User Experiences With and Recommendations for Mobile Health Technology for Hypertensive Disorders of Pregnancy: Mixed Methods Study
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
JMIR MHEALTH AND UHEALTH Jongsma et al
Original Paper
User Experiences With and Recommendations for Mobile Health
Technology for Hypertensive Disorders of Pregnancy: Mixed
Methods Study
Karin Rolanda Jongsma1*, PhD; Josephus F M van den Heuvel2*, MD; Jasmijn Rake2, MD; Annelien L Bredenoord1,
Prof Dr; Mireille N Bekker2, MD, PhD
1
Department of Medical Humanities, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
2
Obstetrics and Gynaecology, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
*
these authors contributed equally
Corresponding Author:
Karin Rolanda Jongsma, PhD
Department of Medical Humanities
University Medical Center Utrecht
Utrecht University
PO Box 85500
Utrecht, 3508 GA
Netherlands
Phone: 31 88 75 51351
Email: k.r.jongsma@umcutrecht.nl
Abstract
Background: Hypertensive disorders of pregnancy (HDP) are a primary cause of adverse maternal and neonatal outcomes
worldwide. For women at risk of hypertensive complications, guidelines recommend frequent surveillance of blood pressure and
signs of preeclampsia. Clinic visits range from every 2 weeks to several times a week. Given the wide ubiquity of smartphones
and computers in most countries and a growing attention for self-management, digital technologies, including mobile health
(mHealth), constitute a promising component of monitoring (self-measured) blood pressure during pregnancy. Currently, little
is known about the experiences of women using such platforms and how mHealth can be aligned with their needs and preferences.
Objective: The objectives were twofold: (1) to explore the experiences of Dutch women who had an increased risk of HDP
with a blended care approach (mHealth combined with face-to-face care) for remote self-monitoring of blood pressure and
preeclampsia symptoms and (2) to formulate recommendations for the use and integration of mHealth in clinical care.
Methods: Alongside a prospective blended care study (SAFE@home study) that monitors pregnant women at increased risk
of HPD with mHealth technology, a mixed methods study was conducted, including questionnaires (n=52) and interviews (n=11).
Results were analyzed thematically.
Results: Of the 4 themes, 2 themes were related to the technologies themselves (expectations, usability), and 2 themes were
related to the interaction and use of mHealth (autonomy and responsibilities of patients, responsibilities of health care professionals).
First, the digital platform met the expectations of patients, which contributed to user satisfaction. Second, the platform was
considered user-friendly, and patients favored different moments and frequencies for measuring their blood pressure. Third,
patient autonomy was mentioned in terms of increased insight about their own condition and being able to influence clinical
decision making. Fourth, clinical expertise of health care professionals was considered essential to interpret the data, which
translates to subsequent responsibilities for clinical management. Data from the questionnaires and interviews corresponded.
Conclusions: Blended care using an mHealth tool to monitor blood pressure in pregnancy was positively evaluated by its users.
Insights from participants led to 7 recommendations for designing and implementing similar interventions and to enhance future,
morally sound use of digital technologies in clinical care.
(JMIR Mhealth Uhealth 2020;8(8):e17271) doi: 10.2196/17271
KEYWORDS
mobile health; hypertension; telemonitoring; ethics; high-risk pregnancy; preeclampsia; digital health
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 1
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
such platforms and how these digital tools can be aligned with
Introduction their needs and preferences.
Mobile health (mHealth) refers to the use of mobile devices, This study aimed, firstly, to explore how pregnant women, who
mobile phones, and wireless technologies to support the have used mHealth as part of a blended care approach for
achievement of health objectives [1]. mHealth is expected to repeated blood pressure measurements and preeclampsia
improve access to care, enhance patient satisfaction, and reduce symptom reporting, experience the use of such technology.
clinic visits and admissions without compromising safety of Second, the study aimed to formulate recommendations based
care and is argued to improve interaction with and participation on these user experiences. Based on the insights originating
of better-informed and more active patients [2-4]. To date, from the users’ experiences, we identified several
mHealth has mostly focused on patients with chronic conditions recommendations to design and implement similar interventions
or healthy individuals to improve healthy lifestyle habits [5-7]. and to enhance future use of digital technology in clinical care.
As in other domains of health care, including pregnancy care,
a shift is currently occurring from hospital-based to home-based Methods
services [8]. In search of improved care for pregnant women,
tailored care with the integration of mHealth has been suggested A mixed methods study, alongside a prospective blended care
as an addition to or partial replacement of frequent prenatal study (SAFE@home study) [16,17], was performed to explore
visits [9]. This approach is called blended care, where digital the understanding of patients’ experiences with mHealth [18,19].
technologies are combined and integrated with face-to-face Data were collected by means of validated questionnaires and
care. While many of these technologies are being developed semistructured in-depth interviews with patients that had
and implemented, little is still known about clinical outcomes experience with mHealth for remote monitoring of HDP, to
including safety, effectiveness, patient satisfaction, and ethical explore their experiences and motivations. The research ethics
considerations. committee of the University Medical Center Utrecht determined
that this study was exempt from the Medical Research Involving
Hypertensive disorders of pregnancy (HDP) are a primary cause
Humans Act (reference number 18-898-C).
of adverse maternal and neonatal outcomes worldwide and occur
in 10% of pregnancies [10]. Risk groups for hypertensive Context of the Blended Care Approach in Prenatal
complications include women with chronic hypertension, Care
diabetes, obesity, renal disease, cardiac disease, and
The overarching prospective study, named Safe@Home,
preeclampsia in a prior pregnancy. The proportion of women
evaluates the use of mHealth technology to remotely monitor
with these risk factors has been steadily rising over recent years
blood pressure and preeclampsia symptoms. The data collected
[10]. For women considered to be at risk, guidelines recommend
within this study were sent by the patient to the digital
frequent observation of the fetal condition and the pregnant
monitoring team, who reviewed the data each day except for
woman’s blood pressure and signs of preeclampsia [11]. Planned
the weekend days. The mHealth technology consisted of an
and unplanned visits can range from every 2 weeks to 4 times
automated blood pressure monitor with Bluetooth connection
a week or even daily. The burden of these recurrent visits is
to a smartphone app for iOS users and a web-based portal for
significant, for both patients and their spouses and family, as
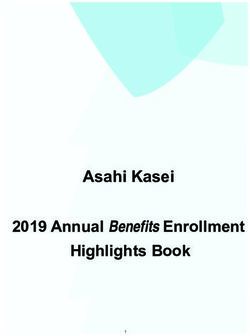
Android users (Figure 1) [16,17]. Digital monitoring started
well as for health care services. However, the incidence of
from 16 weeks gestational age and was continued until delivery,
preeclampsia with severe features is approximately 3% [12],
with interruption in case of hospital admission. Participation in
meaning that a substantial number of monitored women, while
the blended care approach was offered to pregnant women
at risk, do not develop this condition.
whom, at intake, presented with one of the following risk factors
Given the wide ubiquity of smartphones and tablets in most for hypertensive complications: chronic hypertension, history
countries, mHealth is a promising alternative for monitoring of prior preeclampsia, or maternal cardiac or renal disease
hypertension during pregnancy. The latest research has shown requiring prenatal care in our clinic in the University Medical
that pregnant women are willing to undertake repeated Centre Utrecht (university hospital) or Diakonessenhuis Utrecht
self-measurements and a majority of women would like to be (general teaching hospital). Access to a smartphone or tablet
involved in their blood pressure management [13,14] and regard with internet connection and good understanding of either the
remote monitoring important for their pregnancy follow-up Dutch or English language were required. More information
[15]. Little is known about the experiences of women using about the overarching study can be found in [16,17].
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 2
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Figure 1. Example of the blood pressure trend graph in the Luscii app.
A prenatal visit schedule was predefined for this group of assessed the usability of the mHealth technology (via an app or
patients, with a reduced number of visits while continuing web portal) and the connected devices, focusing on the ease of
remote monitoring. Participants were asked to measure their use and given instructions. This usability questionnaire consisted
blood pressure every weekday before 10 am and at least 1 hour of 9 propositions rated on a 5-point Likert scale (strongly agree
after waking up. A 9-question symptom score list could be to strongly disagree) to obtain quantifiable scores (see Textbox
answered in case of hypertension. Predetermined thresholds 1). Furthermore, the use of the blood pressure monitor, usability
(systolic blood pressure >140 mm Hg, diastolic blood pressure of the smartphone app, and content of the app could be rated
>90 mm Hg) or self-reported symptoms of preeclampsia in the on a scale from 1 to 10. The usability questionnaire was
questionnaire resulted in automatically generated alarm signals generated by the study team and not validated before the start
on a monitoring dashboard in the hospital. For health care of the study. The second questionnaire was the validated
providers, a web portal provided online access to Client-Centered Care Questionnaire (CCCQ). The CCCQ was
patient-reported questionnaires and blood pressure data. developed as an instrument to measure client-centeredness as
Members of the digital monitoring team (midwives or obstetric experienced by clients of care organizations and to evaluate the
nurses) reviewed the data every morning from the outpatient effects of interventions aimed at improving the
department. The combination of blood pressure measurement client-centeredness of care services [20]. Themes of the CCCQ
and the presence of symptoms was reviewed and if needed, the include recognition, respect, autonomy, and partnership as
digital monitoring team could consult the obstetrician for advice. perceived by the participants. It consists of 15 questions rated
Subsequently, participants were contacted to advise about on a 5-point Likert scale, ranging from “totally disagree” to
management or follow-up. The platform was embedded into “totally agree” (Multimedia Appendix 1). Results of the CCCQ
prenatal care with the use of a reduced predefined prenatal visit can be interpreted using a unidimensional application. This is
schedule, with regular appointments in the outpatient department done by aggregating all information in one measure and
carried out by hospital midwives and gynecologists (in training). calculating a total test score. This total score expresses care
receivers’ perception of client-centered care, with higher scores
Data Collection representing higher perceived client-centered care. Separate
Questionnaires questions are discussed thematically, in line with the qualitative
results of this study.
At 36 weeks of gestation, two questionnaires were sent by email
to all participants of the prospective study. One questionnaire
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 3
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Textbox 1. Items on the usability questionnaire.
- The system and its use were easy to understand.
- I felt at ease using the system during pregnancy.
- While using the system, I was able to continue my daily activities.
- I am satisfied with the ease of use of this system.
- I would recommend this system to other pregnant women.
- The instructions for use of the blood pressure monitor were clear.
- The instructions for use of the app were clear.
- It was clear when to provide my measurements.
- It was clear when to contact my health care provider.
combined methods of close reading and constant comparison;
Interviews codes emerging from the transcripts were clinical expertise,
Semistructured in-depth interviews were conducted with reassurance, burden and stress, and understanding one’s own
participants of the overarching study after an email invitation. condition. Codes were examined and systematically reviewed
Patients who were willing to be interviewed and were able to for supporting or conflicting evidence concerning emerging
speak either Dutch or English were included in the interview themes and codes. We also explored whether there were any
study through purposive sampling. The topic list was designed differences between nulliparous and parous women and between
to include the motivations, experiences, and perspectives of women with a history of HDP and those without. Where
patients using the platform. The semistructured format provided relevant, we explicitly address these differences in the results.
participants with the opportunity to discuss matters they believed Results are reported using the Consolidated Criteria for
needed emphasis, while offering guidance throughout the Reporting Qualitative research checklist.
interview. Questions for the interview guide were based on
preliminary quantitative results from our questionnaires, which Results
suggested the importance of technical functioning,
communication with care providers, and implications for Patient Characteristics
autonomy. The topic list was expanded based on the literature Of 103 invited participants, a total of 51 participants completed
on ethical aspects of digital health, mHealth, and digital both questionnaires, and one participant only completed the
monitoring. Interviews were conducted by KJ (assistant CCCQ (total n=52). The interviews were conducted with 11
professor) and MD (research assistant), both female researchers women (8 after delivery, 3 during pregnancy) and comprised
with experience in qualitative studies using interviews. No the qualitative part of this study. All interviews (n=11) took
relationship with participants was established prior to the place by phone, as preferred by the participants, and lasted
interviews. The interviews were conducted until saturation was between 35 minutes and 58 minutes. The majority of the
reached, meaning that no new perspectives or themes were interviewed women (8/11) also completed the questionnaires.
found in consecutive interviews and no new themes emerged
from the data. Verbatim transcriptions of interviews and The demographic data of both groups are shown in Table 1.
interviewers’ notes were compared with audio recordings to Obstetric characteristics of relevance to this topic are indicated
check for accuracy. Transcripts were imported into NVivo12 for the interviewees and questionnaire participants (see Table
and analyzed thematically, combining inductive and deductive 1).
analyses. KJ and MD started with an a priori coding scheme to After analysis of the data from the interviews and questionnaires,
allow for deductive coding based on topics described in the we identified 4 themes. Of these, 2 themes were related to the
literature (responsibilities, shared decision making, patient mHealth technology itself (themes 1 and 2), and 2 themes were
empowerment, motivations). Codes and their meanings were related to the interaction with and use of the mHealth technology
discussed among the research team prior to coding to guarantee (themes 3 and 4).
intercoder reliability. The inductive part of the thematic analysis
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 4
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Table 1. Patient characteristics.
Parameters Questionnaires Interviews
(n=52) (n=11)
Maternal age (years), mean (SD) 34.40 (4.127) 34.18 (2.529)
2 24.94 (4.62) 23.88 (2.496)
BMI (kg/m ), mean (SD)
Ethnicity, n (%)
Caucasian 47 (90.4) 11 (100)
Afro-Caribbean 0 (0) 0 (0)
Mediterranean 3 (5.8) 0 (0)
Other 2 (3.8) 0 (0)
Level of education, n (%)
Primary school 1 (1.9) 0 (0)
Secondary school 4 (7.7) 0 (0)
Middle-level applied education 14 (26.9) 3 (27.3)
Higher-level applied education 17 (32.7) 6 (54.5)
Scientific education (university) 13 (25.0) 2 (18.2)
Unknown 3 (5.8) 0 (0)
Nulliparous, n (%) 19 (36.5) 2 (18.2)
HDPa prior pregnancy, n (%)
None 14 (26.9) 3 (27.3)
Chronic hypertension 1 (1.9) 1 (9.1)
Gestational hypertension 5 (9.6) 2 (18.2)
Preeclampsia/HELLPb 13 (25.0) 3 (27.3)
Not applicable (nulliparous) 19 (36.5) 2 (18.2)
Initial diagnosis at start of SAFE@home study, n (%)
Preeclampsia in prior pregnancy 10 (19.2) 2 (18.2)
Chronic hypertension 17 (32.7) 5 (45.5)
Cardiac disease 17 (32.7) 3 (27.3)
Renal disease 8 (15.4) 1 (9.1)
HDP current pregnancy, n (%)
None 23 (44.2) 2 (18.2)
Chronic hypertension 14 (26.9) 3 (27.3)
Gestational hypertension 6 (11.5) 2 (18.2)
Preeclampsia 9 (17.3) 4 (36.4)
a
HDP: hypertensive disorders of pregnancy.
b
HELLP: hemolysis, elevated liver enzymes, low platelet count.
client-centeredness of the blended care approach, based on the
Theme 1: Expectations of and Satisfaction With the CCCQ, was rated at an average 57.5 of 75 points (range 36-75
mHealth Technology points), which translates to a score of 77 from a possible total
Quantitative Analysis score of 100. This total CCCQ score was comparable between
nulliparous women (score of 76, n=19) and parous women (score
Analysis of the usability questionnaire showed that almost all
of 77, n=33). Of all parous women, women with prior HDP
participants (49/51, 96%) felt comfortable using mHealth. The
(19/33) scored the CCCQ slightly higher (score of 79/100) than
vast majority (45/51, 88%) would recommend it to their friends
those without experience with HDP (14/51; score of 75/100).
and family, especially participants who had been pregnant before
(97% of multiparous vs. 74% of nulliparous women). Overall,
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 5
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Qualitative Analysis experienced symptoms associated with preeclampsia. Also,
In order to understand what is important for mHealth users, we when their measurement indicated normal blood pressure, the
asked the interview participants what their expectations were digital monitoring was considered useful and reassuring, because
before they started using the digital technology in the it would indicate that the symptoms were not caused by
Safe@Home study and whether their expectations were met. hypertension. Comparable to the results of the questionnaire,
The most often mentioned motivations to start using the all interviewed women would recommend the system to other
technology were the expected reassurance of being closely pregnant women.
monitored by a health care professional (9/11; 2 nulliparous Some reflections of the interview participants indicated that
and 7 parous), better pregnancy outcomes (6/11; 3 with a history their expectations did not always match their experiences. A
of hypertension and 3 with a history of HPD), and the prospect few women were surprised by health care professionals calling
of fewer hospital visits (5/11; none with a history of HPD). This when they did not expect it, while at other times, they were not
aligned well with their experiences; most interview participants called by the health care professional when they expected it
(8/11) reported they felt reassured and safe because of the close based on their uploaded blood pressure data (2/11; both with a
monitoring by their obstetric care professional. The use of history of hypertension). Participants who needed reassurance
mHealth reduced the frequency of visits, which contributed to that their blood pressure or symptoms were nothing to worry
the users’ wellbeing and a more relaxed pregnancy experience about sometimes called the hospital themselves. Furthermore,
(9/11; 2 nulliparous and 7 parous). The blended care approach one interview participant needed several extra hospital visits
also enabled timely preventative measures or interventions, because of hard-to-control hypertension, eventually leading to
which resulted in early detection of abnormalities or risks (2/11). hospital admission. As a result, she was somewhat disappointed
All interview participants considered it a benefit to be able to that the digital monitoring platform did not live up to her
measure their own blood pressure, especially when they expectations (P5, Table 2).
Table 2. Quotes illustrating interviewees’ expectations and satisfaction.
Topic Quotes
Reassurance More relaxed, I’d say. I haven’t worried at all about my blood pressure. I considered it under control […] Because you
do it continuously [the measurements], it reassures you. (P1)
It is very pleasant and extremely easy. It’s reassuring that you are being monitored [by health care professionals]. (P11)
Frequency of visits It has given me peace of mind over all those months, primarily because of the significantly reduced number of clinical
visits. (P1)
It is ironic; we expected it because it was announced like that, that we would have to visit the hospital less often, because
we would be monitored via the app, but it resulted in more frequent contact. (P5)
Furthermore, the vast majority of participants (47/51, 92%) was
Theme 2: Usability of the mHealth Tool satisfied with the usability of the mHealth technology; 81%
Quantitative Analysis (41/51) of the participants said the daily measurements took ≤5
minutes a day (average 4.57 minutes, range 3-15 minutes), and
Analysis of the questionnaires showed that nearly all participants
women could easily continue their daily routine while using the
considered the user instructions of the blood pressure monitor
technology (50/51, 98%). Some found it difficult to combine
(49/51, 96%) and smartphone app or website (48/51, 94%) to
digital monitoring with their daily routine (5/51, 10%).
be clear and understandable. Similarly, almost everyone (49/51,
96%) found it easy to learn how to use the mHealth technology On a scale from 1 to 10, the blood pressure monitor was rated
(Figure 2). at 8.5 (range 6-10), usage of the smartphone app at 7.6 (range
1-10), and content of the smartphone app at 7.8 (range 1-10).
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 6
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Figure 2. Results from the user satisfaction questionnaire.
about her medical condition (1/11; with a history of HPD) or
Qualitative Analysis to allow it to become a habit in their daily routine (2/11).
Similar to the questionnaire, interview participants (6/11) Multiple mHealth users (4/11) measured several times a day
considered the app to be “modern” and easy to use; all users of when they experienced symptoms of preeclampsia or
the web portal (4/11) suggested that an Android app would be hypertension. At the same time, others (6/11; 4 with a history
more user-friendly. Moreover, the iOS app was regarded to be of HDP) mentioned that daily measurements were too
comprehensive; the symptom survey was considered short but burdensome or medicalizing, especially when they perceived
clear and easy to complete — it did not take them much effort their symptoms or blood pressure to be stable. A couple of
and time (4/11; 2 with a history of HPD and 2 without). Other interviewees (2/11) mentioned they missed the mHealth tool
technical aspects that contributed to the ease of use were the after giving birth and would have wanted to continue to measure
reminder function, automatic Bluetooth synchronization, and during their postpartum period.
perceived high accuracy of the measurement. A couple of
participants (2/11) noted that technical understanding of the A couple of women (2/11) mentioned technical errors in the
functioning of the app was irrelevant for their user experience. synchronization of their measurements with the system used in
the hospital. Furthermore, a couple of others (2/11; both parous
A few users mentioned that measuring early in the morning was and with a history of hypertension) felt that the symptom score
not always easy to combine with either commuting to work or list to monitor preeclampsia signs was at times confusing
“family rush hour” in the morning (3/11) or not representative, because some questions did not match the specific pregnancy
as their morning blood pressure was naturally low (1/11). These term. In particular, the question “Can you feel the baby move?”
users preferred to have the option to measure in the evening was considered to be upsetting in the first trimester. Also, one
instead of the morning. Most considered measuring 5 times a interview participants considered the orange or red lights
week sufficient; a couple of interview participants measured stressful, as she never saw a green light because of her high
every day, even during weekends, either because of worries values (P9, with a history of HPD; Table 3).
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 7
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Table 3. Quotes illustrating interviewee perspectives on the usability of the mHealth tool.
Topic Quote
App vs web portal At first, I used the web portal, but when I had a closer look, I realized that the app is much easier, because it
automatically synchronizes. It is so easy! (P1)
Frequency of measurement Before I started, I thought it would be burdensome to measure my blood pressure every day and was not convinced
that it would be necessary. [...] But eventually, it was very easy. It became part of my routine to measure my
blood pressure in the morning before going to work or before bringing the children to school. (P8)
The app was meant to be used in the morning, which was somewhat a downside, because my blood pressure is
fine in the morning. (P3)
While I was using it, no [I did not experience anything unexpected], but after giving birth and being back home,
I continued measuring with my own device, because I missed that sort of information about my body. (P7)
Questions suitable to term Those questions did not really match with being in the first trimester. Because it asked for example “do you feel
contractions,” “do you still feel the baby move,” But [at that time], I hardly had a belly, and I couldn’t even feel
the baby yet. [..] I found it difficult and puzzling. (P10)
Alarms “Those lights [on the blood pressure device], they should get rid of in favor of people who are easily stressed
out. They should rather show you a green light when you’re fine, orange when there are problems, and red when
things are bad. [..] It showed orange so often. Since my blood pressure has been high my whole life, you feel
like there is a continuous alarm, while yeah, that was not really the case.” (P9)
Qualitative Analysis
Theme 3: Autonomy and Responsibility of Patients
Interview participants noted two dimensions related to patient
Quantitative Analysis autonomy. First, all interview participants (11/11) mentioned
Respondents of the questionnaires were positive about their role that mHealth helped to be informed about HDP. Insights on
within the blended care approach. The majority of the blood pressure over time, as displayed in a trend line in their
participants felt they were given sufficient opportunity to draw app, was especially considered to be informative (6/11; all
on their own knowledge and experience (40/51, 77%) and to parous). Such information raised awareness about the symptoms
decide about the kind of care they receive (43/52, 83%). of HDP and when to report to health care professionals (4/11).
Furthermore, they felt they were given enough opportunity to Some interview participants (2/11) argued that these insights
do what they were capable of doing themselves (47/52, 90%). are paired with responsibilities to carefully measure blood
However, only half of the participants (26/52, 50%) felt like pressure and to contact the health care professional when
they were given enough opportunity to arrange and organize symptoms increase.
prenatal care themselves. Some (30/52, 57%) would like even A second aspect related to patient autonomy mentioned by
more influence in clinical decision making and felt that health participants was that the use of mHealth contributed to them
care professionals are sometimes too quick to deny a possibility. being in control of their own health and to bring their own
A minority of the participants (21/52, 40%) felt like they had a perspectives to the fore in consultations with health care
say in deciding when the care was provided. professionals (7/11). mHealth allowed them to monitor their
own symptoms and, when necessary, adapt their behavior (4/11),
for example with regard to activities or medication (P8, Table
4).
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 8
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Table 4. Quotes illustrating interviewee perspectives on autonomy and responsibilities of patients.
Topic Quote
Being informed I experienced that I thought I was going to measure hypertension because I felt a headache, but then I didn’t measure
anything abnormal. That is odd. But exactly because of such experiences, I consider it beneficial to be able to measure,
because it provided objective information to really judge it. Because I find it difficult to determine what is the matter,
simply by how I feel. (P8)
I then understood, you know, why they [health care professionals] ask you all these questions and that these are relevant.
Because of the symptom score list or due to hypertension and related symptoms of preeclampsia, that I became aware
that once you experience such symptoms, you shouldn’t think it’s normal, but that you have to inform health care pro-
fessionals. (P2)
Information for lifestyle It is information, you know. I had to take care of my activity level; when I did not measure hypertension, I would go
outside for example. […]. And in case I would measure hypertension, I would take it easy and ask my husband to take
care of the children. It provides information relevant for such activities. That was very helpful. (P8)
Responsibilities [..] but it is also your own responsibility, the responsibility of the mother or the pregnant woman. Not only because you
know your body best, but also because you become aware of aspects because of this research study. And then it’s my
responsibility to discuss it with the health care professional. (P2)
Control You both have access to the information. What I see in my overview, the physician can also see, so you can also look
at it together. I got the impression that more deliberation is possible, that you do it together like how should I interpret
this and the physician can explain it for example. (P8)
have invaluable clinical expertise to oversee the implications
Theme 4: Health Care Professionals’ Expertise and of the measurements, as well as to decide the need for additional
Responsibilities tests, the interval of clinical visits, and medication or
Quantitative Analysis hospitalization. The follow-up initiated by health care
professionals — either by phone or via clinical visits —
After starting the digital monitoring, it was clear for the majority
contributed to the feeling of being well taken care of and met
of the participants when the digital monitoring team needed to
the interviewees’ expectations regarding responsibilities (5/11).
receive their measurements (49/51, 96%) and when to contact
Patients also mentioned that it should remain the health care
the physician regardless of their data (42/51, 82%). They felt
professionals’ responsibility to undertake action when the
that their personal wishes were sufficiently considered by the
measurements deviate from the norm (5/11). They felt relieved
health care professionals (46/52, 89%). Most of the survey
that monitoring and resulting action are not solely the patient’s
respondents said they could tell that their obstetric care
responsibility (11/11).
professional really listened to them (50/52, 96%) and that they
were given enough opportunity to say what kind of care they Moreover, patients were appreciative that health care
needed (47/52, 90%). professionals acted if a patient would underestimate the severity
of their situation (3/11). Patients argued that important decisions
Qualitative Analysis about their condition cannot exclusively be based on the
In addition to the findings of the quantitative research, information from the tool, but an expert’s clinical view is
interviewees showed that they consider the expertise of the required for interpretation and to make personalized treatment
health care professionals important in monitoring HDP. All decisions (5/11; Table 5).
interview participants (11/11) said that health care professionals
Table 5. Quotes illustrating interviewees’ perspectives on expertise and responsibilities of health care professionals.
Topic Quote
Medical expertise Well, for me, those data, I’m not trained as a health care professional, to interpret my data. I, myself, had the [possibil-
ity] to see how my blood pressure developed over time. But the idea that health care professionals see my data and can
interpret it and can ask you to come to the hospital when necessary, that is comforting. (P2)
[..] and that they can interpret it. Like for me, it was the case that it [blood pressure] was higher than 90, even if 90 is
the threshold value for me, but [they explained] that for me, you see sometimes other things happening. Then I know
that, you know, it’s very helpful when a physician helps me and interprets the data. I mean, that they don’t simply tell
and stick to the threshold values, but also interpret it in your specific situation. I believe the shared effort lies in me
conducting the measurements and supplying that information. (P8)
[..] it’s a shared effort. But I think the physician is leading because they know best. I mean, I know more or less which
medication I take now and what sort of effect it has on me. But I don’t know, for example, whether or when I can stop
taking medications and what consequences it would have; I haven’t studied for that. (P4)
Active monitoring I really like having been called after [by a nurse], because then you have confirmation that they will undertake action
when it is necessary. [..] I think it was great, that in that way also really something is done with the data you collect
every day. (P7)
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 9
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
overall very satisfied with the easy-to-use technology. mHealth
Discussion was considered to support patient autonomy by providing
This study analyzed user experiences with a blended care information and ways to be in control, but the interpretation of
approach for the monitoring of HDP (Safe@Home study). the measurements requires the involvement of health care
Overall, the results of the questionnaires and interviews professionals. Participants also noted a few possibilities for
corresponded and were supplementary. The effects of using improvement. With the focus on future development and
mHealth met the expectations of the participants, who were implementation of mHealth in care, we extracted multiple
recommendations from our results (see Textbox 2).
Textbox 2. Recommendations for the future use and implementation of mHealth technologies in clinical care.
1. Be modest in the communication regarding expected group benefits of the digital health technology to prevent disappointing individual patients
who do not experience these specific benefits.
2. Provide the user insight into the data; in particular, a graphic representation over time is a helpful method to foster patient knowledge and can
support patients to participate in clinical decision making.
3. The mHealth data should be integrated in (electronic) health records and should be accessible to all health care professionals that are engaged in
care.
4. The health care professionals should remain responsible for the interpretation of data obtained via digital monitoring, as the clinical expertise of
health care professionals is necessary for the early detection of abnormalities and clinical decision making.
5. Health care professionals should be aware of (pregnant) patients’ willingness and capability to self-measure their blood pressure at home.
6. Symptom score lists and blood pressure thresholds should be personalized, meaning that the questions should be adapted to the pregnancy term
and thresholds should be set to fit the user’s situation.
7. The moment and frequency of measurement should be communicated clearly but should also be sensitive and adaptable to the daily life of the
user.
at the delivery date, but should be available postnatally, which
Our Findings in Context was also expressed by our interview participants [21,22].
Currently, several digital technologies are being developed that
moderate or replace traditional clinical care. The study described Opportunities for and Challenges With Blended Care
here is an excellent example of such digital health technology Approaches in Clinical Care
in the clinical context that replaces some of the care traditionally With the rapid development and implementation of digital
provided in the clinical setting with digital monitoring at home. technologies in health care settings, the need for ethical guidance
Our study confirmed several findings described by other digital and practical recommendations for the implementation of such
monitoring studies. Some comparable studies have reported on technologies, including mHealth, is widely acknowledged by
remote blood pressure monitoring in pregnancy, without patients, health care professionals, and influential advisory
in-clinic monitoring by care professionals [21,22]. For a councils [23-25]. With the implementation of these technologies,
comparable intervention with clinical monitoring, only survey it becomes possible to move beyond mere speculative debates
data were reported [15]. Our study confirmed that pregnant about the opportunities and challenges of mHealth and to
women at risk of HDP are willing to participate in investigate how the practice is developing. Our study explored
self-monitoring services and are capable of bearing the both user experiences and the expectations of users prior to
responsibilities of measuring their own blood pressure using mHealth tools for digital monitoring. User experiences
[15,21,22]. Our study confirmed that women who experienced depend not only on the quality of the technology but also on
HDP in a prior pregnancy, in particular, were strongly in favor the expectations one has before using it. Investigating both
of blended care approaches in prenatal care [22]. A comparable expectations and experiences is helpful, not only to understand
intervention for pregnant women with hypertension that included what may motivate pregnant women to use such technologies
remote monitoring of blood pressure and monitoring by health but also to assess whether these tools live up to users’
care professionals reported that 83% of the participants expectations. Our study provides several insights in that respect:
experienced a feeling of safety and that 68% preferred to be less frequent hospital visits and better-informed patients were
contacted within 12 hours after the measurement in case of often mentioned as factors contributing to the satisfaction with
abnormal measurements, preferably by their midwife or this technology. This shows that some of the widely discussed
obstetrician [15]. Our study found comparable feelings of promises of mHealth were met in our study. Other claims about
appreciation and safety among the users, partly because of the mHealth, such as increased accessibility, cost-effectiveness,
follow-up by health care professionals by phone or via clinical and more empowered patients [1,2], were not (fully)
visits. Self-measuring was found to be reassuring; when substantiated by our study.
abnormal values were detected as women took and interpreted
their own measurement, it was clear for the participants when Furthermore, our study indicates that ethical guidance for the
to contact the clinic [21]. Other studies have also found that use of digital technologies in health care settings differs in
women prefer that blood pressure monitoring should not stop significant ways from concerns about digital health consumers.
Using digital technologies, including mHealth, in health care
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 10
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
settings raises a wider range of ethical challenges than have Strengths and Limitations
been described in the consumer context [26,27]. Aside from This is a mixed methods study that benefits from reducing
concerns about effectiveness, privacy, and safety, the health weaknesses inherent to both methods; it expands understanding,
care context requires us to carefully assess the delegation of while also being comprehensive. Approximately half of the
responsibilities to patients, influence on patient autonomy, and total users of the mHealth technology filled out the validated
proportionality of burden and benefits. Regarding the delegation questionnaires. The sample of interviewees was representative
of responsibilities, our study showed that users are able to bear of the participants of the questionnaires in terms of age, BMI,
the responsibility for measuring their own blood pressure, but education level, and underlying conditions (Table 1). The
they did not feel able to bear the responsibility of interpreting findings of the survey and interviews were supplementary and
their own data. Clinicians play an important role in the helped to better understand what and for which reasons the
responsible use and implementation of these technologies. This mHealth tool was appreciated, which can inform future mHealth
indicates that careful consideration is required regarding which health interventions.
tasks and responsibilities can be delegated to technology (instead
of face-to-face care) and which can be delegated to patients Our results must be interpreted in the context of the following
(instead of the health care professionals) without compromising limitations. Selection bias (self-selection) might have influenced
safety or quality of care. Digital technologies, including the results, as participants of the prospective study agreed to
mHealth, are not a stand-alone solution in the clinical context take part in this innovative strategy with digital monitoring and
and need to be supplemented with clinical expertise. With regard may thus have a positive attitude in general to mHealth.
to the influence on patient autonomy, our study has supported Furthermore, the women willing to participate in this study may
evidence that patients can become more familiar with their own have had a relatively positive experience with this specific
body and disease symptoms and are able to use this information technology. Also, the experience of participants could have
in adjusting their behavior or to deliberate with physicians. It been biased by the outcome of their pregnancy. However, as
is important to recognize that supporting and respecting patient the findings of the questionnaires (collected during pregnancy)
autonomy are not completely in their own hands. Health care and the interview data (8 postpartum, 3 during pregnancy)
professionals involved in blended care play a crucial role. Not correspond, the influence may be marginal. The interviewed
only will health care professionals have to recognize and respect patients were fairly highly educated and may therefore not be
wishes of autonomous persons but will also have to navigate representative of pregnant women in other socioeconomic
between the standardized way of measuring, supported by digital situations. This explorative study has a relatively small sample
technology, while still being able to personalize the analysis size; in both the quantitative and qualitative aspects of the study,
and interpretations to the interests and needs of a specific patient. the provided ratios and percentages were not statistically
Lastly, while mHealth technologies have several benefits, such powered and therefore cannot be fully generalized to other
as accessibility of information for both patients and health care populations or care settings. Although saturation was reached
professionals, less frequent hospital visits, and better on the identified codes and themes, further research could
understanding of one’s own conditions, these benefits need to investigate these topics in more depth.
outweigh the burden of using these technologies (eg, time
Conclusions and Recommendations
investment, user friendliness). Overall, our participants were
very positive and satisfied with the mHealth technology, but Our study explored the perspectives of pregnant women
the interview participants who felt their blood pressure was regarding the use of mHealth in a blended care approach to
stable because of prescribed medication argued that the burden remotely monitor blood pressure in pregnancy. Based on the
of measuring every day became somewhat disproportionate. experiences of the users, several recommendations have been
Less frequent measurements may be a way to balance the burden formulated. These recommendations draw on the needs,
and benefits for these groups. It also indicates that high levels experiences, and views of the patients, meaning that following
of satisfaction with this blended care approach might be specific these recommendations will contribute to better-aligned and
to the high-risk population that was selected for this approach. patient-centered care. These recommendations can help other
For the high-risk population, there is much to gain in terms of scholars or physicians to guide the process of implementation
both health outcomes and time investment, but the balance may and design of similar mHealth technologies.
tip differently for medium-risk to low-risk groups.
Acknowledgments
This project was partly funded by a Child Health Boost grant of the University Medical Center Utrecht in 2018. We would like
to thank all participants in this study for sharing their experiences and Melodi Dekker for her support in the analysis of the
interview material.
Conflicts of Interest
None declared.
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 11
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
Multimedia Appendix 1
Client-centered-care questionnaire (CCCQ).
[PDF File (Adobe PDF File), 393 KB-Multimedia Appendix 1]
References
1. mHealth: New horizons for health through mobile technologies: second global survey on eHealth. Geneva: World Health
Organization; 2014:156-192.
2. Topol E. The Patient Will See You Now: The Future of Medicine is in Your Hands. Jackson, TN: Ingram Publisher Services;
2015.
3. World Health Organization. WHO Guideline: Recommendations on digital interventions for health system strengthening.
2019. URL: https://www.who.int/reproductivehealth/publications/digital-interventions-health-system-strengthening/en/
[accessed 2020-07-16]
4. European Commission. Green Paper: mobile Health ("mHealth"). Shaping Europe’s digital future. 2014 Apr 10. URL:
https://ec.europa.eu/digital-single-market/en/news/green-paper-mobile-health-mhealth [accessed 2020-07-16]
5. Mol A. What Diagnostic Devices Do: The Case of Blood Sugar Measurement. Theoretical Medicine and Bioethics 2000
Jan;21(1):9. [doi: 10.1023/a:1009999119586]
6. Lupton D. The digitally engaged patient: Self-monitoring and self-care in the digital health era. Soc Theory Health 2013
Jun 19;11(3):256-270. [doi: 10.1057/sth.2013.10]
7. Pinnock H, Hanley J, McCloughan L, Todd A, Krishan A, Lewis S, et al. Effectiveness of telemonitoring integrated into
existing clinical services on hospital admission for exacerbation of chronic obstructive pulmonary disease: researcher blind,
multicentre, randomised controlled trial. BMJ 2013 Oct 17;347(3):f6070-f6070 [FREE Full text] [doi: 10.1136/bmj.f6070]
[Medline: 24136634]
8. van den Heuvel JF, Groenhof TK, Veerbeek JH, van Solinge WW, Lely AT, Franx A, et al. eHealth as the Next-Generation
Perinatal Care: An Overview of the Literature. J Med Internet Res 2018 Jun 05;20(6):e202 [FREE Full text] [doi:
10.2196/jmir.9262] [Medline: 29871855]
9. Woo VG, Lundeen T, Matula S, Milstein A. Achieving higher-value obstetrical care. Am J Obstet Gynecol 2017
Mar;216(3):250.e1-250.e14. [doi: 10.1016/j.ajog.2016.12.033] [Medline: 28041927]
10. Hutcheon JA, Lisonkova S, Joseph K. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy.
Best Pract Res Clin Obstet Gynaecol 2011 Aug;25(4):391-403. [doi: 10.1016/j.bpobgyn.2011.01.006] [Medline: 21333604]
11. Hypertension in pregnancy: diagnosis and management: NICE guideline [NG133]. National Institute for Health and Care
Excellence. 2019 Jun 25. URL: https://www.nice.org.uk/guidance/ng133 [accessed 2020-07-16]
12. Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph K. Maternal Morbidity Associated With Early-Onset and
Late-Onset Preeclampsia. Obstetrics & Gynecology 2014;124(4):771-781. [doi: 10.1097/aog.0000000000000472]
13. Hodgkinson JA, Tucker KL, Crawford C, Greenfield SM, Heneghan C, Hinton L, et al. Is self monitoring of blood pressure
in pregnancy safe and effective? BMJ 2014 Nov 18;349(1):g6616-g6616. [doi: 10.1136/bmj.g6616] [Medline: 25406132]
14. Magee LA, von Dadelszen P, Chan S, Gafni A, Gruslin A, Helewa M, Group For The CHIPS Pilot Trial Collaborative.
Women's views of their experiences in the CHIPS (Control of Hypertension in Pregnancy Study) Pilot Trial. Hypertens
Pregnancy 2007 Jul 07;26(4):371-387. [doi: 10.1080/10641950701547549] [Medline: 18066957]
15. Lanssens D, Vandenberk T, Lodewijckx J, Peeters T, Storms V, Thijs IM, et al. Midwives', Obstetricians', and Recently
Delivered Mothers' Perceptions of Remote Monitoring for Prenatal Care: Retrospective Survey. J Med Internet Res 2019
Apr 15;21(4):e10887 [FREE Full text] [doi: 10.2196/10887] [Medline: 30985286]
16. van den Heuvel JF, Kariman SS, van Solinge WW, Franx A, Lely AT, Bekker MN. SAFE@HOME - Feasibility study of
a telemonitoring platform combining blood pressure and preeclampsia symptoms in pregnancy care. Eur J Obstet Gynecol
Reprod Biol 2019 Sep;240:226-231. [doi: 10.1016/j.ejogrb.2019.07.012] [Medline: 31330428]
17. van den Heuvel JFM, Lely AT, Huisman JJ, Trappenburg JCA, Franx A, Bekker MN. SAFE@HOME: Digital health
platform facilitating a new care path for women at increased risk of preeclampsia - a case-control study. Pregnancy Hypertens
2020 Jul 18;22:30-36 [published online ahead of print, 2020 Jul 18]. [doi: 10.1016/j.preghy.2020.07.006] [Medline:
32717653]
18. Lilford RJ, Foster J, Pringle M. Evaluating eHealth: how to make evaluation more methodologically robust. PLoS Med
2009 Nov 24;6(11):e1000186 [FREE Full text] [doi: 10.1371/journal.pmed.1000186] [Medline: 19956674]
19. Jaspers MW. A comparison of usability methods for testing interactive health technologies: methodological aspects and
empirical evidence. Int J Med Inform 2009 May;78(5):340-353. [doi: 10.1016/j.ijmedinf.2008.10.002] [Medline: 19046928]
20. de Witte L, Schoot T, Proot I. Development of the client-centred care questionnaire. J Adv Nurs 2006 Oct;56(1):62-68.
[doi: 10.1111/j.1365-2648.2006.03980.x] [Medline: 16972919]
21. Hinton L, Tucker KL, Greenfield SM, Hodgkinson JA, Mackillop L, McCourt C, et al. Blood pressure self-monitoring in
pregnancy (BuMP) feasibility study; a qualitative analysis of women's experiences of self-monitoring. BMC Pregnancy
Childbirth 2017 Dec 19;17(1):427. [doi: 10.1186/s12884-017-1592-1] [Medline: 29258469]
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 12
(page number not for citation purposes)
XSL• FO
RenderXJMIR MHEALTH AND UHEALTH Jongsma et al
22. Sheehan E, Khalil A, Kay L. Using a smartphone app to identify signs of pre-eclampsia and/or worsening blood pressure.
British Journal of Midwifery 2019 Feb 02;27(2):92-99. [doi: 10.12968/bjom.2019.27.2.92]
23. Lucivero F, Jongsma KR. A mobile revolution for healthcare? Setting the agenda for bioethics. J Med Ethics 2018 Oct
15;44(10):685-689 [FREE Full text] [doi: 10.1136/medethics-2017-104741] [Medline: 29907579]
24. Ruckenstein M, Schüll ND. The Datafication of Health. Annu. Rev. Anthropol 2017 Oct 23;46(1):261-278. [doi:
10.1146/annurev-anthro-102116-041244]
25. The Nuffield Council on Bioethics. The collection, linking and use of data in biomedical research and health care: ethical
issues. 2015 Mar 02. URL: https://www.nuffieldbioethics.org/publications/biological-and-health-data [accessed 2020-07-26]
26. Lanzing M. “Strongly Recommended” Revisiting Decisional Privacy to Judge Hypernudging in Self-Tracking Technologies.
Philos. Technol 2018 Jun 6;32(3):549-568 [FREE Full text] [doi: 10.1007/s13347-018-0316-4]
27. Gostin LO, Halabi SF, Wilson K. Health Data and Privacy in the Digital Era. JAMA 2018 Jul 17;320(3):233-234. [doi:
10.1001/jama.2018.8374] [Medline: 29926092]
Abbreviations
CCCQ: Client-Centered Care Questionnaire
HDP: hypertensive disorders of pregnancy
mHealth: mobile health
Edited by G Eysenbach; submitted 01.12.19; peer-reviewed by J Graf, M Feisst, A von Au; comments to author 18.04.20; revised
version received 05.05.20; accepted 13.05.20; published 04.08.20
Please cite as:
Jongsma KR, van den Heuvel JFM, Rake J, Bredenoord AL, Bekker MN
User Experiences With and Recommendations for Mobile Health Technology for Hypertensive Disorders of Pregnancy: Mixed Methods
Study
JMIR Mhealth Uhealth 2020;8(8):e17271
URL: https://mhealth.jmir.org/2020/8/e17271
doi: 10.2196/17271
PMID:
©Karin Rolanda Jongsma, Josephus F M van den Heuvel, Jasmijn Rake, Annelien L Bredenoord, Mireille N Bekker. Originally
published in JMIR mHealth and uHealth (http://mhealth.jmir.org), 04.08.2020. This is an open-access article distributed under
the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted
use, distribution, and reproduction in any medium, provided the original work, first published in JMIR mHealth and uHealth, is
properly cited. The complete bibliographic information, a link to the original publication on http://mhealth.jmir.org/, as well as
this copyright and license information must be included.
https://mhealth.jmir.org/2020/8/e17271 JMIR Mhealth Uhealth 2020 | vol. 8 | iss. 8 | e17271 | p. 13
(page number not for citation purposes)
XSL• FO
RenderXYou can also read