Long-Term Intake of North American Ginseng Has No Effect on 24-Hour Blood Pressure and Renal Function
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Long-Term Intake of North American Ginseng Has No
Effect on 24-Hour Blood Pressure and Renal Function
P. Mark Stavro, Minna Woo, Lawrence A. Leiter, Tibor F. Heim,
John L. Sievenpiper, Vladimir Vuksan
Abstract—Ginseng is consumed by 10% to 20% of adults in Asia and by up to 5% in Western countries. Despite
observational evidence suggesting a link between its intake and the development of hypertension, there remains no
long-term scrutiny for its effect on blood pressure (BP). We therefore undertook a randomized, placebo-controlled,
double-blinded, crossover trial in 52 hypertensive individuals to determine the effect of 12-week North American
ginseng intake on 24-hour BP; we also measured serum cystatin C as a marker of renal function. After a 4-week placebo
run-in, we randomly assigned 52 participants to 3 g/day of ginseng or placebo for 12 weeks. This was followed by an
8-week washout and a subsequent 12-week period in which the opposite treatment was administered. At run-in and at
weeks 0 and 12 of each treatment period, participants were fitted with an ambulatory BP monitor to assess 24-hour BP.
The primary outcome was the treatment difference at week 12 in mean 24-hour systolic BP. Secondary outcomes were
treatment differences at week 12 in other ambulatory BP parameters and serum cystatin C. Forty participants (77%)
completed the trial, with 3 removed from main analysis (n⫽2, antihypertensive drug changes; n⫽1, incomplete
ambulatory monitoring). In the remaining 37, 12-week ginseng treatment was associated with a neutral effect on all
ambulatory BP parameters compared with placebo; an intention-to-treat analysis supported this. Ginseng did not affect
serum cystatin C level. Overall, long-term ginseng use had no effect on 24-hour BP and renal function in hypertensive
individuals. (Hypertension. 2006;47:791-796.)
Key Words: clinical trials 䡲 blood pressure 䡲 hypertension, essential
G inseng is an herb that populations have valued as a tonic
since 25 A.D.1 It is also shown through randomized,
controlled trials (RCTs) to improve glycemic control2 and
seng together account for the majority of ginseng consumed
worldwide. Recently, we demonstrated that single 3-g doses
of NAG15 and P ginseng16 exert neutral and lowering effects
cognitive function.3 In contrast, however, there is repeated on BP, respectively, for 160 minutes after intake. In the
mention in the medical literature that ginseng can elevate former study,15 the neutral effect on BP was comprehensively
blood pressure (BP).4 – 6 This stems from an early observa- shown with 6 batches of NAG in hypertensive individuals. To
tional study by Siegel7 that connected the self-reported use of add to this finding now, the long-term effect of NAG on BP
ginseng to the development of hypertension in 14 individuals would be of even greater significance, because long-term BP
after 3 months of use. This possibility could have widespread outcomes are associated with cardiovascular disease events.17,18
impact, because ginseng is used by 10% to 20% of adults in Also, because long-term BP outcomes might not necessarily
Asia8 –10 and by up to 5% in the United States,11 Australia,12 be inferable from acute outcomes,19 we proceeded to address
and parts of Europe.13 Furthermore, given that 20% to 40% of the effect of NAG on BP after 12 weeks of intake (defined as
adults in these regions are estimated to have hypertension,14 long-term relative to our acute studies). We measured 24-
there is potential for overlap between the prevalence of hour ambulatory BP (ABP), because it is a better determinant
ginseng use and hypertension. Still, there remains no long- of cardiovascular disease risk than office BP, and it allows for
term RCT investigation of the effect of ginseng on BP, and an assessment of circadian BP changes.20,21 As well, for
until such evaluations are undertaken, physicians will remain safety reasons, serum cystatin C was measured as a marker of
greatly limited in the advice they can provide to hypertensive glomerular filtration rate and an indicator of the effect of
individuals regarding ginseng use. NAG on renal function.22
Although many species of ginseng exist, Panax quinque- We determined here, through a single-center, randomized,
folius, or North American ginseng (NAG), and Panax gin- controlled, double-blinded, crossover trial, the effect of 12-
Received November 1, 2005; first decision November 5, 2005; revision accepted January 13, 2006.
From the Risk Factor Modification Centre (P.M.S., L.A.L., J.L.S., V.V.) and Division of Endocrinology and Metabolism (M.W., L.A.L.), St Michael’s
Hospital, Toronto, Ontario, Canada; and Departments of Medicine (M.W., L.A.L, V.V.) and Nutritional Sciences (P.M.S., L.A.L., T.F.H., V.V.), Faculty
of Medicine, University of Toronto, Toronto, Ontario, Canada.
Correspondence to Vladimir Vuksan, Risk Factor Modification Centre, St Michael’s Hospital, #6-136 61 Queen St East, Toronto, Ontario, Canada M5C
2T2. E-mail v.vuksan@utoronto.ca
© 2006 American Heart Association, Inc.
Hypertension is available at http://www.hypertensionaha.org DOI: 10.1161/01.HYP.0000205150.43169.2c
791
Downloaded from http://hyper.ahajournals.org/ by guest on March 6, 2015792 Hypertension April 2006
week NAG intake on 24-hour ABP and renal function in participants to consume a 3-g daily dose as 3 capsules between 7:00
hypertensive individuals. We used a single batch of NAG, AM and 9:00 AM and 3 between 7:00 PM and 9:00 PM, because
preliminary evidence has suggested that ginsenosides remain in
which was representative of NAG on the world market and
human plasma for ⬇12 hours.25 All of the study personnel (including
which was shown previously to exert a neutral effect on BP those administering the treatments and those assessing the outcomes)
for 160 minutes after intake.15 Thus, this study provided, for and participants were blinded to treatment assignment for the
the first time, insight into how long-term ginseng intake could duration of the study.
affect both BP and renal function in humans. After screening, 52 individuals were deemed eligible, and 28 were
randomly assigned to the NAG-then-placebo treatment sequence and
24 to the placebo-then-NAG treatment sequence. The protocol
Methods included: (1) a 4-week open-label placebo run-in, (2) a 12-week
Participants treatment period in which the first treatment of the assigned sequence
was consumed, (3) an 8-week washout period with no treatment, and
The research ethics board at St Michael’s Hospital approved the
(4) a 12-week treatment period in which the second treatment of the
study, and the procedures used were in accordance with institutional
assigned sequence was consumed. At the start of run-in, and at the
guidelines. Individuals were recruited through newspaper advertise-
start (week 0) and end (week 12) of each treatment period, partici-
ments in Toronto and provided written informed consent to partici-
pants arrived at our clinic between 8:00 AM and 9:00 AM fasted (10
pate. Inclusion was an age of 18 to 85 years and hypertension as
to 12 hours prior) and off their antihypertensives (8 hours prior).
defined by the use of antihypertensive drugs or a seated office
Initially, they had body weight assessed, blood samples drawn, and
systolic BP ⱖ140 mm Hg or diastolic BP ⱖ90 mm Hg at each of 3
were fitted with an ABP monitor (ABPM) that was activated
prestudy visits. Exclusion was secondary hypertension, white-coat
between 9:00 AM and 10:00 AM. Immediately after ABPM activation,
hypertension, diabetes, kidney/liver disease, unstable angina, gin-
each participant began his/her typical antihypertensive drug routine
seng use for 2 months before or during the study, or any changes in
(we were, thus, able to ensure that antihypertensive drugs were taken
the type/dose of antihypertensive drugs 1 month before or during
according to the same schedule each time the ABPM was worn).
the study.
Participants refrained from taking NAG or placebo capsules for the
Overall, 37 (30 men and 7 women) hypertensive individuals were
period that the ABPM was worn (ⱖ24 hours). Participants were
included in the main analysis. Their ethnicities included European-white instructed to retire between 10:00 PM and 12:00 AM and to awaken
(n⫽26), East-Asian (n⫽5), South-Asian (n⫽4), African-Caribbean between 6:00 AM and 8:00 AM. They also prepared a 24-hour diary
(n⫽2), and Native-Canadian (n⫽1) individuals. At run-in they had a detailing activity, sleep, and drug schedules.
mean⫾SEM age of 58.4⫾1.6 years, body mass index of 28.6⫾0.9
kg/m2, serum cystatin C of 0.97⫾0.03 mg/L, office systolic/diastolic
BP of 130.2⫾2.4/85.8⫾1.6 mm Hg, and 24-hour systolic/diastolic Primary and Secondary Outcomes
BP of 131.6⫾1.9/81.1⫾1.5 mm Hg. Of the 37 individuals, 32 were The primary outcome was mean 24-hour ambulatory systolic BP at
taking antihypertensive agents (monotherapy, n⫽20; ⱖ2 agents, n⫽12), week 12. Secondary outcomes included mean 24-hour diastolic BP
including angiotensin-converting enzyme inhibitors (n⫽16), angioten- and pulse pressure (PP), as well as mean daytime and night systolic
sin receptor blockers (n⫽5), -blockers (n⫽7), calcium channel block- BP, diastolic BP, and PP at week 12, with daytime defined as 8:00
AM to 8:00 AM and nighttime as 12:00 AM to 6:00 AM.21,26,27
ers (n⫽12), diuretics (n⫽8), and ␣-blockers (n⫽1). The run-in charac-
teristics of the 37 individuals included in the main analysis did not Additional secondary outcomes were serum cystatin C (marker of
significantly differ from those who withdrew or were removed from kidney function)22 and body weight at week 12. To avoid multiplic-
main analysis (n⫽15; data not shown). ity, no subgroup analyses or adjusted analyses were performed.
Treatments and Protocol BP Measurement
In this single-center, randomized, placebo-controlled, double- Office BP (at recruitment and run-in) was measured as described
blinded trial conducted between April 2001 and October 2003 previously.15 Briefly, 3 readings were obtained from the right arm of
(recruitment: April 2001 to May 2002; follow-up: May 2002 to seated participants while their arm was supported at heart level; 1
October 2003), we sought to determine the effect of 12-week NAG trained observer took all of the measures and used a mercury
intake on 24-hour BP. To do so, we used an AB/BA 2-treatment, sphygmomanometer (Baumanometer, W.A. Baum). For ABP mea-
2-period crossover design with the treatment sequences being NAG- surements, participants were fitted with a SpaceLabs 90207 ABPM
then-placebo and placebo-then-NAG.23 (SpaceLabs), with the cuff secured on the nondominant arm for the
We tested a 3-g dose of cornstarch placebo and a single batch of entire ⱖ24-hour period (worn on the same arm for all of the visits).
3-year-old dried NAG root from an Ontario farm. Its acute BP effects ABPM measurements occurred every 15 minutes from 7:00 AM to
and ginsenoside profile have been described previously (where it was 9:00 PM inclusive and every 20 minutes from 10:00 PM to 6:00 AM
designated as NAG from Farm B).15 Briefly, the total ginsenoside inclusive, with a maximum of 87 successful readings for the 24-hour
content of NAG was 62.8 mg/g; as well, its authenticity was period. Measurements were automatically repeated if an error oc-
indicated by the lack of ginsenoside Rf, which is absent from NAG curred. The adult and large adults cuffs were used for arm circum-
but found in other ginseng species, such as P ginseng.24 We ferences of 24 to 31 cm and 32 to 42 cm, respectively.
administered NAG and cornstarch as powders in identical blue-white
500 mg #00 capsules (with vanilla extract added to mask smell and Cystatin C
taste), which were prepared by Sunny Crunch Foods Ltd (Markham, All of the assays were performed in serum obtained from fasted
Ontario, Canada). participants. Specimens were stored at ⫺70°C. Cystatin C was
Capsules were packaged in identical bottles, with their contents measured by a particle-enhanced immunonephelometric assay (N
known by 1 person independent of the conduct of the study. This Latex Cystatin C, Dade Behring) with a nephelometer (BNII, Dade
person coded the treatment bottles, performed the blinding, and Behring).
prepared a concealed allocation schedule that randomly assigned 2
treatment sequences (NAG-then-placebo and placebo-then-NAG) to Statistical Analyses
a consecutive series of numbers in an order generated by a random- Based on previous findings,16 we speculated that the maximum
number table. The treatments were sealed in sequentially numbered difference in mean 24-hour systolic BP at week 12 between NAG
bottles according to the allocation schedule. On enrollment, each and placebo would be 4.4 mm Hg. Accordingly, with an estimated
participant was assigned to the next consecutive number, and at the SD of the between-treatment difference being 7.1 mm Hg and
start of each study period, a second person dispensed the partici- assuming a correlation coefficient of 0.80 between-treatment values
pant’s corresponding bottles of treatment capsules. We instructed at week 12, at a significance level (␣) of 0.05 we calculated that 36
Downloaded from http://hyper.ahajournals.org/ by guest on March 6, 2015Stavro et al Ginseng and 24-Hour Blood Pressure 793
individuals were required to achieve the noted difference in mean All of the analyses were run with sex and age as covariates and
24-hour systolic BP compared with placebo with 80% power. Based were performed with the Number Cruncher Statistical Software
on previous withdrawal rates of ⬇10% during study periods of 12 2000. Significance was set at ␣ of 0.05 and was 2-sided. Values are
weeks,28 we calculated that the enrollment of 52 participants would expressed as mean⫾SEM.
yield 36 participants to a 36-week study period.
We conducted a main analysis, a secondary analysis, and an Adequacy of Blinding
intention-to-treat analysis. The main analysis included participants The adequacy of blinding was assessed according to participant
who: (1) finished both treatment periods, (2) completed 24-hours of responses when asked which treatment they believed they were
ABP monitoring for all of the visits, and (3) adhered to the study taking (NAG, placebo, or uncertain). This question was asked after
protocol and exclusion criteria (ie, no medication changes). Data each treatment period by an individual independent of the conduct of
from these participants underwent crossover analysis.23 According to the study.
the assumptions of this analysis, each parameter was first tested for
a period and carryover effect. Then, for the 24-hour, 8:00 AM to 8:00 Results
PM, and 12:00 AM to 6:00 AM periods, the independent and interactive
effects of treatment (NAG and placebo), week (0 and 12), and time
Subjects
of day (hour) on ambulatory systolic BP, diastolic BP, and PP were Of the screened individuals (n⫽67), 52 proceeded through
assessed by a repeated measures, general linear model (GLM), and run-in and randomization. Among them, 12 (23%) withdrew:
3-way ANOVA. Significant treatment effects were additionally 8 from the NAG-then-placebo sequence (n⫽3, period 1; n⫽1,
explored at weeks 0 and 12 with repeated-measures GLM-ANOVA. washout; n⫽4, period 2) and 4 from the placebo-then-NAG
For cystatin C, the independent and interactive effects of treatment and sequence (n⫽2, period 1; n⫽2, washout). Accordingly, 3
week were assessed by repeated-measures GLM 2-way ANOVA. withdrew while taking NAG (n⫽1, diarrhea; n⫽1, headache;
Significant treatment effects were additionally explored at weeks 0 and
12 with repeated-measures GLM-ANOVA. We assessed body weight n⫽1, antihypertensive drug change), 6 while taking placebo
by the same procedure. (n⫽6, work schedule), and 4 during washout (n⫽3, work
The secondary analysis included participants who finished the first schedule; n⫽1, antihypertensive drug change). Also, 3 from
treatment period with complete 24-hour ABPM at weeks 0 and 12. the placebo-then-NAG sequence were not included in main
This analysis followed a parallel design test in which a GLM 2-way analysis because of antihypertensive drug changes (n⫽2) and
ANOVA tested the independent and interactive effects of treatment unsuccessful ABPM (n⫽1). Overall, 37 participants (71%)
(NAG versus placebo) and week (0 versus 12) on ABP during the
proceeded to main analysis.
first treatment period. Significant treatment effects were explored at
these weeks with a GLM-ANOVA. The intention-to-treat analysis
included all of the participants who finished both treatment periods Compliance and Blinding
with complete 24-hour ABPM, and their data underwent crossover Compliance was estimated by pill count (NAG: 91.7⫾2.3%;
analysis (as described for main analysis).23 placebo: 93.6⫾1.9%; P⫽0.50). Evaluation of blinding re-
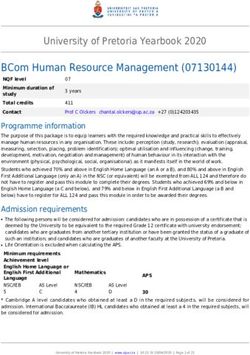
Mean 24-Hour, Daytime, and Night Ambulatory Systolic BP, Diastolic BP, and PP Before (Week 0) and After
(Week 12) NAG and Placebo Intake in 37 Hypertensive Participants
Week 0 Week 12 Difference at Week 12
(n⫽37), P (n⫽37), P (NAG–Placebo 95% CI),
Parameter Treatment mm Hg Value* mm Hg Value* mm Hg
24-Hour systolic BP NAG 129.6⫾1.8 0.56 130.9⫾2.0 0.99 (⫺2.4 to 2.4)
Placebo 130.4⫾1.9 130.9⫾1.8
Daytime systolic BP† NAG 135.1⫾2.0 0.83 136.6⫾2.1 0.64 (⫺2.0 to 3.3)
Placebo 135.9⫾2.0 136.0⫾2.0
Night systolic BP‡ NAG 118.3⫾1.7 0.25 120.8⫾1.9 0.59 (⫺3.9 to 2.2)
Placebo 120.1⫾2.1 121.6⫾1.8
24-Hour diastolic BP NAG 79.7⫾1.3 0.91 80.6⫾1.5 0.99 (⫺1.6 to 1.7)
Placebo 79.9⫾1.3 80.5⫾1.4
Daytime diastolic BP† NAG 84.6⫾1.5 0.93 84.9⫾1.5 0.79 (⫺1.6 to 2.0)
Placebo 84.6⫾1.5 84.7⫾1.5
Night diastolic BP‡ NAG 71.4⫾1.3 0.63 73.4⫾1.6 0.94 (⫺2.3 to 2.2)
Placebo 72.4⫾1.4 73.4⫾1.3
24-Hour PP NAG 49.8⫾1.6 0.27 50.3⫾1.6 0.94 (⫺1.5 to 1.4)
Placebo 50.4⫾1.5 50.4⫾1.5
Daytime PP† NAG 51.1⫾1.7 0.61 51.6⫾1.8 0.60 (⫺1.2 to 1.9)
Placebo 51.5⫾1.6 51.3⫾1.6
Night PP‡ NAG 46.9⫾1.6 0.21 47.4⫾1.5 0.35 (⫺2.5 to 0.9)
Placebo 48.1⫾1.6 48.2⫾1.5
Also shown are the 95% CIs for the treatment differences at week 12. Values are presented as mean⫾SEM.
*P values are for between-treatment comparisons at week 0 and at week 12.
†Daytime indicates the mean of the period 8:00 AM to 8:00 PM inclusive.
‡Night indicates the mean of the period 12:00 AM to 6:00 AM inclusive.
Downloaded from http://hyper.ahajournals.org/ by guest on March 6, 2015794 Hypertension April 2006
vealed that of the 40 participants who completed both (13:00 hours), however, diastolic BP was significantly higher
treatment periods, only 16 expressed certainty of when (ie, at week 12 for NAG compared with placebo (Figure). There
indicated what period) they consumed NAG. Accordingly, 9 were no other mean hourly differences.
of 40 (22.5%) correctly predicted when they were on NAG, Body weight did not differ between NAG and placebo at
whereas 7 of 40 (17.5%) indicated they were on NAG when week 0 (82.8⫾2.3 versus 82.7⫾2.3 kg, respectively; P⫽0.86;
on placebo (P⫽0.58 for 2 analysis). n⫽37) and at week 12 (82.6⫾2.3 versus 82.8⫾2.3 kg, respec-
tively; P⫽0.47; n⫽37). The serum level of cystatin C did not
Main Analysis of BP, Cystatin C, and differ between NAG and placebo at week 0 (0.97⫾0.03
Body Weight versus 0.98⫾0.03 mg/L, respectively; P⫽0.40; n⫽34) and at
There were no significant period or carryover effects on any week 12 (1.00⫾0.03 versus 0.90⫾0.03 mg/L, respectively;
of the measured parameters (BP, bodyweight, or cystatin C). P⫽0.32; n⫽34). A sufficient number of blood samples were
For the BP parameters at week 0, mean values did not differ obtained from only 34 participants for the measurement of
between NAG and placebo (Table). However, at 6:00 AM on serum cystatin C.
week 0, the PP was significantly lower for NAG compared
with placebo (P⬍0.05; Figure); there were no other mean Secondary Analysis
hourly differences. The secondary analysis included the 39 participants who
There was no significant effect of treatment on the primary completed the entire study plus those who withdrew but
outcome, mean 24-hour systolic BP, or on any secondary completed the first treatment period (n⫽7). When their data
outcomes (ie, mean values at week 12 did not differ between were analyzed together in a parallel-design comparison of
NAG and placebo; Table); and there was no significant NAG (n⫽25) versus placebo (n⫽21) on all of the ABP
interaction among treatment, week, and/or hour. At 1:00 PM parameters from treatment period 1, NAG showed no signif-
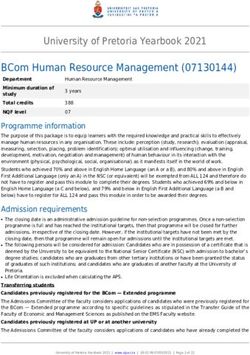
The mean⫾SEM hourly ambulatory sys-
tolic BP, diastolic BP, and PP values
before (at week 0) and after (at week 12)
treatment with 3 g/day of North Ameri-
can ginseng (f) and placebo (䡺) in 37
hypertensive individuals. *North Ameri-
can ginseng vs placebo, P⬍0.05.
Downloaded from http://hyper.ahajournals.org/ by guest on March 6, 2015Stavro et al Ginseng and 24-Hour Blood Pressure 795
icant effect versus placebo on any parameter (results not ginseng known as P quinquefolius, or NAG. NAG is unique
shown). from P ginseng, which is the species that has been tested in other
clinical interventions on ginseng and BP.16,33–35 After harvest,
Intention-to-Treat Analysis the root portion of NAG is dried, whereas the root portion of
Because 12 of the 52 randomized participants were lost to P ginseng is either dried or steamed,1 with the steamed form
follow-up, and 1 had incomplete ABPM, the intention-to-treat being marketed as Korean red ginseng (KRG). Importantly,
analysis included 39 individuals. It was only performed for ABP NAG contains a 3- to 5-times higher content of ginsenosides
and showed no significant effect of period, carryover, or treat- and different profile of ginsenosides than both forms of P
ment on any ABP parameter (results not shown). ginseng.2,15,16,24,28 As well, KRG is the only marketed ginseng
to contain ginsenoside Rg3, the most potent vasodilating
Discussion ginsenoside.36
We showed here, for the first time in a long-term RCT, the effect To date, 4 clinical interventions have tested the effect of P
of ginseng on BP and renal function. The ginseng used was ginseng root on BP.16,33–35 Of these, 1 tested the dried root
NAG, which is a species native to North America that is used and showed that an aqueous-ethanol extract of it at 200
predominantly in Canada, the United States, and China.29 We mg/day had no effect on BP in a 4-week RCT with young,
found that its intake at 3 g/day for 12 weeks relative to normotensive adults.33 In the case of steamed root, KRG, our
placebo was associated with a neutral effect on BP in group found that 3 g of the natural root could lower BP for
hypertensive individuals. This was shown in the main analysis 160 minutes relative to placebo in an RCT with hypertensive
by a lack of difference between NAG and placebo at 12 weeks individuals.16 As well, an 8-week nonrandomized trial dem-
for each of the mean 24-hour, daytime and night ABP parame- onstrated that 4.5 g/day of the natural KRG root significantly
ters (Table), which was supported by an intention-to-treat decreased BP in hypertensive individuals.35 Furthermore, in a
analysis. Also, although there was an increase in diastolic BP nonrandomized trial with young, normotensive adults, an
for NAG relative to placebo at the 1:00 PM (13:00 hours) time aqueous extract of KRG root at a mean dose of 610 mg
point of week 12 (Figure), this was considered clinically significantly decreased BP at 45, 60, and 75 minutes after
insignificant, because mean daytime and 24-hour diastolic BP intake.34 Thus, although studies on ginseng and BP exist, the
did not differ between treatments. As for cystatin C, NAG use of extracts and nonrandomized designs was common,
intake did not affect its serum level relative to placebo, which precluded an accurate assessment of efficacy. Still,
indicating no influence on renal function. Thus, this study evidence to date indicates that NAG has no effect on BP and
showed that 12-week consumption of NAG had no effect on that P ginseng, if steamed, could be antihypertensive. Future
ABP or renal status in hypertensive individuals. RCTs will have to determine whether the ginseng species, the
The BP outcomes here added to our previous finding,15 steaming process, and the ginsenoside content and/or profile are
which showed an acute neutral effect on BP with 6 batches of important factors affecting BP. Importantly, though, contrary to
NAG differing in quality and profile of ginsenosides, phar- Siegel’s7 observational finding, no clinical intervention has
macologically active components of NAG.30 Importantly, the shown ginseng to elevate BP.
6 batches were chosen by the Ginseng Growers Association In the current study, 2 participants reported adverse events
of Ontario to represent the total crop of NAG from Ontario, (headache and diarrhea), and withdrew, and both were taking
which supplies ⬎60% of NAG worldwide.15 Here, we tested NAG at the time. Whereas clinical documentation of the
1 of these batches, and because it was phytochemically adverse events of NAG is lacking, Coon and Ernst37 system-
similar to the other 5 batches, we speculated that our current atically reviewed 146 clinical trials representing ⬎8500
findings could be extrapolated to these other 5 and, thus, to a individual exposures to P ginseng and found it to have the
majority of NAG on the world market. same adverse event profile as placebo.
With respect to the form of NAG tested, we administered The current study had 3 limitations. First, 25% of the
the whole dried root in its natural form, which is the most participants withdrew, and another 5% had their data re-
consumed form, and the form that cultivators sell to supple- moved from main analysis. We did, however, conduct a
ment manufacturers. Accordingly, we were able to assess all secondary analysis and intention-to-treat analysis to rectify
of the components of NAG within their native matrix. In this, and both showed identical outcomes to the main analy-
particular, we avoided using aqueous-alcohol extracts, be- sis. Second, whereas the antihypertensive-treated participants
cause they would have contained only the NAG components in the main analysis (n⫽32) held their antihypertensive
soluble within the base of the extract,31 thus precluding a type(s) and dose(s) constant for the entire study, their use of
comprehensive investigation of the efficacy of NAG. antihypertensives could have prevented an accurate interpre-
As for dosage, in keeping with our acute efficacy trial,15 we tation of the effect of NAG on BP because of possible
administered 3 g, which is the recommended dose of ginseng NAG– drug interactions. However, an objective here was to
in traditional Chinese medicine,32 and the average intake determine the effect of NAG on BP in a representative
reported in the study by Siegel,7 where ginseng intake was population of hypertensive individuals so that the findings
associated with elevated BP. As well, the 12-week treatment could be extrapolated to such individuals. To add to the
period represented the time span in which hypertension current findings, future studies should determine the effect of
developed in Siegel’s report.7 NAG on BP in untreated hypertensive or prehypertensive
Although this was the first long-term RCT on ginseng root individuals to better understand the influence of NAG on BP
and BP, it should be emphasized that it evaluated the species of in the absence of antihypertensive drugs.
Downloaded from http://hyper.ahajournals.org/ by guest on March 6, 2015796 Hypertension April 2006
Perspectives 16. Stavro PM, Woo M, Vuksan V. Korean red ginseng lowers blood pressure
The topic of ginseng and BP in humans commenced ⬎25 years in individuals with hypertension (abstract). Am J Hypertens. 2004;17:S33.
17. Neal B, MacMahon S, Chapman N. Effects of ace inhibitors, calcium
ago with an observational study that suggested a link between antagonists, and other blood-pressure-lowering drugs: Results of prospec-
ginseng use and hypertension.7 Since then, 2 acute-duration tively designed overviews of randomised trials. Blood pressure lowering
RCTs found that NAG15 and P ginseng16 have neutral and treatment trialists’ collaboration. Lancet. 2000;356:1955–1964.
lowering effects on BP, respectively. We showed here that 18. Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, Hua
T, Laragh J, McInnes GT, Mitchell L, Plat F, Schork A, Smith B,
12-week intake of NAG is associated with a neutral effect on Zanchetti A. Outcomes in hypertensive patients at high cardiovascular
24-hour BP relative to placebo in a multiethnic, middle-to- risk treated with regimens based on valsartan or amlodipine: The value
older aged, hypertensive population. NAG also had no effect randomised trial. Lancet. 2004;363:2022–2031.
on the serum level of cystatin C, a marker of renal function 19. Guyton AC. Blood pressure control–special role of the kidneys and body
fluids. Science. 1991;252:1813–1816.
and cardiovascular mortality.38 Overall, these findings widen 20. Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW,
the perspective on ginseng and BP and provide initial insight Mancia G, Nachev C, Palatini P, Parati G, Tuomilehto J, Webster J.
into the effect of ginseng on renal function. Future RCTs Predicting cardiovascular risk using conventional vs ambulatory blood
should evaluate additional doses of NAG that represent its pressure in older patients with systolic hypertension. Systolic hyper-
tension in Europe trial investigators. JAMA. 1999;282:539 –546.
range of intake in the general population. As well, the effect
21. Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez
of P ginseng on BP should be determined through similar DA, Fagard RH, Gheeraert PJ, Missault LH, Braun JJ, Six RO, Van Der
long-term RCTs, because it shows the potential to lower Niepen P, O’Brien E. Prognostic value of ambulatory blood-pressure
BP.16 recordings in patients with treated hypertension. N Engl J Med. 2003;
348:2407–2415.
22. Mussap M, Plebani M. Biochemistry and clinical role of human cystatin c.
Acknowledgments Crit Rev Clin Lab Sci. 2004;41:467–550.
Funding for this study was provided by the Ontario Ministry of 23. Senn S. Cross-Over Trials in Clinical Research. 2nd ed. West Sussex,
Agriculture and Food, as well as by the Ontario Ginseng Growers England: John Wiley and Sons Ltd; 2002.
Association, who also provided the ginseng. 24. Wang X, Sakuma T, Asafu-Adjaye E, Shiu GK. Determination of gin-
senosides in plant extracts from panax ginseng and panax quinquefolius
References l. By lc/ms/ms. Anal Chem. 1999;71:1579 –1584.
1. Yun TK. Brief introduction of panax ginseng. J Korean Med Sci. 2001; 25. Tawab MA, Bahr U, Karas M, Wurglics M, Schubert-Zsilavecz M.
16(Suppl):S3–S5. Degradation of ginsenosides in humans after oral administration. Drug
2. Vuksan V, Sievenpiper JL, Koo VY, Francis T, Beljan-Zdravkovic U, Xu Metab Dispos. 2003;31:1065–1071.
Z, Vidgen E. Am ginseng (panax quinquefolius l) reduces postprandial 26. Fagard R, Brguljan J, Thijs L, Staessen J. Prediction of the actual awake
glycemia in nondiabetic subjects and subjects with type 2 diabetes and asleep blood pressures by various methods of 24 h pressure analysis.
mellitus. Arch Intern Med. 2000;160:1009 –1013. J Hypertens. 1996;14:557–563.
3. Kennedy DO, Scholey AB. Ginseng: Potential for the enhancement of 27. Fagard RH, Staessen JA, Thijs L. Optimal definition of daytime and
cognitive performance and mood. Pharmacol Biochem Behav. 2003;75: night-time blood pressure. Blood Press Monit. 1997;2:315–321.
687–700. 28. Vuksan V, Sievenpiper JL, Sung MK, Di Buono M, Jenkins AL, Stavro
4. Klepser TB, Klepser ME. Unsafe and potentially safe herbal therapies. PM, Leiter LA, Nam KY. Safety and efficacy of korean red ginseng
Am J Health Syst Pharm. 1999;56:125–141. intervention (Saeki): Results of a double-blind, placebo-controlled,
5. Baldwin CA, Anderson LA, Phillipson JA. What pharmacists should crossover trial in type 2 diabetes (abstract). Diabetes. 2003;52:A137.
know about ginseng. Pharm J. 1986;237:583–586. 29. Novelli S. Ginseng from Canada. Bi-Weekly Bulletin of Market Analysis
6. Miller LG. Herbal medicinals: Selected clinical considerations focusing Division Agriculture and Agri-Food Canada. 2003;16:1– 4.
on known or potential drug-herb interactions. Arch Intern Med. 1998; 30. Attele AS, Wu JA, Yuan CS. Ginseng pharmacology: Multiple con-
158:2200 –2211. stituents and multiple actions. Biochem Pharmacol. 1999;58:1685–1693.
7. Siegel RK. Ginseng abuse syndrome. Problems with the panacea. JAMA. 31. Gafner S, Bergeron C, McCollom MM, Cooper LM, McPhail KL, Gerwick
1979;241:1614 –1615. WH, Angerhofer CK. Evaluation of the efficiency of three different solvent
8. Lim MK, Sadarangani P, Chan HL, Heng JY. Complementary and alter- systems to extract triterpene saponins from roots of panax quinquefolius
native medicine use in multiracial Singapore. Complement Ther Med. using high-performance liquid chromatography. J Agric Food Chem. 2004;
2005;13:16 –24. 52:1546–1550.
9. Kim MJ, Lee SD, Kim DR, Kong YH, Sohn WS, Ki SS, Kim J, Kim YC, 32. Dharmananda S. The nature of ginseng. Traditional use, modern research,
Han CJ, Lee JO, Nam HS, Park YH, Kim CH, Yi KH, Lee YY, Jeong SH.
and the question of dosage. HerbalGram. 2002;54:34 –51.
Use of complementary and alternative medicine among Korean cancer
33. Caron MF, Hotsko AL, Robertson S, Mandybur L, Kluger J, White CM.
patients. Korean J Intern Med. 2004;19:250 –256.
Electrocardiographic and hemodynamic effects of panax ginseng. Ann
10. Shin KR, Jho MY, Lee GS, Park SY, Shin SJ. Study of the patterns of
Pharmacother. 2002;36:758 –763.
alternative therapy by the elderly (abstract). Nurs Health Sci. 2002;4:A8.
34. Han K, Shin IC, Choi KJ, Yun YP, Hong JT, Oh KW. Korea red ginseng
11. Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and
water extract increases nitric oxide concentrations in exhaled breath.
alternative medicine use among adults: United States, 2002. Adv Data.
2004;1–19. Nitric Oxide. 2005;12:159 –162.
12. MacLennan AH, Wilson DH, Taylor AW. The escalating cost and prev- 35. Han KH, Choe SC, Kim HS, Sohn DW, Nam KY, Oh BH, Lee MM, Park
alence of alternative medicine. Prev Med. 2002;35:166 –173. YB, Choi YS, Seo JD, Lee YW. Effect of red ginseng on blood pressure
13. Nilsson M, Trehn G, Asplund K. Use of complementary and alternative in patients with essential hypertension and white coat hypertension. Am J
medicine remedies in Sweden. A population-based longitudinal study Chin Med. 1998;26:199 –209.
within the northern Sweden MONICA project. Multinational monitoring 36. Kim ND, Kang SY, Park JH, Schini-Kerth VB. Ginsenoside rg3 mediates
of trends and determinants of cardiovascular disease. J Intern Med. endothelium-dependent relaxation in response to ginsenosides in rat
2001;250:225–233. aorta: Role of k⫹ channels. Eur J Pharmacol. 1999;367:41– 49.
14. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. 37. Coon JT, Ernst E. Panax ginseng: A systematic review of adverse effects
Global burden of hypertension: Analysis of worldwide data. Lancet. and drug interactions. Drug Saf. 2002;25:323–344.
2005;365:217–223. 38. Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB,
15. Stavro PM, Woo M, Heim TF, Leiter LA, Vuksan V. North American Siscovick DS, Stehman-Breen C. Cystatin c and the risk of death and
ginseng exerts a neutral effect on blood pressure in individuals with cardiovascular events among elderly persons. N Engl J Med. 2005;352:
hypertension. Hypertension. 2005;46:406 – 411. 2049 –2060.
Downloaded from http://hyper.ahajournals.org/ by guest on March 6, 2015Long-Term Intake of North American Ginseng Has No Effect on 24-Hour Blood Pressure
and Renal Function
P. Mark Stavro, Minna Woo, Lawrence A. Leiter, Tibor F. Heim, John L. Sievenpiper and
Vladimir Vuksan
Hypertension. 2006;47:791-796; originally published online March 6, 2006;
doi: 10.1161/01.HYP.0000205150.43169.2c
Hypertension is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2006 American Heart Association, Inc. All rights reserved.
Print ISSN: 0194-911X. Online ISSN: 1524-4563
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://hyper.ahajournals.org/content/47/4/791
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Hypertension can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial
Office. Once the online version of the published article for which permission is being requested is located,
click Request Permissions in the middle column of the Web page under Services. Further information about
this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Hypertension is online at:
http://hyper.ahajournals.org//subscriptions/
Downloaded from http://hyper.ahajournals.org/ by guest on March 6, 2015You can also read