The Journal of COVER STORY: Pivoting to Telehealth-Overnight, p.14 - America's Physician Groups
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
The Journal of Volume 14 • No. 1 • Summer 2020 COVER STORY: Pivoting to Telehealth– Overnight, p.14 Post-Pandemic Partnerships, p.16 Choosing an MSO, p.34
Looking to avoid risk?
WE CAN SHOW
YOU THE WAY.
We’re taking the mal out of malpractice insurance.
Thanks to our national scope, regional experts, and
data-driven insights, we’re uniquely positioned to spot
trends early. We shine a light on risks that others can’t
see, letting you focus on caring for patients instead
of defending your practice. It’s a stronger vision that
creates malpractice insurance without the mal.
Join us at thedoctors.com
The Doctors Company is proud to
be a partner and Elite Sponsor of
America’s Physician Groups.
7490_Journal_APG_ORM_Summer2020_0820_v1.indd 1 8/7/20 2:00 PMAT ALIGNMENT HEALTH PLAN,
We promise to
make health care
as convenient and
hassle-free as possible.
We promise to
take care of our
members, keeping an
eye on their health
around the clock.
We provide 24/7
concierge service
for anytime access to
doctors, transportation
assistance, help with
questions and more!
are you in
A L I G N M E N T ?
( 8 4 4 ) 3 1 0 - 2 247 A l i g n m e n t H e a l t h c a re.co m14
TABLE OF CONTENTS
ON THE COVER
Bill Wulf, MD
The APG Chair-Elect shares how Central Ohio
Primary Care pivoted to telehealth—overnight.
The Journal of
DEPARTMENTS 24
Preemptive Compliance Reviews:
6 A Business Development Strategy
From the President
Publisher
Valerie Okunami 26
Editor-in-Chief
Don Crane
Editorial Advisory Board
8 Do Oversight Programs Have
a Measurable ROI?
Lura Hawkins, MBA News and Events
Dianne Glover, MPH
Mary Kay Payne, Arch Health Partners
Managing Editor
Lura Hawkins, MBA
10 32
Important Considerations Before
Contributing Writers Federal Policy Update
Brad Ayres Accepting Delegation
Bill Barcellona
APG Advocates for COVID-19 Relief
Ute Burness, RN
Don Crane
Garrett Eberhardt
Russ Foster 12 34
Justin Frazer
Choosing an MSO: 10 Factors
Policy Briefing
Dawn Maroney to Consider
Sheila Stephens MHA Grad Implements Telehealth
Bill Wulf, MD
During COVID-19
Journal of America’s Physician
Groups is published by
Valerie Okunami Media
PO Box 674, Sloughhouse,
CA 95683
21
Phone 916.761.1853 APG Member List
apg.org
Please send press releases and editorial
inquiries to Journalofapg@gmail.com or
c/o Journal of America’s Physician Groups,
FEATURES
915 Wilshire Blvd., Suite 1620,
Los Angeles, CA 90017
For advertising, please send email to
vokunami@netscape.com
16
Payer-Provider Partnerships in a
Subscription rates: $32 per year; $58 two
years; $3 single copy. Post-Pandemic World
Advertising rates on request. Bulk third class
18
mail paid in Jefferson City, MO
Every precaution is taken to ensure the
accuracy of the articles published in Journal
of America’s Physician Groups. How Will COVID-19 Impact
Opinions expressed or facts supplied by its Business Insurance Premiums?
authors are not the responsibility of Journal
of America’s Physician Groups.
© 2020, Journal of America’s Physician
Groups. All rights reserved.
Reproduction in whole or in part without
written permission is strictly prohibited.
4 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020Independent and Supported That’s what it means to be a Hill Physicians provider. As the largest IPA in Northern California, our physicians provide care to over 350,000 patients. We give you the support you need so you can remain independent and focus on what matters most: high-quality patient care. A leader in the industry, Hill Physicians offers: • A 30-year history of fiscal strength under the leadership of an all-physician Board of Directors. • A strong commitment to making technological investments, including a subsidized EHR, high performance claims system and patient registry. • Dedicated and exceptional support for you and your practice staff. • Health programs to support you such as case management, diabetes education, nutritional counseling and pharmacy consultations. • Fast, accurate claims payments. • Competitive reimbursement and meaningful performance bonuses. Learn more at www.HillPhysicians.com/JoinUs
From the President
A M E S S AG E F R O M D O N C R A N E , P R E S I D E N T A N D C EO
A M E R I C A’ S P H YS I C I A N G R O U P S
Members and friends,
When the ball dropped and we rang in the year 2020, few could imagine the world
as it is today. As I write this in late July, there are 16.5 million confirmed cases of the
novel coronavirus around the world, with 4.3 million cases here in the United States. Don Crane,
America’s Physician Groups
We’ve seen countries shut down their borders, states close virtually all businesses, President and CEO
and cities come to a complete standstill. The sickness and death, the economic
devastation, the stress—all brought about by COVID-19. Very few of us have ever experienced anything like this before.
Like many other organizations, America’s Physician Groups was not immune to COVID-19. Our highest priorities are the
health, safety, and well-being of the APG community. With that in mind, we made the very difficult decision to cancel
our Annual Conference 2020.
As the severity of COVID-19 became more evident, physicians rolled up their sleeves and got to work, putting their
own health at risk to meet the care needs of the patients and communities they serve. Many of our physician group
members—in a week or less—transformed their practices from virtually all in-patient visits to virtually all telehealth. Our
members are finding new and innovative ways to serve—from remote monitoring to virtual yoga. As one APG member
said, “We’re doing whatever it takes to keep our patients healthy.”
Your commitment to care hasn’t changed under these trying circumstances. And our commitment to providing you with
the leadership, advocacy, and educational resources you need remains as strong as ever. Here is what we are doing on
behalf of our members and others in the value-based care movement:
• We are hard at work in Washington, advocating to ensure physician organizations receive the resources they need
to keep their doors open and continue providing care to patients.
• Through our website, webinars, and other materials, we are educating our members on how to qualify for and
access vital resources in legislation like the CARES Act. We are providing information on changes to health
policies and regulations that matter to your practice.
• While we support our members’ fight against COVID-19, we also remain focused on driving the evolution and
transformation of healthcare delivery throughout the nation.
There is no question that millions of Americans are rightfully hurting and fearful of an uncertain future. I take solace
in a quote from Mahatma Gandhi: “The future depends on what we do in the present.” I couldn’t be prouder to be part
of an organization whose members are serving on the front lines of this healthcare crisis. Working together, we will
answer this global health threat. And we will come out
stronger for it.
As to the future, I hope you will join us for our Colloquium
2020, which will be held as a virtual event November 17-
19. The theme is a timely one: “Answering the Call: Value-
Based Care in Public Health.” For today, however, I hope
you stay safe and healthy.
As always, stay tuned and stay in touch. o
6 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020Mazars USA Can Help Your Organization with Proven Strategies for Operational Excellence Mazars USA’s Healthcare Consulting Group is proud to support APG’s vision of driving the evolution and transformation of healthcare delivery throughout the nation. Find out how Mazars can optimize your organization’s performance in the following areas: • CMS and State Audit Readiness Assessment, Preparation and Response • Compliance - including CMS, State and Accreditation • Comprehensive Program, Policy and Procedure Development • Enterprise Risk Management • Finance and Revenue Cycle • Fraud, Waste and Abuse • Managing New Licensing Requirements • Network Adequacy • Process Improvement • Public Policy Interpretation and Strategy • Quality and Utilization Management ...and much more. Gil Enos, Principal 916.565.6130 www.mazarsusa.com/hc
News and Events
WEBINARS NORTHWEST REGIONAL MEETING
August 19 Thursday, September 24
Emerging Insights of COVID-19 on Healthcare Delivery SAN DIEGO REGIONAL MEETING
August 20 Tuesday, September 29
Racism – A Public Health Crisis in America
PEDIATRICS COMMITTEE
August 27 Wednesday, September 30
Reimagining the Physician Role to Serve Seniors in the
Wake of a Crisis SOUTHEAST REGIONAL MEETING
(Offered by naviHealth) Tuesday, October 6
September 28 MIDWEST REGIONAL MEETING
Medical Group Pharmacy Trends and Drug Pipeline Tuesday, October 6
(Offered by Ventegra)
SOUTHWEST REGIONAL MEETING
PUBLIC RELATIONS/MARKETING COMMITTEE Tuesday, October 13
Tuesday, September 1
INLAND EMPIRE REGIONAL MEETING
GENERAL MEMBERSHIP/HUMAN Thursday, October 15
RESOURCES COMMITTEE
Wednesday, September 2 MOUNTAIN REGIONAL MEETING
Thursday, October 15
NORTHEAST REGIONAL MEETING
Tuesday, September 15 CONTRACTS COMMITTEE
Thursday, November 12
NORTHERN CALIFORNIA REGIONAL MEETING
Wednesday, September 16 For information on all APG events, visit www.apg.org. o
The Journal of Virtual Colloquium Edition 2020
“Value Based Care In Public
Health Emergencies”
Discounted Rates For
Members
For Information contact:
Valerie Okunami, Publisher
916-761-1853
journalofapg@gmail.com
8 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020VIRTUAL
EVENT
Nov. 17 - 19!
COLLOQUIUM 2020
November 17 - 19, 2020
ANSWERING THE CALL: VALUE-BASED CARE
IN PUBLIC HEALTH EMERGENCIES
For registration and information visit www.apg.org
Summer 2020 JOURNAL OF AMERICA’S PHYSICIAN GROUPS l 9Federal Policy Update
APG Advocates for COVID-19 Relief
BY G A R R E T T E B E R H A R D T, D I R EC TO R O F F E D E R A L A F FA I R S , A M E R I C A’ S P H YS I C I A N G R O U P S
The nationwide response to the COVID-19 pandemic continues. Congress and
the administration have passed a series of bills and regulations offering financial
relief and support for various industries impacted by COVID-19 and the resulting
halt to commerce across the country.
America’s Physician Groups has been extremely active in advocating on behalf
of our membership for financial relief and assistance during this pandemic. We
have also been very active in ensuring that alternative payment models, Medicare
Advantage (MA), and other risk-bearing arrangements are preserved during this
public health emergency—so that the move from volume to value-based care can
continue its momentum.
MSSP ADVOCACY
“Throughout
APG, along with eight other healthcare organizations, sent a letter to Seema
Verma, Administrator of the Centers for Medicare & Medicaid Services (CMS).
The letter provided recommendations in response to policy and regulatory
revisions related to the COVID-19 public health emergency. the COVID-19
The letter’s recommendations focused on ensuring that the Medicare Shared
Savings Program (MSSP) remains sustainable for accountable care organizations pandemic,
(ACOs) and physician groups that are on the front lines of COVID-19.
APG has been
“Every day, ACOs and physician groups are among the millions of healthcare
‘heroes’ providing care to the communities they serve,” wrote Don Crane, focused on
President and CEO of APG. “We urge CMS to provide them with the resources
they need to continue that care.” ensuring that
FUTURE OF APMS WEBINAR
physicians
Brad Smith, Deputy Administrator and Director for the Center for Medicare have a stable
and Medicaid Innovation (CMMI), joined APG’s recent webinar—co-hosted by
CareJourney—on the Future of APMs. Valinda Rutledge, Senior Vice President stream of
of Federal Affairs at APG, and Aneesh Chopra, President of CareJourney, gave
presentations on: financial
• What risk-based care will look like as the pandemic continues
assistance.”
• The future state of risk-based models in a post-COVID-19 world
• The value offered by staying in risk-based models during COVID-19
Deputy Administrator Smith reiterated his agency’s commitment to risk-based
models while speaking with attendees. He offered continued support and
collaboration from CMMI in pursuit of the models’ viability.
TELEHEALTH RECOMMENDATIONS
APG also met with CMS leadership to advocate that audio-only telehealth
services qualify for risk-adjustment payments. In April, CMS announced
10 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020that organizations—including those in Medicare Considering the increased importance of telehealth, the
Advantage (MA)—that submit diagnoses for risk- letter addressed to Senate Finance made the case for
adjusted payment can now submit diagnoses from making these changes permanent.
telehealth visits for risk adjustment. However, CMS
insisted that payment eligibility only extended to APG also submitted letters to Sens. Jeanne Shaheen
audio-video visits. (D-N.H.) and Michael Bennet (D-Colo.), as well as five
additional Senate offices, in support of their recently
APG sent a letter advocating for extending eligibility introduced Medicare Accelerated and Advance
for MA risk-adjustment payment to audio-only Payments Improvement Act. This legislation provides
telehealth services during COVID-19. The letter physician groups on the front lines of COVID-19 with the
recommended that CMS count diagnoses obtained financial resources they need to continue providing care
from audio-only telehealth services for MA risk to the communities they serve. Key components include:
adjustment and offered suggestions on the guardrails • Authorizing CMS to offer partial forgiveness for
given by CMS—analyzing the obstacles they present the loans provided by the accelerated and advance
for physicians in providing care. payment programs
The letter also highlighted discrepancies in payment • Lowering the amount withheld from Medicare
for audio-only telehealth visits compared with audio- service claims from 100% to a much more
visual visits. APG continues to advocate on this issue manageable 25%
and the extension of adequate payment for audio- • Lowering the applicable interest rate of repayment
only telehealth services. to 2%
COMMENTS: INTERIM FINAL RULE IN CONCLUSION
APG filed comments to CMS on the agency’s Throughout the COVID-19 pandemic, APG has been
April interim final rule. The rule offered regulations focused on ensuring that physicians have a stable
addressing a variety of issues resulting from the stream of financial assistance—while also advocating
COVID-19 pandemic. APG outlined a host of that Congress, the U.S. Department of Health & Human
recommendations in response to the rule, including: Services, CMS, and other federal agencies work to
• Expansion of eligible providers for alleviate near-term financial concerns so that physicians
reimbursement for telehealth may concentrate on providing care.
• Reimbursement for physicians for audio-only APG is committed to transforming our healthcare system
telehealth services for MA risk adjustment toward one focused on value-based care and improved
• Lifting restrictions on e-health and virtual check- population health, quality, and patient experience. APG
ins that require providers to track possible follow- will advocate for additional financial relief as debate in
up visits and reconcile any follow-up interactions Washington continues. o
• Clarity on the types of services that may be
available to patients on homebound status
during the public health emergency
• Incentives to keep healthcare organizations
enrolled in alternative payment models
• Pay-for-reporting for all quality measures in
2020 and 2021
ON CAPITOL HILL
We have also remained active in our advocacy on
Capitol Hill. We sent letters to the Senate Committee
on Finance and the Senate Committee on Health,
Education, Labor and Pensions (HELP). The letters
stressed the importance of telehealth and advocated
for continuing flexibilities for these visits past the
current public health emergency.
Summer 2020 JOURNAL OF AMERICA’S PHYSICIAN GROUPS l 11Policy Briefing
MHA Grad Implements Telehealth During COVID-19
BY B I L L B A R C E L LO N A , E X EC U T I V E V P, G OV E R N M E N T A F FA I R S , A M E R I C A’ S P H YS I C I A N G R O U P S
In March 2020, as the COVID-19 pandemic hit California, Yamilett Medrano
jumped into the deep end of the pool.
“Yami” Medrano graduated from the University of Southern California’s Master
of Health Administration Program in 2017. She then began working for Loma
Linda University Health—first as Telehealth Program Manager and then as
Program Director for Digital Health. Her job: implement and develop telehealth
adoption among Loma Linda physician networks throughout Southern
California’s “Inland Empire.” Loma Linda is a big system, with a network of over
1,000 providers.
The job was going slowly and steadily with the usual issues—health plan
reluctance to incent telehealth adoption and physician confusion over dozens
of conflicting standards and billing processes. During the first part of 2020,
“Loma Linda’s though, newly enacted California legislation was accelerating telehealth
adoption. This was in anticipation of a January 1, 2021, mandate for health
insurers to cover telehealth services and pay providers in parity with in-person
earlier visits. But the challenging environment was still impeding adoption.
preparations The COVID-19 pandemic changed everything.
provided a AN OVERNIGHT CHANGE
foundation for The Inland Empire, like the rest of the country, suddenly experienced an
overnight drop in patient visits. Physicians scrambled to keep their offices
rapid adoption open, scrounging for personal protective equipment (PPE). Public officials
cautioned people to avoid elective healthcare, and patients stayed home. Loma
across its Linda University Health, like other systems across the nation, had to implement
telehealth capabilities almost overnight.
provider Since Medrano was the only full-time employee in the Digital Health
network.” department, she was tasked with developing expertise and partnering
with leaders across the organization to prepare the standards, billing, and
technology aspects for implementation.
Prior to the pandemic, the system was averaging five to 10 video visits per day.
In a matter of 72 hours, the number of video visits was increased to include all
physician-based and hospital-based clinics. By March 17, all clinics had been
instructed to convert visits to telephone or video.
At the late April peak, the network was averaging 53% of overall outpatient
visits completed via video, about 21% via telephone, and another 26% in
person. E-visits increased volume, but only reached about 1% of overall visits.
Primary care areas (i.e., family medicine, general medicine, and pediatrics)
achieved as high as 90% to 95% of total visits completed virtually. These
encompassed video, telephone, and e-visits.
12 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020Since the pandemic began, 651 providers have seen Patients like the experience as well. Medrano reports
patients via video, and 127 clinic locations have offered that surveys indicate that patients appreciate the
video visits. This does not include additional hospital and convenience and feel as if they have more time to ask
skilled nursing facility (SNF) video visits. questions and speak with their physician.
Will telehealth stick? By early May, the network began
A FOUNDATION FOR SUCCESS to add back more in-person visits and procedures/
Like other integrated systems that had embarked on surgeries into its utilization volume. Loma Linda
adopting telehealth prior to COVID-19, Loma Linda’s University Health is still averaging 30%-50% of
earlier preparations provided a foundation for rapid its patient visit volume (it varies across specialties)
adoption across its provider network. through telehealth video visits. Medrano estimates that
the network will reach a level of 20% to 30% virtual
The previous integration of the electronic health record patient visits over the long term. Both patients and
(EHR) solution, Epic, included MyChart video visits and physicians have learned to appreciate the convenience
provided a stable platform for provider adoption that and access provided by telehealth.
was connected to the existing patient record system.
Loma Linda had also contracted with Vidyo to provide Was the effort worth it? Definitely, says Medrano.
secure, accessible telehealth access to patients across The quick effort to deploy telehealth solutions
the internet. across the entire network was a professionally
rewarding experience, bringing a profound sense of
After the Centers for Medicare & Medicaid Services accomplishment. An early advocate for telehealth, she
(CMS) issued a HIPAA waiver, Zoom was also also participates in the California Telehealth Policy
introduced into clinical workflows. Zoom soon Coalition—a stakeholder group that circulates best
accounted for 20% of all video visits. The other 80% practice resources and advocates for greater adoption
were completed using MyChart or other physician- of this form of care delivery. The future will bring
preferred video options. Medrano attributes the rapid greater understanding of the areas in which video
deployment to the availability of the EHR-integrated visits can be offered, and where they cannot. o
video platform and the huge team effort that helped
Loma Linda respond and transition care successfully. Postscript: Medrano’s time at USC included courses
taught by Bill Barcellona, an adjunct professor at USC.
In a matter of days and weeks, Loma Linda also had He is very proud of Medrano’s work ethic, commitment,
to create patient-facing education—including flyers, and skills, and he looks forward to her future
FAQs, tips and tricks, and a dedicated webpage. Its accomplisments.
marketing team rushed to place billboards throughout
the community advertising virtual care. “We continue to
revise and strategize how we educate and communicate
with patients, physicians, and staff,” she says.
The time crunch was just the first hurdle. Loma Linda
University Health was also challenged with connectivity
issues and network infrastructure problems. Audio
difficulties arose from time to time. Medrano identified
a need for a secondary, non-integrated video solution
such as Zoom or Doximity for patients who did not have
a patient portal or did not want to join via MyChart.
WILL TELEHEALTH STICK?
How did the doctors and patients feel about this
transition? A surprising number of physicians that had
previously been resistant to telehealth realized that
the video visit format was comfortable for both them
and their patients. Physicians can learn a lot about a
patient’s environment and background through video
visits.
Summer 2020 JOURNAL OF AMERICA’S PHYSICIAN GROUPS l 13ON THE COVER
APG Member Spotlight
Pivoting to Telehealth—Overnight
BY B I L L W U L F, M D
Prior to March of this year, Central Ohio Primary Care (COPC) did not provide
telehealth visits. In preparation for a slow launch of video visits in 2020, we
increased our broadband capabilities in early 2020. Fortuitously, an upgrade from
eClinicalWorks (eCW) in January improved our ability to deliver a satisfactory video
visit.
The plan was to pilot telehealth mid-year with a slow launch in the third quarter.
Then, COVID-19 came along.
IT AND TELEHEALTH RESPONSE
In response to the emerging pandemic—and in accordance with directives from the
state of Ohio’s Department of Health—we asked our physicians to limit in-person
visits to emergencies or those deemed clinically necessary. We instructed our
physicians that no wellness exams be performed in person, for patients of any age,
beginning March 23. “The plan was to
In just one week, starting March 17, the COPC Information Services Department
enabled 380 providers to perform video visits. In the six weeks between March 23
pilot telehealth
and May 8, our staff web-enabled over 16,000 patients who had not previously been mid-year with a
accessing our portal, thus enabling an upcoming video visit for these individuals. Our
physicians used eCW, Updox, and (rarely) FaceTime technology for video visits. slow launch in
Patient volumes were maintained at a 65% level compared with 2019, and 65% of
all visits were done by video during the six weeks following March 23. COPC care
the third quarter.
management staff reached out to nearly 4,000 high-risk patients to meet both
social and medical needs. These patients were identified based on age, chronic
Then, COVID-19
conditions, past emergency room utilization, and on whether they lived alone. came along.”
If needed, care management staff went to the patient’s home with an iPad to
facilitate a video visit with a physician. During this time, an after-hours video visit
system enabled over 500 video visits during evenings and weekends. Our triage
system found that nearly half of these patients required a visit within four hours, and
all were done via video.
These visits were “picked-up” by waiting physicians within one minute of being
placed in a queue by an after-hours call center nurse. As of June 18, COPC had
completed over 90,000 video visits this year. Despite now seeing patients in person,
we continue to use video for more than 20% of our over 3,500 daily visits.
SURVEYS SAY…TELEHEALTH IS HERE TO STAY
We surveyed over 8,000 patients following their video visit, as well as our primary
care physicians. We found that:
• 98% of patients were either satisfied or highly satisfied with their video visit.
• Only 36% of patients said they would prefer their next visit be in-person.
14 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020• 90% of physicians planned to continue telehealth as and even encouraged others to care for our patients
part of their practice. outside of the limited hours we set for our clinics.
• 97% of physicians were either confident or Fortunately, the nationwide expansion of value-based
extremely confident in their ability to provide contracting and the progressive movement to full-risk
telehealth. contracting will accelerate the recognition that we as
Continued telehealth services will require adequate primary care physicians will be expected to assume
reimbursement from commercial and government payers, an expanded responsibility for our patients’ care. o
as well as employer support. A video visit performed by Bill Wulf, MD, is CEO of Central Ohio Primary Care
a patient’s PCP within the health record is clearly the (COPC) and Chair-Elect of America’s Physician
most desirable and clinically efficient telehealth service Groups.
available. There are surely many visits that can and
should be provided via video.
Central Ohio Primary Care (COPC) is an
LOOKING BACK independent, physician-owned primary care
It is a shame that it took a pandemic to move us to organization with 435 physicians in 77
telehealth. In retrospect, I believe we as primary care locations. Ancillary services include a high-
physicians began abdicating some of our responsibility complexity laboratory, radiology, cardiovascular
years ago—when we turned our phones to an answering testing, and six urgent care facilities. COPC
service at 5 p.m. each weekday and on weekends. utilizes eClinicalWorks and cares for 25% of the
population in Central Ohio.
Our recorded message would first instruct patients to
hang up and call 911 or go to the emergency room if All COPC commercial contracts include a per-
there was an emergency. Next we provided a long list of member, per-month prepayment used for care
services we could not, or would not, provide after hours. management and education programs, as well
Finally, we asked the patient to leave a message and as year-end shared savings. COPC is a CPC+
returned the call sometime later. participant for 35,000 Medicare fee-for-service
lives and is in a joint venture with agilon health
This abdication led to the need for urgent care facilities, in prepaid, full-risk arrangements for 33,000
overuse of emergency departments, and the advent Medicare Advantage lives.
of remote telehealth services provided outside of the
patient’s longitudinal record. We have often allowed
Summer 2020 JOURNAL OF AMERICA’S PHYSICIAN GROUPS l 15Payer-Provider Partnerships in a Post-
Pandemic World
BY DAW N M A R O N E Y
The realities of the COVID-19 pandemic reveal an urgent need for healthcare
providers and payers to work together for the benefit of both patients and
frontline physicians. Infected patients require fast, unfettered access to testing
and treatment. Overwhelmed physicians and their staff must clear the way to
treat urgent patients, while upholding care for their patients struggling with
chronic illnesses and ongoing treatment needs.
As global attention naturally turns toward the crisis at hand, it is important that
stakeholders across the healthcare industry do not lose sight of the role that
payer-provider partnerships will play not only today, but moving forward. The
good news is our industry was moving in this direction even before COVID-19.
In a 2019 SPH Analytics survey of more than 80 providers and health plans,
94% of respondents said they believe collaboration between payers and
“Partnerships providers is now a key determinant of success.1 Partnerships within the
healthcare ecosystem we’re building today will become the foundation for
more sustainable business models that put patients at the center of care,
within the offer efficiency to overburdened healthcare teams, and work toward reducing
unnecessary spending—all ingredients for effective healthcare resilience in the
healthcare future.
ecosystem we’re Last year, Alignment Healthcare formed partnerships with two of California’s
largest regional systems: Sutter Health, based in Sacramento, and PIH Health in
building today Whittier. As the benefits of our partnerships have become more obvious during
the pandemic, we have learned that these relationships work best when our
will become the goals are aligned and our partnerships meet the needs of every patient in the
foundation for ecosystem. While many factors contribute to a successful partnership, we have
discovered that three overarching tenets are critical.
more sustainable
TENET 1: SIMPLIFY PATIENT ACCESS TO CARE
business models As community hospitals across the country quickly pivoted to address faster
that put patients testing and urgent care for coronavirus cases, we saw a concerted effort
to reschedule routine physician visits and non-urgent or voluntary medical
at the center of procedures. It made sense, too: Hospitals were right to preserve capacity for
incoming COVID-19 patients.
care.”
Necessity becomes the mother of faster adoption. While staying home has been
the recommended strategy for flattening the curve and avoiding infection, we
cannot ignore the importance of general healthcare and the ongoing monitoring
and treatment for chronic illnesses. In response, we’ve seen a dramatic spike
in the adoption of telehealth solutions. This year, the U.S. telehealth market is
expected to reach around $10 billion, with 80% year-over-year growth due to
the COVID-19 pandemic, according to an Arizton report.2 And for good reason.
As TechRepublic recently reported, “Online appointments give doctors greater
16 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020flexibility, and with flexibility being one of the key interests, allowing payers to more easily lower the cost
factors in preventing burnout, that perk is incredibly trajectory of healthcare costs and offering providers the
beneficial for the provider’s state of mind.” 3 tools to help effectively deliver quality care.” 4
A foundation for our partnerships with Sutter and Tightly aligned incentives for patients, providers,
PIH is Alignment Healthcare’s ACCESS On-Demand and payers are a key foundation for our provider
Concierge program. This service empowers Alignment partnerships. First and foremost, patients must have
Health Plan members to access a national network the best possible outcomes—or they will take their
of U.S. board-certified physicians by phone or video business elsewhere. Meanwhile, providers need
24 hours a day, seven days a week. This makes it accurate, complete interoperable patient data and help
easy for our members to honor shelter-in-place orders with ongoing consumer engagement. Payers need the
without delaying a diagnosis, treatment, or changes in highest-quality care for their members, with an eye
prescriptions. It also allows doctors to focus first and toward staying efficient with resources and cutting out
foremost on their highest-priority patients. waste.
In just one example, as the payer in California, we
TENET 2: PROVIDE FLEXIBLE SUPPORT FOR implemented a proactive educational communications
STRESSED PHYSICIANS AND THEIR TEAMS campaign that engaged nearly 100% of our members
Before COVID-19, physicians already balanced through email, SMS text, phone calls, telephonic town
limited time with increasing patient loads. As this new halls, and direct mail, advising them on how to protect
pandemic schedule intensifies, digital solutions that themselves from COVID-19 and stay at home. We
automate manual tasks, provide a more comprehensive believe this aggressive member engagement effort
picture of patient health, and allow physicians to invest contributed to lives saved.
more time in critical cases will become invaluable.
While the pandemic and all of its social, economic, and
A foundation for Alignment’s provider partnerships is health impacts have yet to play out, the payer-provider
AVA™, our proprietary data analytics and technology partnerships we are codifying now will be part of the
command center. AVA hosts our Alignment Healthcare future of driving value across the healthcare chain for
Patient 360, which gives physicians a snapshot of a the patient, the doctor, and the greater good—no matter
member’s health and treatment history so they can what comes next. o
facilitate care coordination and close gaps in care. It
keeps providers engaged with their patients’ care even Dawn Maroney is President for Alignment Healthcare,
if they cannot see them physically. It also simplifies a Medicare Advantage company focused on providing
access to additional care that may be needed. population health management services to health
systems and provider groups across the country.
Alignment Healthcare has also worked to supplement
physicians’ telehealth backlog—now a growing reality— References
with Alignment’s network of doctors. We do this via our 1
Amick, Amy. “Why Payer-Provider Partnerships Need More
Care Anywhere program, a targeted high-risk program Collaboration.” Physicians Practice. October 2, 2019. https://www.
focused on the delivery of in-home care. Our clinical physicianspractice.com/view/why-payer-provider-partnerships-need-
more-collaboration
team, in coordination with a member’s primary care
physician, provides members 24/7 access to a doctor 2
Arizton Advisory and Intelligence. “Telehealth Market in US – Industry
and data-driven in-home care solutions. Outlook and Forecast 2020-2025.” April 15, 2020. https://www.
prnewswire.com/news-releases/the-telehealth-market-in-us-to-reach-
revenues-of-over-25-billion-during-the-period-2020-2025---market-
TENET 3: ALIGN INCENTIVES TOWARD A research-by-arizton-301040962.html
MORE SUSTAINABLE BUSINESS MODEL THAT 3
Bayern, Macy. “Telemedicine Soars Amid COVID-19. Will Virtual
CENTERS THE ECOSYSTEM AROUND BETTER Healthcare Be the New Normal?” TechRepublic. May 19, 2020.
PATIENT OUTCOMES https://www.techrepublic.com/article/telemedicine-soars-amid-covid-
19-will-virtual-healthcare-be-the-new-normal/
Unfortunately, the traditional healthcare landscape
often puts payers and providers at odds around
4
Deloitte. “Aligning Health Plans and Providers: Working Together
to Control Costs.” 2017. https://www2.deloitte.com/content/dam/
misaligned incentives in the patient interaction. Deloitte/us/Documents/life-sciences-health-care/us-lshc-deloitte-
According to a 2017 Deloitte report, “Value-based care aligning-health-plans-and-providers-v1.pdf
encourages providers and health plans to align their
Summer 2020 JOURNAL OF AMERICA’S PHYSICIAN GROUPS l 17How Will COVID-19 Impact Business
Insurance Premiums?
BY B R A D AY R E S
Given the climate of great uncertainty created by the COVID-19 pandemic, how
will business insurance premiums be affected? To help answer this question for
the America’s Physician Groups member community, I will share some of the
recent trends influencing insurance rates and provide guidance on what can be
expected with premiums in your upcoming renewals. (And please, don’t shoot
the messenger—I come in peace.)
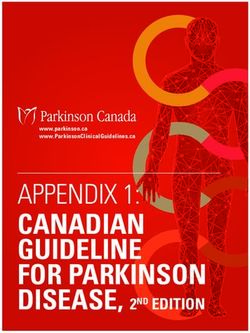
FACTORS IMPACTING RATES
Insurance rates are primarily driven by empirical data but are influenced by
risk-projection models. Risk is inextricably tied to uncertainty. In this unique
time of global health, social, and financial uncertainty, insurance premiums are
increasing, coverage is tightening, and deductible levels are rising for several
“Insurance
lines of insurance.
Insurance underwriters are guided by actuaries. These actuaries are supported
by teams of financial and business analysts that use technology to evaluate and
determine a given organization’s risk. They take into account one to three years premiums are
of historic empirical “experience” data, exposure across coverage categories,
and the firm’s financial strength, coupled with industry guidance. increasing,
coverage is
AREAS OF ANTICIPATED PREMIUM INCREASES
We are seeing the greatest rate increases in employment practices liability
tightening, and
(EPL), followed by directors and officers (D&O) and errors and omissions (E&O)
insurance. Other lines—including cyber and crime, as well as property and
deductible levels
casualty (P&C)—are showing lower unilateral increases in comparison. Stop are rising.”
loss and employee benefits insurance rates appear to be less directly impacted
by the pandemic at this point.
CONTRIBUTING FACTORS
Layoffs and Furloughs:
Since the economic impacts of the pandemic hit our industry late in the first
quarter, carriers have seen wrongful termination claims spike. This is due to the
widespread furloughs and layoffs many healthcare delivery organizations have
had to make. The carriers must account for this increase in wrongful termination
claims in their risk models, and it is now reflected in higher premiums for EPL
and E&O insurance.
Working From Home:
Although deemed “essential,” most health delivery organizations have pivoted
to having their employees work primarily from home. This dramatic change has
introduced new risks.
18 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020I don’t believe any
healthcare executive COVID-Related Impact on Premiums for
would have predicted
in January that his or
Risk-Bearing Organizations
her entire team would Q3-20 Through Q1-21 Renewals
operate remotely
from their homes— Anticipated
Coverage Change
let alone complete Insurance Premium Reason
Trends
such a transition in Impact
Employment Practices Liability 10% to 50% Extensive HR-related policy Layoffs, furloughs, and
under a few weeks. (EPL) increase updates, signed waiver workforce changes leading to
The technologies requirements, RTW policies more wrongful termination
that were rapidly followed exposure
deployed, the remote Directors and Officers (D&O) 10% to 30% Carrier withdrawals, Fiscal responsibilities, insured’s
increase restrictions in coverage,accuracy in modeling, proper
management and
additional underwriting transparency, oversight of
accountability scrutiny operations
processes Professional Liability/Medical 5% to 10% Policy limits on liability
COVID-related employee suits,
established in such Malpractice increase decreased infection-related litigation
short order, were increased, workplace safety
costs and issues
impressive. It’s been
HMO Reinsurance (Provider 5% to 20% Decreased pharmacy Pharmacy costs driving majority
a remarkable feat to Stop Loss) increase coverage limits, increased of costs. Expensive gene therapy
witness the robust member exclusions drugs entering market.
changes, particularly Errors and Omissions (E&O) 5% to 10% Conservative underwriting, Business risk measurement
in claims operations, increase limit constriction unsettled, operational change
resulting from economic forces
where teams
Cyber Liability, Cyber Crime, 5% to 20% Additional documentation of Cyber attacks up 25% to 40%
traditionally worked Privacy & Network Security, increase the distributed network since pandemic. Remote
in office settings. Network Business Interruption security system and policies employees using more
(Cyber) in place vulnerable systems.
But the speed of Business Property & Casualty Minimal change No direct COVID-19 correlation
this change has also noted.
created cyber-crime
risks not anticipated
before the pandemic. Healthcare operations are now pandemic, attackers are taking advantage of the fact
being run from a widely distributed work environment that many employees have been working from home,
of home settings, rather than being managed within the without the technical protections that their corporate
heavily fortified corporate infrastructure. New security networks often provide.”1
vulnerabilities include:
Return to Work:
• Personal equipment being used for professional
When things stabilize, a robust “return to work” strategy
use
will be important to protect the health of your employees
• Multi-factor authentication (MFA) often not utilized and your business from avoidable workers’ compensation
using shared home computers claims. Litigation driven by employees feeling unsafe to
• Company VPNs established on compromised return to work due to the threat of workplace COVID-19
personal equipment infections is contributing to premium increases.
This presents criminals with opportunities, and Recommendations from leading health agencies
the attacks are growing in sophistication and zeal. are advising employers to become workplace health
Ransomware and phishing schemes increase during gatekeepers to ensure office safety.2 While this seems
high-anxiety periods as more people fall prey to fear like a necessary step given the crisis we face, such
and hope-based campaigns. practices threaten to infringe on longstanding personal
health privacy rights in the name of new models of
A recent Beazley report showed a 25% increase workplace safety procedures. Your insurance broker
in ransomware attacks in the first quarter this year
over the prior quarter. The report states, “During the continued on next page
Summer 2020 JOURNAL OF AMERICA’S PHYSICIAN GROUPS l 19continued from page 19 WHAT YOU CAN DO
should have resources to support your human When possible, ensure your broker incorporates an
resources department with carrier-recommended tools “experience refund” to your premiums. This provision will
to help you balance this fragile dilemma. benefit you if the insurer’s loss experience is less than
projected. Build in more time during your renewal to
Expect insurance premium increases with D&O, E&O, account for the additional supporting documentation that
and EPL as we travel down uncharted paths littered carriers are now requesting.
with HR land mines this year.
Make sure you are receiving multiple carrier bids. The
Medical Spend Projected Increases: rate variation from carrier to carrier can be 15% to
The financial effects of the COVID-19-related critical 50% for certain coverage lines. The rate disparity is
care cases ripple through the entire healthcare heightened during times of great uncertainty. If you
ecosystem. There’s also concern about an increase have not received multiple carrier bids in the past, you
in hospitalizations coinciding with the flu season this may have paid hundreds of thousands of dollars more
fall. With such widespread speculation of the financial on insurance than necessary. Multiple bids are more
impact on both public and private entities, underwriters important than ever.
are more risk-averse. This is reflected in increased
rates, higher deductibles, lower caps, and more carve- SILVER LININGS
outs written into the policies.
The COVID-19 pandemic is a global tragedy of
We’ve also seen stop-loss insurance carriers incalculable measure. Amidst the great loss, the crisis
increasingly engage with clients to develop specific has sharpened us and inspired heroic healthcare
risk mitigation strategies to help prepare and manage leadership and innovation. I believe the courageous
the rise of high-cost exposure. The shared incentive decisions made in streamlining workflows, empowering
to manage costs is driving many carriers to extend individuals, trusting remote employees, widely
analytic tools and clinical resources to clients. incorporating telehealth technologies, and proactively
engaging patients will lead to permanent changes. Some
Shift From Commercial to Medicaid: of these remarkable innovations were highlighted by New
Millions of former commercially insured members are West Physicians and Vancouver Clinic in a recent APG
now on Medicaid. This is due to the highest volume webinar.4
of initial filing for unemployment assistance since
I am hopeful these efforts and breakthroughs will lead
the Great Depression. For physicians, this shift has
to lower insurance premiums the following policy year as
meant reductions in contract rates and fee-for-service
you demonstrate improved outcomes even in a time of
reimbursements.3
crisis. In the meantime, the broker community is here to
When significant decreases in physician compensation advocate for you and help ensure you have the necessary
transpire, an increase in claims fraud traditionally insurance protection to weather the storms ahead. o
follows. Investing in a leading claims fraud/waste/
Brad Ayres is the Senior Healthcare Advisor for Pinnacle
abuse solution to protect your business will not only
Brokers, an APG Group Purchasing (GPO) partner.
protect you during this anticipated trend, but help
control stop-loss premium increases in the years References
ahead.
1
Beazley Breach Insights, June 2020. Retrieved July 5, 2020, from
https://www.beazley.com/news/2020/beazley _breach_insights_
ADDITIONAL RENEWAL DOCUMENTATION june_2020.html
2
Centers for Disease Control and Prevention, May 21, 2020. Retrieved
You can expect more stringent financial reporting July 6, 2020, from https://www.cdc.gov/coronavirus/2019-ncov/
and reserve requirements. Carriers are requiring community/resuming-business-toolkit.html#employer-sheet
additional financial documentation and tightening 3
Milliman, April 29, 2020. Estimating the impact of COVID-19
financial solvency standards. They are also looking for on healthcare costs in 2020. Retrieved April 29, 2020,
compliance adherence language pertaining to return- from Milliman: https://milliman-cdn.azureedge.net/-/
media/milliman/pdfs/articles/covid-impact-webinar-slides.
to-work procedures and office health safety (OSHA) ashx?la=en&hash=9D48FDF7A8D0D4808E8E23961A796B13
protocols. These updated protocols for each state are 4
America’s Physician Groups. (2020, April 17). APG. Retrieved July
available at osha.gov/stateplans/. 5, 2020, from https://www.apg.org/wp-content/uploads/2020/04/
COVID-19-Case-Studies-in-Excellence.pdf
20 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020ORGANIZATIONAL MEMBERS Physicians Group • Hattiesburg IPA • Jest IPA Dignity Health Medical Foundation: Dignity
• KMG • Liberty Independent Physicians Group Health Medical Group Arizona • Dignity Health
ACO Management Services, LLC • Lighthouse IPA • Little River Canyon IPA • Medical Group Nevada • Dignity Health Medical
Kamal Jemmoua, CEO Memphis Mid Town IPA • North Tennessee Network - Santa Cruz • Foundation Physicians
Mallory Cary, Regional Director ACO Operations Medical Network • Prestige Physicians Group Medical Group • Identity Medical Group • Mercy
IPA • Princeton Premier IPA • Providence Medical Imaging Medical Group • Mercy Medical Group •
Advanced Medical Management, Inc. *
Network IPA • Red Mountain IPA • Renaissance Woodland Clinic Medical Group
Kathy Hegstrom, President
Physicians Organization • River Region IPA
Hank Lee, Executive Vice President Commonwealth ACO
• Rutherford County Physicians Network •
Groups: MediChoice IPA • Northern California SCIPA • Southern Medical Physicians IPA • St. Petar Novakovic, MD
Physician Network • Seoul Medical Group • Thomas Med Partners, LLC • Summit West IPA • Lance Donkerbrook, CEO
M E M B E R S
Torrance Health IPA Synergy HealthCare • Synergy IPA • Tallaco IPA Conifer Health Solutions
• Tennessee Valley IPA • Trendsetter Physicians Mary Bacaj, Head of Value-Based Care
Adventist Health Physicians Network IPA IPA • TriStar Medical Network • Valley Forge IPA
Erica Fraguero, Director of Finance, SCR • Valley Organized Physicians • Walker IPA • West Groups: Exceptional Care Medical Group • Family
Arby Nahapetian, MD, CMO Alabama IPA Choice Medical Group • Family Health Alliance
• Mid Cities IPA • Omnicare Medical Group •
Aegis Medical Group Cedars-Sinai Medical Group * Premier Care of Northern California • Saint
Carl Patten, General Counsel Caroline Goldzweig, MD, Chief Medical Officer Agnes Medical Group
Affinity Medical Group John Jenrette, MD, Executive VP, Medical Network
Cornerstone Health Enablement Strategic
Richard Sankary, MD, President Central Ohio Primary Care Physicians Inc. * Solutions (CHESS)
Melissa Christian, Interim VP of ACO Operations J. William Wulf, MD, CEO Yates Lennon, MD, Chief Transformation Officer
Agilon Health Larry Blosser, MD, Corporate Medical Director Dan Roberts, Chief Operations Officer
Ben Kornitzer, MD, Chief Medical Officer Central Oregon Independent Practice Desert Valley Medical Group, Inc.
Steven Sell, Chief Executive Officer Association Imran Siddiqui, MD, Medical Director
AllCare IPA Divya Sharma, MD, Medical Director Marie Langley, IPA Administrator
Matt Coury, CEO Kim Bangerter, Executive Director
DFW HealthCare Partners LLC
Randy Winter, MD, President ChenMed * Osehotue Okojie, MD, IPA Chairman
Allied Physicians of California Guarov Dayal, MD, President, New Markets and Josh Cook, President
Thomas Lam, MD, CEO Chief Growth Officer
Stephen Greene, Chief of Staff DuPage Medical Group
Kenneth Sim, MD, CFO Paul Merrick, MD, President, Co-CEO
AltaMed Health Services Corporation Children First Medical Group Mike Pacetti, CFO, Co-CEO
Castulo de la Rocha, JD, President and CEO James Florey, MD, Chief Medical Officer
James Slaggert, Chief Executive Officer East Coast Medical Services, Inc.
AppleCare Medical Group, Inc. Ismary Gonzalez, MD, President
Trish Baesemann, President Children’s Physicians Medical Group
Leonard Kornreich, MD, President and Chief Edinger Medical Group
George Christides, MD, Chief Medical Officer Stan Arnold, MD, Senior Physician Executive
Executive Officer
Arizona Health Advantage, Inc. Denise McCourt, COO
Tanya Sibrava, DO, Senior Medical Director Chinese American IPA
Peggy Sheng, Chief Operating Officer El Paso Integral Care, IPA
Terry Smith, Chief Operating Officer Hector Lopez, DO, Chairman of the Board
George Liu, MD, President & CEO
Austin Regional Clinic * Tony Martinez, Administrator
Norman Chenven, MD, Founding CEO Chinese Community Health Care Association
Cathy Chan, Director of Operations EPIC Management, LP
Anas Daghestani, MD, Chief Operating Officer Raymond Chan, MD, VPMA & CMO
Bayhealth Physician Alliance, LLC CHOC Physicians Network John Goodman, President & CEO
Evan W. Polansky, JD, Executive Director Michael Weiss, MD, VP Population Health
Groups: Beaver Medical Group, L.P. • Pinnacle
Joseph M. Parise, DO, Medical Director Choice Medical Group Medical Group • Tri-Valley Medical Group
Beaver Medical Group * Manmohan Nayyar, MD, President
Thomas Conjurski, MBA, MSO/IPA Administrator Equality Health – Q Point
John Goodman, President and CEO Pedro Rodriguez, HMA Board Member
Raymond Chan, MD, VP Medical Admin/CMO of CHS Physician Partners IPA, LLC Mark Hillard, President
Epic Health Plan Patrick M. O’Shaughnessy, DO, EVP & Chief
Clinical Officer Facey Medical Foundation *
Bright Health Inc. Erik Davydov, MD, Medical Director
Martin Serota, MD, Chief Medical Officer Jonathan Goldstein, MBA, Executive Director
David Mast, Chief Executive, Medical Group
A P G
Rachel Winokur, Chief Exeuctive Officer Cigna Medical Group Foundations
Brown & Toland Physicians * Kevin Ellis, DO, CMO
Good Samaritan Medical Practice
Kelly Robison, CEO Citrus Valley Independent Physicians Association
Joel Klompus, MD, President & Interim CMO Gurjeet Kalkat, MD, Executive Medical Director Nupar Kumar, MD, Medical Director
California Pacific Physicians Medical Group, Martin Kleinbart, DPM, Chief Strategy Officer
Greater Newport Physicians Medical
Inc. Collaborative Health Systems, LLC Group, Inc. *
Dien V. Pham, MD, CEO Anthony J. Valdes, President Adam Solomon, MD, CMO
Carol Houchins, Administrator Deeling Teng, MD, Senior Medical Director
Colorado Permanente Medical Group, P.C.
Canopy Health Margaret Ferguson, MD, President & Executive Hatfield Medical Group
Mike Robinson, CEO Medical Director David Hatfield, MD, Chief Medical Officer
Margaret Durbin, MD, CMO Claire Tamo, CFO and VP, Business Operations Maria Barnett, Director of External Affairs
CareAllies CommonSpirit Health * Hawaii IPA
Joe Nicholson, DO, Chief Medical Officer Gary Greensweig, DO, SVP Physician Enterprise, Greigh Hirata, MD, President
Casey McKeon Chief Physician Executive Julie Warech, Administrative & Financial
Groups: Accountable Care Coalition of Alabama Bruce Swartz, EVP Physician Enterprise Manager
• Baldwin Physicians Network • Ben Franklin Groups: Catholic Health Initiatives: Architrave Hawaii Pacific Health
Physicians IPA • Broad Spectrum IPA • Clarksville Health • Arkansas Health Network • CHI Kenneth B. Robbins, MD, CMO
Medical Network • Cullman Primary Care • Dallas Franciscan Health • CHI St. Joseph Health • Maureen Flannery, VP, Clinic Operations
IPA • DC Qual-Care IPA • Delco Wellness IPA • Colorado Health Neighborhoods • KentuckyOne
DFW Healthcare Partners IPA • East Memphis Health Partners • Mercy Health Network • Mission Hawaii Permanente Medical Group, Inc.
Medical Network • El Paso Integral Care • Elite HealthCare Network • PrimeCare Select • St. Geoffrey Sewell, MD, Executive Medical Director
Medical IPA • Emerald Shores IPA • Etowah IPA Luke’s Health Network • TriHealth • UniNet Daryl Kurozawa, MD, Associate Medical Director
• Franklin Medical Network • Greater Chicago
Summer 2020 JOURNAL OF AMERICA’S PHYSICIAN GROUPS l 21Heritage Provider Network * • Integrated Health Partners • Pioneer Provider Optum (Formerly HealthCare Partners) *
Richard Merkin, MD, President Network • Premier Physicians Network • Prospect Amar Desai, MD, President Coastal Region
Richard Lipeles, COO Medical Group-LA Care • Prudent Medical Group Don Rebhun, MD, Regional Medical Director
• Redwood Community Health Coalition • Watts
Groups: Affiliated Doctors of Orange County • Arizona Health Corporation OptumCare Network of Connecticut
Health Advantage, Inc. • Arizona Priority Care Plus • Karen Gee, SVP & COO
Bakersfield Family Medical Center • California MemorialCare Medical Group * Rob Wenick, MD, VP & Medical Director
Desert IPA • California Physician Network • Coastal Mark Schafer, MD, CEO
Communities • Physician Network • Desert Oasis Laurie Sicaeros, COO, VP of Physician Alignment Orlando Family Physicians
Healthcare • Greater Covina Medical Group • Heritage Medhat Bedros, MD, Chief Medical Officer
Physician Network • Heritage Victor Valley Medical Mercy Health Physicians Roslynn ORourke, Chief Financial Officer
Group • High Desert Medical Group • Lakeside Michele Montague, COO
Pacific Medical Administrative Group
Community Healthcare • Lakeside Medical Group •
M E M B E R S
Meritage Medical Network Donna Mah, MD, President
Regal Medical Group • Sierra Medical Group Wojtek Nowak, CEO Michael Chang, MD, Executive Director
Hill Physicians Medical Group, Inc. * J. David Andrew, MD, Medical Director
Pediatric Associates
David Joyner, CEO Monarch HealthCare * Peter Shulman, MD, CEO
Amir Sweha, MD, CMO Bart Asner, MD, CEO Scott Farr, COO
Hoag Clinic Ray Chicoine, President
Peoples Health Network
Kris Iyer, MD, Sr. Vice President & Chief Administrative Montefiore Medical Center/IPA Warren Murrell, President and CEO
Officer Stephen Rosenthal, SVP Brent Wallis, MD, Medical Director
Scott Ropp, Vice President and CFO
Monterey Bay Independent Physician Groups: Health Prime, LLC • Independent
Innovare Health Advocates Association Physician Association of New Orleans, Inc. •
Charles Willey, MD, President & CEO James N. Gilbert, MD, President & Chairman of the Memorial Independent Physician Association, Inc.
Paul Beuttenmuller, CFO Board • North Shore Independent Physician Association,
IntegraNet Health Michele Wadsworth, Network Management Inc. • Pontchartrain IPA, Inc. • South Louisiana
Lawrence Wedekind, CEO Associate Independent Physician Association • University
Jaime Duarte, MD, Medical Director, Outpatient Medical Group, LLC
Mount Sinai Health Partners *
Intermountain HealthCare * Niyum Gandhi, EVP & Chief Population Health PHM MultiSalud, LLC
Rajesh Shrestha, COO Officer Roberto L. Bengoa Lopez, President
Robert Fields, MD, Senior Physician Leader on Lynnette Ortiz, MD, Medical Director
In Salud, Inc. Population Health
Groups: Advantage Medical Group • Alianza de
Armando Riega, President
MSO of Puerto Rico * Medicos del Sureste • Centro de Medicina Familiar
Carmen Ramos, CPA, Executive Director
Richard Shinto, MD, CEO del Norte • Centro de Medicina Primaria Advantage
Iora Health Inc. * Raul Montalvo, MD, President del Norte • Centros Medicos Unidos del Oeste •
Rushika Fernandopulle, MD, MPP, CEO G.M.D.C., Inc. • Grupo Advantage del Oeste • Grupo
Tyler Jung, MD, CMO NAMM California * Medico de G.M.B., Inc. • Grupo Medico de Orocovis
Leigh Hutchins, CEO
Jade Health Care Medical Group, Inc. Ken Cohen, MD Physicians Care Network
Edward Chow, MD, President & CEO Mary Anderson, MD, Medical Director
Groups: Coachella Valley Physicians of PrimeCare, Denis McDonald, Executive Director
Thomas Woo, Manager of Operations
Inc. • Empire Physicians Medical Group • Mercy
John Muir Physician Network * Physicians Medical Group • Primary Care Physicians DataTrust
Lee Huskins, President & CAO Associated Medical Group, Inc. • PrimeCare Kathi Toliver, VP of IPA Administration
Ravi Hundal, MD, CFO Medical Group of Chino • PrimeCare Medical Lisa Serratore, COO
Network, Inc. • PrimeCare of Citrus Valley •
Key Medical Group, Inc. Groups: Greater Tri-Cities IPA • Noble AMA IPA •
PrimeCare of Corona • PrimeCare of Hemet Valley
Brent Boyd, CEO St. Vincent IPA
Inc. • PrimeCare of Inland Valley • PrimeCare
James Foxe, MD, Medical Director of Moreno Valley • PrimeCare of Redlands • Physicians of Southwest Washington, LLC
Landmark Medical, PC PrimeCare of Riverside • PrimeCare of San Melanie Matthews, CEO
Michael H. Le, MD, President Bernardino • PrimeCare of Sun City • PrimeCare Gary R. Goin, MD, President
of Temecula • Redlands Family Practice Medical
Leon Medical Centers, Inc. Group, Inc. PIH Health Physicians
Rafael Mas, MD, SVP & CMO Rosalio J. Lopez, MD, SVP & CMO
Julio G. Rebull, Jr., SVP NaviHealth, Inc. Andrew Zwers, Chief Operating Officer
Jay LaBine, MD, CMO
Loma Linda University Health Care Gina Bruno, MBA, VP, Clinical Strategy Pioneer Medical Group, Inc. *
J. Todd Martell, MD, Medical Director Jerry Floro, MD, President
A P G
New West Physicians, P.C. * Andrew Zwers, Chief Operating Officer
Managed Care Management and Educational, Ken Cohen, MD, CMO
LLC Portland IPA
Luis Deliz Varela, MD, Medical Director Northwest Permanente, P.C. * Susan Clack, MD, President and Board Chair
Guido Lugo Modesto, Esq., Administrator Colin Cave, MD, Director of External Affairs, Pamela Bauer, CEO
Government Relations and Community Health
Marshfield Clinic, Inc. * Marilyn Weber, Chief Financial Officer Preferred IPA of California
Narayana Murali, MD, EVP & CSO Mark Amico, MD, Medical Director
Northwest Physicians Network of Zahra Movaghar, Administrator
Martin Luther King, Jr. Community Medical Washington, LLC
Group Jesse Gamez, COO Premier Family Physicians
John Fisher, MD, MBA, President Kevin Spencer, MD, CEO and President
Laurie Gallagher, Practice Administrator Ochsner Clinic Foundation Mat King, CFO
Philip M. Oravetz, MD, Chief Population Health
Medicos Selectos del Norte, Inc. Officer PriMed Physicians
Mildalias Dominguez Pascual, MD, President Mark Couch, MD, President
Fernando A. Garcia Cruz, MD Ohio Integrated Care Providers Robert Matthews, VP of Quality
Cindy M. Baker, CEO
MedPOINT Management Patrick Goggin, MD, Quality Improvement Medical Prisma Health *
Kimberly Carey, President Director Angelo Sinopoli, MD, Chief Clinical Officer
Rick Powell, MD, CMO
OHSU Health IDS, LLC Privia Medical Group LLC
Groups: • Associated Hispanic Physicians of Southern Katrina McPherson, MD, Chief Medical Officer Keith Fernandez, MD, National Chief Clinical Officer
California IPA • Bella Vista Medical Group, IPA • Jeff Conklin, Chief Executive Officer Graham Glaka, VP, New Product Development
Centinela Valley IPA • Crown City Medical Group •
El Proyecto del Barrio, Inc. • Family Care Specialists Omnicare Medical Group ProHealth Physicians, Inc.
IPA • Global Care Medical Group IPA • Golden Toni Chavis, MD, President Jack Reed, President & CEO
Physicians Medical Group, Inc. • Health Care LA IPA Ashok Raheja, MD, Medical Director Rich Guerriere, MD, SVP & CMO
22 l JOURNAL OF AMERICA’S PHYSICIAN GROUPS Summer 2020You can also read