Periodontitis as potential risk factor for Alzheimer's disease
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
RESEARCH REVIEW 121
Ghazal Aarabi, Götz Thomalla, Carolin Walther, Carola Mayer, Thomas Beikler, Guido Heydecke,
Udo Seedorf*
Periodontitis as potential risk
factor for Alzheimer’s disease
Introduction: Neuroinflammation is a hallmark of Alzheimer’s disease (AD).
Multiple infectious agents have been demonstrated in the brain and proposed
to be involved in AD, but robust evidence of causation has not yet been
established. It was hypothesized that periodontitis (PD) and infection with
Porphyromonas gingivalis may be linked to onset and progression of AD.
Although inflammation is present in both diseases, the exact mechanisms and
interactions between periodontitis and AD are poorly understood.
Method: In this narrative review, we highlight recent progress in exploring
potential associations of PD with AD and its surrogates (amyloid plaques) and
clinical sequelae (i.e. dementia), respectively.
Discussion and Result: Recent evidence suggests that periodontitis interacts
with AD to increase the severity of clinical dementia and to accelerate its mani-
festations. These results indicate that periodontitis may be an emerging risk
factor for AD and that the risk may be mediated directly by Porphyromonas
gingivalis and its secreted neurotoxic gingipains. The recent development of an
oral gingipain inhibitor, which is currently tested in a randomized controlled
trial, offers the unique opportunity to verify the infectious hypothesis of AD. If
successful, this research can be expected to result in a significant improvement
of prevention and treatment of PD and AD.
Keywords: periodontitis; Alzheimer‘s disease; Porphyromonas gingivalis;
gingipain; neuroinflammation; dementia; oral prophylaxis; therapy
Department of Prosthetic Dentistry, Center for Dental and Oral Medicine, University Medical Center Hamburg-Eppendorf, Germany: PD Dr. Ghazal Aarabi, Dr. Carolin
Walther, Prof. Dr. Guido Heydecke, Prof. Dr. Udo Seedorf
Department of Neurology, Head- and Neurocenter, University Medical Center Hamburg-Eppendorf, Germany: Prof. Dr. Götz Thomalla, Carola Meyer
Department of Periodontics, Preventive and Restorative Dentistry, University Medical Center Hamburg-Eppendorf, Germany: Prof. Dr. Thomas Beikler
* Corresponding Author
Citation: Aarabi G, Thomalla G, Walther C, Mayer C, Beikler T, Heydecke G, Seedorf U: Periodontitis as potential risk factor for Alzheimer’s disease. Dtsch Zahnärztl Z Int 2021;
3: 121–128
Peer-reviewed article: submitted: 15.04.2020, revised version accepted: 22.06.2020
DOI.org/10.3238/dzz-int.2021.0014
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)AARABI, THOMALLA, WALTHER ET AL.:
122 Periodontitis as potential risk factor for Alzheimer’s disease
(Fig. 1: Ishii, 2014 [17], reprinted with permission from the American Journal of Neuroradiology, AJNR)
Figure 1 Diagnosis of Alzheimer’s disease by non-invasive imaging. Left: Healthy elderly male subject, age: 78 years, Mini-Mental
State Examination score: 30. (A) Note the slightly enlarged right inferior horn of the lateral ventricle on the T1-weighted MR image.
(B) Note that the regional glucose metabolism is not reduced on the FDG-PET images. Note that glucose metabolism in the posterior
cingulate is much larger than that in other regions. (C) PiB-PET reveals nonspecific accumulation in the white matter but no PiB ac-
cumulation in the gray matter. The amyloid deposit is negative. Right: Patient with early Alzheimer’s disease, age: 77 years, Mini-
Mental State Examination score: 25. (A) Note the slight atrophy of the right hippocampus. (B) FDG-PET reveals diminished glucose
metabolism in the bilateral parietotemporal association cortices and posterior cingulate gyri and precuneus. (C) PiB accumulation is
seen in the cerebral cortices except for the occipital and medial temporal regions. High PiB accumulation is present in the medial
parietal and frontal regions, indicative of positive amyloid deposit [17].
FDG = [18F]-fluorodeoxyglucose; PET = positron emission tomography; PiB = Pittsburgh Compound.
Introduction ually lost. The most common forms lin 1 (PSEN1), and presenilin 2
In Germany, approximately 1.2 mil- are Alzheimer‘s disease (AD) and vas- (PSEN2). Together, these mutations
lion mostly elderly people suffer from cular dementia, which together ac- explain only 5–10 % of the occur-
dementia (GDB 2016 Dementia Col- count for approximately 85 % of all rence of early-onset AD (reviewed by
laborators, 2019). The number of cases [14]. While AD is caused by pro- [45].
people living with dementia has in- tein deposits called amyloid plaques Previous research supports that
creased significantly in the last 3 de- or senile plaques in the brain (Fig. 1), chronic inflammatory processes play
cades due to ageing. Despite of some vascular dementia is due to a circula- a pivotal role in AD dementia [24, 43,
evidence of minor decreases in the tory disorder resulting in a dimin- 49]; but the events that trigger in-
age-specific incidence rates [48], ished cerebral oxygen supply. Well es- flammation in the first place are still
further increases in the number of tablished risk factors for vascular de- unclear. One repeatedly postulated
people affected by dementia may be mentia are hypertension, heart dis- possibility is that AD associated in-
expected due to the prevailing demo- ease, diabetes, high cholesterol levels flammation may result from an infec-
graphic trends. Limited starting (hyperlipidemia), obesity, physical in- tious etiology [31]. Multiple infec-
points for prevention and the ab- activity, and smoking [12]. Age and tious agents, including Cytomega-
sence of an effective treatment sug- the ε4 allele of apolipoprotein E are lovirus (CMV), herpes simplex virus
gest that the dementia-related burden major established risk factors for the types 1 and 2 (HSV-1, HSV-2), Heli-
on patients, caregivers, and the frequent multifactorial forms of AD cobacter pylori, Chlamydophila pneu-
health-care system will likely con- [12]. In addition, rarer familial forms moniae, Borrelia burgdorferi, and Por-
tinue to rise. exist, which are primarily due to phyromonas gingivalis have been dem-
Dementia is a neurodegenerative high-penetrance mutations in amy- onstrated in the brain and proposed
disease in which neurons are grad- loid precursor protein (APP), preseni- to be involved in AD, but robust evi-
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)AARABI, THOMALLA, WALTHER ET AL.:
Periodontitis as potential risk factor for Alzheimer’s disease 123
dence of causation has not yet been was discussed comprehensively in a apical OR periapical abscess, Porphyro-
established [28, 37]. Extracellular recent review by Aarabi et al. [1]. monas gingivalis, Porphyromonas endo-
amyloid-β (Aβ) deposits, which ac- Thus, this narrative review aims at dentalis, Streptococcus mutans, GroEL,
cumulate in the gray matter of the presenting and evaluating recent lipopolysaccharide. 2) Neurology: Alz-
brain, are a hallmark of the AD. It progress in exploring potential associ- heimer’s disease, dementia, cognitive
could be demonstrated Aβ belongs to ations of infections with Porphyro- decline, brain, amyloid plaques or
an evolutionarily conserved family of monas gingivalis with AD and its clini- senile plaques, magnetic resonance
proteins, collectively known as anti- cal sequelae, i.e. dementia and mild imaging OR tomography, CT OR
microbial peptides (AMPs) [19, 39]. cognitive impairment (MCI). In AD, computer tomography. 3) Inflam-
AMPs act as a first-line of defense PD was shown to be associated with mation: autoimmunity, C-reactive
against a large range of pathogens increased dementia severity and protein OR CRP, interleukin, peri-
including bacteria, mycobacteria, vi- more pronounced cognitive decline, odontitis, oral infection, systemic
ruses, fungi, and protozoans [47]. thus indicating a link to an increased inflammation, acute phase, endothe-
Mice lacking the amyloid precursor systemic pro-inflammatory state [15]. lial AND function OR dysfunction.
protein (APP) show an attenuated An example of a case of severe gen- Other: epidemiology.
survival rate after bacterial infection eralized PD is shown in Figure 2. Search terms of each subject area
and it is assumed that oligomer- were combined logically and resulted
ization and fibrillization is required Methodology in 230 hits, which were recorded and
for Aβ‘s antimicrobial activity [25]. The search strategy for this review screened by GA and US manually and
The recent finding that Aβ has anti- was developed in view of our aim to categorized a priori relevant or inter-
microbial activity has motivated the find and present recent evidence sup- esting. Excluded were non-peer-re-
scientific community to verify a pos- porting an infectious etiology of AD viewed studies and studies with in-
sible infectious cause of AD [25, 39, and the potential contribution of Por- sufficient sample sizes to yield at least
40]. It was hypothesized that peri- phyromonas gingivalis to AD and its a statistical power of 80 % to detect
odontitis (PD) and infection with clinical sequelae, i.e. dementia and the claimed effects. Also studies that
Porphyromonas gingivalis may be mild cognitive impairment (MCI). were prone to the possibility of re-
linked to onset and progression of The literature search was restricted to verse causation (typically case-con-
AD. Although inflammation is pres- PubMed, PMC (NCBI) and Web of trol studies comparing the frequency
ent in both diseases, the exact mech- Science SCI with the following search of periodontitis in healthy subjects
anisms and interactions between PD terms: 1) Oral medicine: oral infec- and dementia patients) were ex-
and AD are poorly understood. The tion, periodontitis, gingivitis, bleed- cluded (18 publications). Animal
impact of inflammation on vascular ing on probing, gum disease, tooth- studies that had no direct relation-
dementia and its association with PD loss, endodontic lesion OR infection, ship to human AD (21 publications),
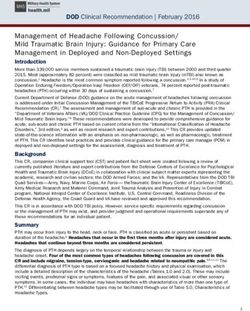
(Fig. 2: T. Beikler)
Figure 2 Example of severe periodontitis with the typical presentation of loss of alveolar bone. The x-ray shows teeth exhibiting
generalized severe bone loss of 30–80 %. The red line marks the actually existing bone level. The green line shows where the original
bone level was before the patient developed periodontitis. Periodontitis is an inflammatory disease and Porphyromonas gingivalis as
well as a number of other mostly Gram-negative anaerobe bacteria play a key role in its pathogenesis.
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)AARABI, THOMALLA, WALTHER ET AL.:
124 Periodontitis as potential risk factor for Alzheimer’s disease
and studies that concerned with nitive decline [21]. Gatz et al. evalu- In general, the blood-brain bar-
dementia rather than with AD ated data from the Swedish Twin rier protects the brain against expo-
(146 publications) were also ex- Registry to identify potentially mod- sure to bacteria and other toxic
cluded. This prescreening procedure ifiable risk factors for AD. The most agents. However, there are 2 main
resulted in 45 proposed references consistent risk factor for AD was routes via which bacteria may cross
(98.3 % agreement between both tooth loss before the age of 35. Low an impaired blood-brain barrier and
authors, Cohen’s kappa: 0.95), which educational status also associated enter the brain: first, by bacteremia
were stored in an Endnote web data- with the risk for dementia and lack and second, by migrating along the
base that was accessible to all au- of physical exercise associated with trigeminal nerve (mouth brain axis)
thors, who decided consensually the risk for non-Alzheimer’s demen- [34, 43]. Pro-inflammatory cytokines
which publication should be refer- tia [9]. However, tooth loss is a poor that are triggered by Porphyromonas
enced based on the article’s content outcome measure because tooth loss gingivalis and other periodontal
(41 publications) and 8 additional may have an adverse influence on pathogens are secreted from the in-
references resulting from manual diet. Thus, a poor diet and not the fected sites at the periodontium,
searches were added during peer- periodontal inflammation per se may enter the blood stream and reach the
reviewing. This procedure resulted have been the causal factor under- brain via the circulation and weaken
in the 49 references cited in this re- lying the observed association in the blood-brain barrier by inducing
view. these studies. a proinflammatory state favoring
The hypothesis that PD may be cerebral small vessel disease (CSVD).
Association between associated with Aβ deposits in the Moreover, Porphyromonas gingivalis
chronic oral infections and brain was also investigated by posi- can infect endothelial cells and
dementias tron emission tomography imaging, stimulate the expression of endothe-
Chronic oral infections such as PD which enabled non-invasive im- lial adhesion molecules, which may
may be able to modulate the risk of aging of these deposits [20]. The promote monocyte/macrophage ad-
AD dementia. In the Third National study included 38 healthy elderly hesion and infiltration into the en-
Health and Nutrition Examination men and women. After adjusting dothelial layer of the blood-brain
Survey (NHANES-III), a large repre- for confounders, clinical attachment barrier [46]. Thus, infections with
sentative cross sectional observatio- loss of ≥ 3 mm was associated with Porphyromonas gingivalis may con-
nal study among 2,355 participants elevated Aβ in affected brain regions tribute to the destruction of the
≥ 60 years of age, PD was associated (p = 0.002) [20]. There are a number blood-brain barrier via inflammation
with cognitive decline, which is con- of additional studies that supported during CSVD. Imaging markers of
sidered to be a precursor of dementia an association between dementia CSVD were found to be associated
[30]. However, the type of dementia and periodontal disease or tooth loss with cognitive decline in elderly
was not assessed and brain MRI was (reviewed by [44]). Although these people affected by AD [7, 8]. The
not available for the study. A re- studies had limitations, such as subgingival biofilm is composed
duced number of teeth – a frequent small sample sizes, lack of rigorous mostly of lipopolysaccharide (LPS)-
cause of a past PD – increased the criteria to diagnose PD and differ- producing Gram-negative bacteria
risk of higher prevalence and inci- entiate between different types of [38], some of which can trigger in-
dence of dementia of all causes in dementia, and the possibility of re- flammatory responses in the brain
the Nun Study [27, 41]. The Nun verse causation, the evidence for an [2], damage the blood-brain barrier
Study is a longitudinal survey on association between PD and demen- in animal models of AD [18], and
aging and AD of nearly 700 nuns tia or AD nevertheless appears to be stimulate the production of Aβ pep-
from across the United States. Its rather solid, thus raising questions tides by neurons [26]. Porphyromonas
strength relates to the fact that AD about possible mechanisms under- gingivalis has the ability to impair
diagnosis was performed post mortem lying these findings. the blood-brain barrier by gingipain-
to ensure a high sensitivity and spe- mediated degradation of the junc-
cificity of the AD diagnosis. In addi- How periodontal pathogenic tional adhesion molecule (JAM1), a
tion, the dental records were com- bacteria cross blood-brain tight junction–associated protein
plemented with results from cogni- barriers that regulates the epithelial barrier
tive tests longitudinally over a long Key pathogens involved in the path- function [42]. Gingipains cleave
period of time. ogenesis of PD are, amongst others, JAM1 specifically at residues K134
Data from the U.S. Department Porphyromonas gingivalis and Trepo- and R234, resulting in permeability
of Veterans Affairs Dental Longi- nema denticola [23], which colonize of the epithelium to LPS, and pro-
tudinal Study (VA-DLS) of almost deep periodontal pockets. Serum IgG teoglycan (PGN). Knockdown of
600 men aged 28 to 70 at entry who antibody levels to Porphyromonas gin- JAM1 in cultured cells increased the
had been followed for up to 32 years givalis were shown to be associated permeability to LPS, PGN, and gingi-
showed that the risk of cognitive de- with an increased incidence of AD pains [42]. Thus, bacterial toxins
cline increased with the number of and AD progression [30, 41], sug- may be able to penetrate the brain
lost teeth and that also PD and car- gesting an involvement of Porphyro- via the damaged blood-brain barrier.
ies lesions were associated with cog- monas gingivalis in AD. Moreover, oral bacteria may access
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)AARABI, THOMALLA, WALTHER ET AL.:
Periodontitis as potential risk factor for Alzheimer’s disease 125
the brain via infection of monocytes chinery. It could be demonstrated, [13], suggesting that the integrity of
followed by brain recruitment [5, 11] for instance, that the rabies virus the trigeminal nerve, which may be
or direct infection of endothelial enters the central nervous system by impaired by oral infections, is cru-
cells, which protect the blood-brain retrograde axoplasmic flow [29], the cial for these brain functions. Oral
barrier [36]. tetanus neurotoxin is retrogradely infection of ApoE knockout mice
Passage through the trigeminal transported towards the soma in sig- with Porphyromonas gingivalis led to
nerve is supported by the observa- naling endosomes after uptake at the sustained brain infections and acti-
tion that higher levels of periodontal neuromuscular junction [3] and the vation of the complement pathway
pathogen Treponema could be de- HSVs are transported inside the [32]. In transgenic mice over-ex-
tected in the brain and the trigemi- nerve in transport vesicles along pressing a mutated form of the
nal nerve of AD patients than in un- with APP [4, 35]. However, whether human APP, oral infection with Por-
affected controls [34]. The trigemi- Porphyromonas gingivalis and the gin- phyromonas gingivalis impaired the
nal nerve innervates the oral cavity gipains reach the CNS via axonal cognitive function and increased the
and connects it with the central transport and whether they are also buildup of AD-like deposits together
nervous system. Compared to peri- co-transported with APP is currently with alveolar bone loss compared
odontally healthy subjects, patients unclear. to non-infected mice [16]. Porphyro-
with PD have a higher risk for tri- monas gingivalis, the key stone bac-
geminal neuralgia, which is char- Detection of Porphyromonas terium of PD, was recently detected
acterized by recurrent paroxysmal gingivalis and gingipains in in the brains of AD patients for the
pain within the distribution of the the brain first time post mortem [6] and Por-
trigeminal nerve [22]. Experimental disruption of the tri- phyromonas gingivalis gingipains and
The most likely mechanism em- geminal nerve led to age-dependent LPS have also been detected in
ployed by Porphyromonas gingivalis loss of cholinergic neurons in learn- human AD brains [6, 33]. One of the
and the gingipains for passage ing and memory-related brain re- first brain regions to be damaged in
through the nerve is axonal trans- gions and impaired learning in a AD is the hippocampus. The study
port using the axonal transport ma- mouse model of AD (SAMP8 mice) by Dominy et al. could demonstrate
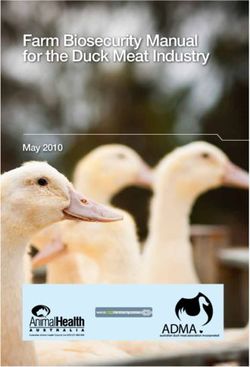
(Fig. 3: Teixeira, 2017, [43])
Figure 3 Periodontitis, Porphyromonas gingivalis, gingipains, and Alzheimer’s disease. Periodontitis is a bacteria-induced chronic
inflammation of the tooth supporting structures. Porphyromonas gingivalis is a key pathogen involved in the pathogenesis of peri-
odontitis. The periodontal inflammation triggers bacteremia of P. gingivalis, a systemic inflammation, and a pro-inflammatory acute
phase reaction, which lead to blood-brain barrier (BBB) damage. P. gingivalis has the ability to infect the brain via the damaged BBB
or other means, such as the trigeminal nerve. The brain infection, which is also linked to gingipain-mediated neurodegeneration,
triggers a Th1/Th2 inflammatory response and activation of the brain’s innate immune system (interferon-γ (IFN-γ) leading to
accumulation of fibrillar amyloid β (Aβ), and tau. Figure adopted from figure 1 in reference [43].
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)AARABI, THOMALLA, WALTHER ET AL.:
126 Periodontitis as potential risk factor for Alzheimer’s disease
gingipain RgpB in neurons of the other hand, gingipains were found Acknowledgments
dentate gyrus and CA3, CA2, and also in healthy people and some Ghazal Aarabi, Götz Thomalla,
CA1 of the hippocampus [6]. In ad- people with AD did not have in- Guido Heydecke and Thomas Beikler
dition, RgpB co-localized primarily creased levels compared to these are employed at and receive salaries
with neurons and astrocytes as well controls. People with AD reduce from the University Medical Center
as with tau tangles, and intra-neu- their oral hygiene and they tend to Hamburg-Eppendorf, Carolin Walter
ronal Aβ, but not with microglia, get leaky blood-brain barriers, which and Carola Mayer and Udo Seedorf
which was consistent with the pro- may increase their susceptibility to are employed at the University
posed roles of Porphyromonas gingi- infections in their brains. Thus, it Medical Center Hamburg-Eppendorf
valis in the pathogenesis of AD. cannot be excluded that the brain and their salary is funded by third
infection is merely a by-product in- party funds.
Implications for treatment stead of a cause of the disease. The
of Alzheimer’s disease data from the mouse models may not
To date, several classes of gingipain be of much relevance for the situ-
inhibitors have been described. ation in humans because Porphyro- Conflicts of interest
These include inhibitors from natu- monas gingivalis is a pathogen that GA, CW, CM, TB, GH, and US de-
ral sources, synthetic compounds, infects humans and has evolved clare no potential conflicts of inter-
antibiotics, antiseptics, antibodies, alongside the human immune sys- est, GT declares that he has received
and bacteria. Most known synthetic tem. Nevertheless, animal models consulting fees from Acandis and
compounds are potent gingipain in- are essential to generate new hypo- Stryker, grants from Bayer, and lec-
hibitors but have undesirable side theses, which can be tested, prefer- ture fees from Bayer, Boehringer
effects because they also inhibit a entially in randomized clinical trials, Ingelheim, Bristol-Meyers Squibb/
wide range of host proteases. Natu- to see whether a new intervention Pfizer, Daiichi Sankyo, Portola, and
ral inhibitors include cranberry benefits people suffering from AD. Stryker.
and rice extracts, which inhibit gin- Since it is highly unlikely that a
gipain activity and prevent the single type of bacteria is the only
growth and biofilm formation of cause of a disease as complex as AD,
References
periodontal pathogens. Meanwhile a we need a better understanding of
small molecule gingipain inhibitor, the potential role of the whole oral 1. Aarabi G, Thomalla G, Heydecke G,
COR388, has been developed, which microbiota as a cause of the disease, Seedorf U: Chronic oral infection: an
emerging risk factor of cerebral small
was safe and well-tolerated in i.e. microbiome studies of human
vessel disease? Oral Dis 2019; 25:
2 Phase 1 trials. COR388 is currently brains post mortem. Also important 710–719
tested in a larger phase 2/3 clinical are state-of-the-art brain magnetic
2. Abbayya K, Puthanakar NY, Nadu-
trial (the GingipAIN Inhibitor resonance imaging studies to dem-
winmani S, Chidambar YS: Association
for Treatment of Alzheimer’s Dis- onstrate a potential impact of the between periodontitis and Alzheimer‘s
ease trial, GAIN, ClinicalTrials.gov oral microbiota on preclinical sur- disease. N Am J Med Sci 2015; 7:
ID: NCT03823404) to evaluate rogate markers of AD, such as global 241–246
whether this oral drug is safe and brain volume, atrophy of subcortical
3. Bercsenyi K, Schmieg N, Bryson JB et
can slow or halt the progression of structures, like the hippocampus, al.: Tetanus toxin entry. Nidogens are
AD by blocking the neurotoxic ac- cerebral white matter disintegration, therapeutic targets for the prevention of
tivity of gingipains. The GAIN trial and graph-theoretical measures of tetanus. Science 2014; 346: 1118–1123
follows a randomized controlled de- topology of large-scale structural 4. Cheng SB, Ferland P, Webster P,
sign and is looking to enroll more brain networks. Bearer EL: Herpes simplex virus dances
than 500 participants with mild to Since PD is preventable and with amyloid precursor protein while
moderate AD at more than 90 clini- treatable, subjects with PD should exiting the cell. PLoS One 2011; 6:
cal trial centers in the United States be informed and treated in order to e17966. doi.org/10.1371/journal.
pone.0017966
and Europe. lower the microbial challenge and
to prevent the systemic inflamma- 5. Coureuil M, Lécuyer H, Bourdoulous
Final considerations tory burden, thereby promoting a S, Nassif X: A journey into the brain: In-
sight into how bacterial pathogens cross
The results reviewed here clearly higher quality of life. The recent
blood-brain barriers. Nat Rev Microbiol
support the notion that inflam- development of an oral gingipain 2017; 15: 149–159
mation plays an important role in inhibitor, which is currently tested
PD and AD. Figure 3 shows some of in a randomized controlled trial, for 6. Dominy SS, Lynch C, Ermini F et al.:
Porphyromonas gingivalis in Alzheimer‘s
the basic mechanisms and the se- the first time offers the opportunity
disease brains: Evidence for disease cau-
quence of events that may be in- to verify the infectious hypothesis sation and treatment with small-molecule
volved in the neurodegeneration in- of AD. If successful, this research inhibitors. Sci Adv 2019; 5(1): eaau3333.
duced by PD. The hypothesis that can be expected to result in a sig- doi:10.1126/sciadv.aau3333
PD and Porphyromonas gingivalis are nificant improvement of prevention 7. Ferri CP, Prince M, Brayne C, Global
causally related to AD and its pro- and treatment of PD and PD-related prevalence of dementia: a Delphi consen-
gression is highly attractive. On the AD. sus study. Lancet 2005; 366: 2112–2117
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)AARABI, THOMALLA, WALTHER ET AL.:
Periodontitis as potential risk factor for Alzheimer’s disease 127
8. Garde E, Mortensen EL, Krabbe K, 21. Kaye EK, Valencia A, Baba N, Spiro A, heimer‘s disease brain tissue. J Alzheimers
Rostrup E, Larsson HB: Relation between Dietrich T, Garcia RI: Tooth loss and peri- Dis 2013; 36: 665–677
age-related decline in intelligence and odontal disease predict poor cognitive
34. Riviere GR, Riviere KH, Smith KS:
cerebral white-matter hyperintensities in function in older men. J Am Geriatr Soc
Molecular and immunological evidence
healthy octogenarians: A longitudinal 2010; 58: 713–718
of oral Treponema in the human brain
study. Lancet 2000; 356: 628–634
22. Keller JJ, Sheu JJ, Lin HC: Chronic and their association with Alzheimer‘s
9. Gatz M, Mortimer JA, Fratiglioni L et periodontitis and the subsequent risk of disease. Oral Microbiol Immunol 2002;
al.: Potentially modifiable risk factors for trigeminal neuralgia: A 5-year follow-up 17: 113–118
dementia in identical twins. Alzheimers study. J Clin Periodontol 2012; 39:
35. Satpute-Krishnan P, DeGiorgis JA,
Dement 2006; 2: 110–117 1017–1023
Bearer EL:Fast anterograde transport of
10. GDB 2016 Dementia Collaborators: 23. Kinane DF, Berglundh T: Pathogen- herpes simplex virus: Role for the amy-
Global, regional, and national burden of esis of periodontitis. In: Lindhe J, Lang loid precursor protein of alzheimer‘s dis-
Alzheimer‘s disease and other dementias, NP, Karring T (Eds.): Clinical Periodontol- ease. Aging Cell 2003; 2: 305–318
1990–2016: A systematic analysis for the ogy and Implant Dentistry, 5th ed., 36. Sheets SM, Potempa J, Travis J, Casi-
global burden of disease study 2016. Vol. 1, Blackwell Munksgaard, Oxford ano CA, Fletcher HM: Gingipains from
Lancet Neurol 2019; 18: 88–106 2008, pp. 405419 Porphyromonas gingivalis W83 induce
11. Giacona MB, Papapanou PN, Lamster 24. Kinney JW, Bemiller SM, Murtishaw cell adhesion molecule cleavage and
IB et al.: Porphyromonas gingivalis in- AS, Leisgang AM, Salazar AM, Lamb BT: apoptosis in endothelial cells. Infect
duces its uptake by human macrophages Inflammation as a central mechanism in Immun 2005; 73: 1543–1552
and promotes foam cell formation in Alzheimer‘s disease. Alzheimers Dement 37. Sochocka M, Zwolińska K, Leszek J:
vitro. FEMS Microbiol Lett 2004; 241: (N Y) 2018; 4: 575–590 The infectious etiology of Alzheimer‘s
95–101 disease. Curr Neuropharmacol 2017; 15:
25. Kumar DK, Choi SH, Washicosky KJ et
12. Gorelick PB: Risk factors for vascular al.: Amyloid-β peptide protects against 996–1009
dementia and Alzheimer disease. Stroke microbial infection in mouse and worm 38. Socransky SS, Smith C, Haffajee AD:
2004; 35 (Suppl 1): 2620–2622 models of Alzheimer‘s disease. Sci Transl Subgingival microbial profiles in refrac-
Med 2016; 8: 340ra372. doi: 10.1126/ tory periodontal disease. J Clin Peri-
13. He Y, Zhu J, Huang F, Qin L, Fan W,
scitranslmed.aaf1059 odontol 2002; 29: 260–268
He H: Age-dependent loss of cholinergic
neurons in learning and memory-related 26. Lee JW, Lee YK, Yuk DY et al.: Neuro- 39. Soscia SJ, Kirby JE, Washicosky KJ et
brain regions and impaired learning in inflammation induced by lipopolysac- al.: The Alzheimer‘s disease-associated
SAMP8 mice with trigeminal nerve charide causes cognitive impairment amyloid beta-protein is an antimicrobial
damage. Neural Regen Res 2014; 9: through enhancement of beta-amyloid peptide. PLoS One 2010; 5: e9505. doi.
1985–1994 generation. J Neuroinflammation 2008; org/10.1371/journal.pone.0009505
5: 37. doi:10.1186/1742–2094–5–37
14. Hofman A, Ott A, Breteler MM et al.: 40. Spitzer P, Condic M, Herrmann M et
Atherosclerosis, apolipoprotein E, and 27. Lee YT, Lee HC, Hu CJ et al.: Peri- al.: Amyloidogenic amyloid-β-peptide
prevalence of dementia and Alzheimer‘s odontitis as a modifiable risk factor for variants induce microbial agglutination
disease in the Rotterdam Study. Lancet dementia: a nationwide population- and exert antimicrobial activity. Sci Rep
1997; 349: 151–154 based cohort study. J Am Geriatr Soc 2016; 6: 32228. doi:10.1038/srep32228
2017; 65: 301–305
15. Ide M, Harris M, Stevens A et al.: 41. Stein PS, Desrosiers M, Donegan SJ,
Periodontitis and cognitive decline in 28. Mawanda F, Wallace R: Can infec- Yepes JF, Kryscio RJ: Tooth loss, dementia
Alzheimer‘s disease. PLoS One 2016; 11: tions cause Alzheimer‘s disease? Epi- and neuropathology in the Nun study.
e0151081. doi.org/10.1371/journal. demiol Rev 2013; 35: 161–180 J Am Dent Assoc 2007; 138: 1314–1322;
pone.0151081 quiz 1381–1312
29. Mitrabhakdi E, Shuangshoti S, Wan-
16. Ishida N, Ishihara Y, Ishida K et al.: nakrairot P et al.: Difference in neuro- 42. Takeuchi H, Sasaki N, Yamaga S,
Periodontitis induced by bacterial infec- pathogenetic mechanisms in human Kuboniwa M, Matsusaki M, Amano A:
tion exacerbates features of Alzheimer‘s furious and paralytic rabies. J Neurol Sci Porphyromonas gingivalis induces
disease in transgenic mice. NPJ Aging 2005; 238: 3–10 penetration of lipopolysaccharide and
Mech Dis 2017; 3: 15-x. peptidoglycan through the gingival
30. Noble JM, Borrell LN, Papapanou PN, epithelium via degradation of junctional
doi:10.1038/s41514–017–0015-x
Elkind MS, Scarmeas N, Wright CB: Peri- adhesion molecule 1. PLoS Pathog 2019;
17. Ishii K: PET approaches for diagnosis odontitis is associated with cognitive 15: e1008124. doi:10.1371/journal.
of dementia. AJNR Am J Neuroradiol impairment among older adults: anal- ppat.1008124
2014; 35: 2030–2038 ysis of NHANES-III. J Neurol Neurosurg
Psychiatry 2009; 80: 1206–1211 43. Teixeira FB, Saito MT, Matheus FC et
18. Jaeger LB, Dohgu S, Sultana R et al.: al.: Periodontitis and Alzheimer‘s disease:
Lipopolysaccharide alters the blood-brain 31. Panza F, Lozupone M, Solfrizzi V, a possible comorbidity between oral
barrier transport of amyloid beta protein: Watling M, Imbimbo BP: Time to test chronic inflammatory condition and
a mechanism for inflammation in the antibacterial therapy in Alzheimer‘s dis- neuroinflammation. Front Aging Neuro-
progression of Alzheimer‘s disease. Brain ease. Brain 2019; 142: 2905–2929 sci 2017; 9: 327
Behav Immun 2009; 23: 507–517
32. Poole S, Singhrao SK, Chukkapalli S 44. Tonsekar PP, Jiang SS, Yue G: Peri-
19. Kagan BL, Jang H, Capone R et al.: et al.: Active invasion of Porphyromonas odontal disease, tooth loss and demen-
Antimicrobial properties of amyloid pep- gingivalis and infection-induced comple- tia: is there a link? A systematic review.
tides. Mol Pharm 2012; 9: 708–717 ment activation in ApoE-/- mice brains. Gerodontology 2017; 34: 151–163
J Alzheimers Dis 2015; 43: 67–80
20. Kamer AR, Pirraglia E, Tsui W et al.: 45. Van Cauwenberghe C, Van Broeck-
Periodontal disease associates with 33. Poole S, Singhrao SK, Kesavalu L, hoven C, Sleegers K: The genetic land-
higher brain amyloid load in normal Curtis MA, Crean S: Determining the scape of Alzheimer disease: clinical impli-
elderly. Neurobiol Aging 2015; 36: presence of periodontopathic virulence cations and perspectives. Genet Med
627–633 factors in short-term postmortem Alz- 2016; 18: 421–430
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)AARABI, THOMALLA, WALTHER ET AL.:
128 Periodontitis as potential risk factor for Alzheimer’s disease
46. Walter C, Zahlten J, Schmeck B et al.:
(Photo: Löffler Foto, Schiffstr. 5–7,
Porphyromonas gingivalis strain-depen-
(Photo: private, Udo Seedorf)
dent activation of human endothelial
cells. Infect Immun 2004; 72: 5910–5918
47. Wiesner J, Vilcinskas A: Antimicrobial
79098 Freiburg)
peptides: The ancient arm of the human
immune system. Virulence 2010; 1:
440–464
48. Wu YT, Beiser AS, Breteler MMB et al.:
The changing prevalence and incidence
of dementia over time – current evidence. PD DR. MED. DENT. PROF. DR.
Nat Rev Neurol 2017; 13: 327–339
GHAZAL AARABI, MSC. UDO SEEDORF
49. Wyss-Coray T, Rogers J: Inflamma- Department of Prosthetic Dentistry, Department of Prosthetic Dentistry,
tion in Alzheimer disease-a brief review Center for Dental and Oral Medicine, Center for Dental and Oral Medicine,
of the basic science and clinical literature. University Medical Center University Medical Center
Cold Spring Harb Perspect Med 2012; Hamburg-Eppendorf Hamburg-Eppendorf
2: a006346. doi:10.1101/ Martinistr. 52, 20251 Hamburg Martinistr. 52, 20251 Hamburg
cshperspect.a006346 g.aarabi@uke.de u.seedorf@uke.de
© Deutscher Ärzteverlag | DZZ International | Deutsche Zahnärztliche Zeitschrift International | 2021; 3 (3)You can also read