding of the study is best ensured by the data chronic conditions, with considerable savings to the
coordinating center but can be performed by the site as healthcare system [3] .
well as a caregiver, for example, a caregiver can place The magnitude of all these moving parts requires a
pills in numbered envelopes to be opened on consecu- robust infrastructure to support them and maximize
tive days maintaining the blind. The infrastructure the patient/provider encounter. Healthcare plans dif-
is always present to support operational steps that are fer in the number of minutes allowed for patient face
protocol specific. Persons can be monitored through time with the provider and even that is questionable
mobile health technology and even by remote entry of as they are mostly looking at a computer screen. Pro-
their improvement and/or worsening of their condi- vider time can be available directly, via phone and/or
tion. The infrastrucuture with clinical research asso- telemedicine and by mobile health (m-Health) devices
ciates can ensure the proper oversight of the patient. for 24/7 monitoring whereby the information can be
Data integrity and all the controls associated with an summarized on a daily, weekly or monthly basis for
RCT are in place for a PBTN study such as queries transmission to the practitioner. Infrastructures such
and close-out procedures. Bias is minimized by the as Kaiser Permanente which is a closed healthcare sys-
same blinding procedures that would be applicable to tem approaches such an infrastructure but do not opti-
an RCT at either the patient or practice level with the mize the person/provider encounter to the level of a
infrastructure overseeing compliance. data point.
Person-centric clinical trials: optimizing Person-centric clinical trials: managing
chronic disease outcomes big data
The concept of person-centricity is best exemplified The ‘Big Data’ concept or a National Medical Grid as
by an individual diagnosed with a chronic condition the repository for healthcare data and treatment out-
where they themselves become pivotal in shaping the comes is a concept used to align the many moving parts
outcome of their condition and future [39] . The role of the system. However, this requires an infrastruc-
of the person mandates moving beyond the passivity ture to ensure that the data going into the system has
of the patient to the self determination of the person been vetted and meets the conditions of data integrity
reflected in their own treatment choices and desired and verification. This is the basis for optimizing the
outcome, essential to optimizing person-centricity. It patient–provider encounter satisfying the parameters
places the person in the forefront of accountability of a data point making this point worthy of being part
and responsibility for compliance of their treatment, of the big data platform. Encounters based on quantity
behavioral modifications to make substantive changes over quality can be misleading for a person wanting
in their lifestyle, which led up to their condition in to participate in the program and expecting a quality
the first place and initiates the process of the person decision from their provider on the best practice treat-
thinking about their health rather than their condi- ment for their condition which may or may not be evi-
tion. Healthcare today is directed toward chronic dence based at that moment. The data would become
treatment and essentially maintaining the status quo ‘evidence based’ as the data trends and would be most
of the person allowing them to continue to pursue a evident when presented as a comparative effectiveness
life style without changing the underlying causative study otherwise the data are presented to the patient
factors to alter the course of the disease process and/ as ‘best practice’ at that moment in time. A subtle but
or maximize the treatment prescribed. Obesity and its distinguishing feature between the terms best practice
sequelae such as hypertension and diabetes are obvious and evidence based. The ethics of practitioners recruit-
examples where the philosophy of person-centricity ing persons (patients) to such studies has been recently
can alter significantly the outcome of the treatment. reported on in the literature [24] .
This also produces a halo effect for the people around The concept of a ‘Big Data’ platform or medical
this person and directly and mutually benefits, for cloud or ‘National Medical Grid’ is consistent with
example, not only the person but the family and com- closing the translational gap. The idea of designing a
munity. Family support as reported by the Institute practical framework that allows for real time compari-
of Medicine can be very influential and cost effective son of clinical outcomes creates a portal for the latest
for the Nation in managing a chronic condition [40] . information to be incorporated into healthcare and
Other conditions such as chronic pain, drug addic- would facilitate change. The infrastructure is essential
tion and depression may have an improved outcome for responsible sharing of clinical trial data [41] .
under person-centricity in conjunction with family The use surveys and administrative datasets for pol-
support and behavioral intervention. The N-of-1 trials icy analysis and policy development is an important
as defined by person-centric are particularly suited for first step in decision making about how to best spend
154 Clin. Invest. (Lond.) (2015) 5(2) future science groupPerson-centric clinical trials Clinical Trial Perspective
healthcare dollars. However, the process requires a basis for person-centric healthcare relies on the same
level of consistency in terminology across all healthcare foundation as person-centric clinical trials: transpar-
disciplines [41] . Whatever the format, it is the quality ency, healthcare literacy and self-determination as well
of the input that we are discussing when applying the as having an infrastructure to support the ‘person’ on
philosophy of person-centricity. its foundation. This shifting of healthcare on indi-
Point-of-use data generated by a GCP practice-based vidual self-reliance rather than on medical paternalism
network as well as administrative and claims datasets is consistent with the essence of person-centricity and
have a role to play in the conduct of CER provided consistent with the American principles. The concept
the data has been subjected to some standard of qual- is transformative in that the person is no longer passive
ity assurance. The use of CER is an important strat- in the process but becomes their advocate for them-
egy to improve health outcomes decisions and balance selves to improve their own clinical outcome. This
healthcare spending. The potential pitfall of CER is truly the N = 1 or what personalized medicine or
is that if policy makers and benefit providers (in an care should be, going beyond the traditional definition
attempt to contain costs) use CER-generated results to reserved for medicine, related to personalized drug
choose services based on price alone, they may restrict development. Person-centric healthcare as it relates
patient access to necessary care [42] . Providing an infra- to personalized medicine embodies not only the drug
structure to function as a scaffold for healthcare can development component but the ‘persons’ active role in
improve data quality and utility and be the interface the treatment to make it ‘personalized’ and to improve
to research [43] . their health.
Large healthcare datasets primarily consist of claims Making each person – encounter a quality encoun-
and/or hospital datasets that are based on diagnosis ter as governed by the principles of GCP can be cost
codes. They lack objective point-of-use data such as effective and streamline a number of organizations
person (patient) reported outcomes, disease activity that have been built on top of this encounter. The
and other measures of health, that could be provided principles of GCP can be the common thread of qual-
by a GCP PBTN/PBRN. ity that creates an audit trail to minimize redundancy
Currently ACOs are limited to claims and diagnosis of treatment, overtreatment, treatment of a question-
data, and use administrative datasets to measure out- able nature and healthcare fraud. Practicing at a level
comes. These administrative datasets are a proxy for below GCP where the encounter now becomes less
point of use data. The hundreds of ACOs around the than acceptable as a data point compromises the data
country attempt to measure quality of care, accepting inclusion into the Big Data platform, requiring vari-
the limits of existing infrastructures and by relying on ous levels of oversight to ensure ‘some level of quality.’
administrative data. A GCP infrastructure would provide practitioners
the ability to integrate research principles for quality
Person-centric clinical trials: transition improvement [44] .
to healthcare for collaboration between A coordinated effort by all stakeholders could lead
person, provider, payer & industry to a meaningful, cost-effective and within-reason,
The current healthcare system is not sustainable and a profitable healthcare system for all stakeholders.
does not adequately consider all of the variables from Healthcare has not made use of the efficiency and
the person, provider, payer and the pharmaceutical economy of scale that it requires if the system is to be
industry and their common interests. To unravel this meaningful, lean and efficient. Healthcare plans differ
complex system would be a burdensome task for any on face time that the person has with the provider with
individual. The attempt to re-direct healthcare to the some so limited that you are encouraged to see some-
‘person’ through the ACA may be the path of least one other than the primary care physician. In a mini-
resistance. The many disparate parts of the health- mal time period one is to familiarize themselves with
care system do not even communicate with each other the person by reviewing the past medical history, listen
making improvements and optimization very diffi- to the person for their chief complaint, examine the
cult if not impossible. The concept of expanding the person, assess the person and findings and make a deci-
principles of person-centric clinical trials to person- sion on treatment. Would it not be better to build the
centric healthcare and providing an infrastructure of quality up front within the encounter and limit all of
inclusion for all stakeholders is an approach which can these points of potential problems on the quality of the
only benefit each person and the community at large. encounter? Differences in quality can be seen in the
Person-centric healthcare shifts the healthcare cost current system as variability in comparative datasets
curve so that the person assumes some accountability ([Electronic Health Record] vs claims data) have dif-
and responsibility for their treatment outcomes. The ferent end points but should be complementary to each
future science group www.future-science.com 155You can also read