Navigating the Cancer Continuum - in the Context of Value-Based Care Patient Navigation in Cancer Care 2.0 - Pfizer for Professionals
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Patient Navigation in Cancer Care 2.0 Guiding patients to quality outcomes Navigating the Cancer Continuum in the Context of Value-Based Care
2 NAVIGATING THE C ANCER CONTINUUM
TABLE OF CONTENTS
I. Introduction 3
II. Past, Present, and Future of Navigation 5
III. Defining Navigation 9
IV. Navigation Core Competencies 11
V. Navigator Role Delineation 13
VI. Models of Navigation 15
VII. Barriers to Care 19
VIII. Distress and Psychosocial Needs 23
IX. Health Literacy 29
X. The Chronic Care Model and Cancer Care Continuum 31
XI. Community Outreach and Prevention 33
XII. Navigation Program Development 45
XIII. Navigation Program Monitoring and Outcome Measures 49
XIV. Metrics 51
XV. Professional Development 55
XVI. Navigation Topics for Professional Development 59
XVII. Conclusion 63
XVIII. Navigation Resources 65I. Introduction
3
I. INTRODUCTION
Since the development of the 2014 Pfizer Evolu- resources to decrease costs across oncology pa-
tion of Navigation slide deck, the healthcare envi- tient populations and healthcare settings.
ronment—including oncology—has changed and Navigation, with its various models, has had to
continues to evolve. With the rising incidence of evolve beyond identifying barriers to incorporate
cancer, an aging population, and advances in core competencies, certification, and standard-
the technology of treatment modalities, the cost ized metrics to help drive continuous quality im-
of cancer is burdensome on both patients and provement and value while identifying evi-
society. The focus of healthcare is shifting to a dence-based best practices that elevate cancer
landscape of value-based care, with health out- care to a grander scale. Value-based care is the
comes achieved per dollars spent. future of cancer management, and the compe-
Value-based care is the concept of improving tencies of navigation help ensure consistent deliv-
quality and outcomes for patients by standardizing ery of optimized patient care across the care
healthcare processes through best practices.1 continuum and align and support this goal.
Navigation is integral to meeting these goals by
facilitating effective interprofessional collabora- Reference
1. Cleveland Clinic website. Value-Based Care. https://my.cleve
tion and promoting patient satisfaction and care
landclinic.org/health/articles/15938-value-based-care. Accessed
quality, as well as the efficient use of healthcare August 14, 2018.II. PAST, PRESENT, AND FUTURE OF NAVIGATION 5
Future of Navigation
II. Past, Present, and
II. PAST, PRESENT, AND FUTURE OF NAVIGATION
Past Initiatives in reach and the elimination of bar- management and patient navi-
Navigation riers to care. To that end, he gation/care coordination, with
Dr. Harold Freeman con- offered free or low-cost breast the goal of identifying and re-
ceived and initiated the na- examinations and mammograms ducing barriers to care (Table 1).2
tion’s first patient navigation coupled with one-on-one navi- With this evolution, the process
program in 1990. This followed gation services. As a result, 5-year of a multidisciplinary team ap-
just over 2 decades of observa- survival rates increased among proach, which centered on open
tion of more than 606 patients this population, from 39% before communication, was developed
with breast cancer treated at intervention to 70% following the to address the psychosocial
Harlem Hospital Center; of these initiation of his patient navigation distresses and financial concerns
patients, 94% were African Amer- program. Dr. Freeman was able of patients, as well as coordi-
ican. This population of dispro- to demonstrate that 5-year can- nate care needs. The process
portionately poor and uninsured cer survival rates can be im- of navigation cultivated the
patients had a high incidence proved with increased access to bidimensional care concept—
of breast cancer mortality and screening and patient naviga- patient-centered, to ensure con-
often presented with more ad- tion programs by addressing and tinuity of care; and health sys-
vanced stages of disease com- working to eliminate issues pre- tem–oriented, to empower pa-
pared with patients living out- sented by lack of health insur- tients and their families—as
side of this community.1 ance, fear and distrust of the oncology care moved to a pre-
Dr. Freeman’s program fo- medical community, and cultur- dominantly outpatient setting.3
cused on the window of oppor- al and communication barriers.1 The navigation model cur-
tunity that was critical to saving The scope of navigation, includ- rently in use was developed fol-
patients from cancer mortality, ing nurse and patient navigation, lowing several organizational
by eliminating barriers to timely has evolved from the Harold P. and government reports and
care that were typically en- Freeman Patient Navigation initiatives focused on decreas-
countered between the point Model of community outreach ing healthcare disparities, elimi-
of a suspicious finding and the and prevention and can now nating barriers to care, and im-
resolution of that finding by fur- span the entire continuum of proving the overall patient
ther diagnosis and treatment. care for oncology patients.1 experience. One such report,
For example, he observed de- Although Dr. Freeman brought the American Cancer Society’s
lays in follow-up care after ab- the patient navigation move- 1989 Report to the Nation: Can-
normal findings or cancer diag- ment to the forefront of health- cer in the Poor, identified the 5
noses, and therefore proposed care delivery in the 1990s, the most critical issues related to
that patient navigators from the nursing profession had its own cancer among the poor.4 The
community could help address movement that had been evolv- report identified the critical is-
and bridge the gaps and barri- ing since the 1970s. The goal sues as: (1) poor people endure
ers that were prevalent between driving the development of the greater pain and suffering from
this patient population and the utilization review movement in cancer compared with other
healthcare system. One of the nursing included monitoring the Americans, (2) poor people and
major goals of what became use and delivery of services in the their families must make person-
known as the Freeman Model 1970s, which evolved into eval- al sacrifices to obtain and pay
was to expand access to cancer uating the appropriateness of for care, (3) poor people face
screenings and clinical follow-up medical care—including its need obstacles in obtaining and using
among the medically under- and efficiency—in the 1980s. The health insurance and often do
served through community out- 1990s brought the focus to case not seek care if unable to pay6 NAVIGATING THE C ANCER CONTINUUM
TABLE 1. Overview of the Evolution of Patient Navigation
Time Frame Relationship with
and Focus Role Other Providers Setting Methodology
1970s: Utilization Monitor use and delivery Adversarial Inpatient Retrospective chart
review of services review
1980s: Utilization Evaluate appropriateness, Adversarial Inpatient Concurrent chart
management medical need, and efficiency review
1990s: Case Assess, plan, implement, Collaborative Involved in Hands-on care
management coordinate, monitor, and evaluate patient care
1990s: Patient Identify and reduce barriers Collaborative Underserved Community outreach
navigation to access to care, diagnosis, patients
and prescription
2000-Present: Identify and reduce barriers Clinical Across the Hands-on care and
Patient navigation to access to care, diagnosis, Collaborative continuum coordination of care
and prescription of care
Source: Shockney L. Evolution of patient navigation. Clin J Oncol Nurs. 2010;14:405-407. Reprinted with permission. Copyright 2010 by Oncology Nursing
Society. All rights reserved.
for it, (4) cancer education pro- (Standard 3.1), which became of tobacco use, alcohol/sub-
grams are culturally insensitive effective in 2016, requires that stance abuse, and/or mental
and irrelevant to many poor cancer programs seeking CoC illness).8 The CNA should list re-
people, and (5) fatalistic ideas accreditation establish a pro- sources available within the
about cancer are prevalent cess to identify and navigate community, as well as point out
among the poor and prevent potential barriers to care, and disparities and gaps in resourc-
them from seeking care.4 Addi- document that process each es.7,8 Taking these steps allows
tional reports and initiatives fo- calendar year.7,8 The process the program to identify priorities
cused on addressing barriers to must be driven by a community aimed at addressing barriers to
care include the US National needs assessment (CNA) that is care and implement programs,
Cancer Institute’s report, Voices conducted at least once every services, and/or partnerships to
of a Broken System: Real Peo- 3 years.7,8 The CNA systematical- overcome them, thereby im-
ple, Real Problems, which indi- ly evaluates processes currently proving outcomes among the
cated that barriers to cancer in place within the facility and target population.8 To stream-
care exist for people of all socio- gathers information to identify line this process and decide on
economic levels5; and the Pa- the community being served, as a plan to overcome barriers,
tient Navigator Outreach and well as any barriers to care that needs related to patients’ ac-
Chronic Disease Prevention Act may exist within that communi- cess, education, treatment,
of 2005, which ensured that ty.7,8 Relevant data collection monitoring, psychological sup-
navigators are accessible to all can include geographic loca- port, and the overall patient
patients with cancer, to provide tions served (urban, suburban, navigation process would be
high-quality, coordinated care.6 rural); socioeconomic charac- considered (Figure 1).7,8
teristics of the sample popula-
Present Initiatives in tion (eg, median household in- Alternative Payment
Navigation come, housing status, average Models and the
In 2012, the American College education level, immigration Future of Navigation
of Surgeons Commission on Can- status, employment status, avail- The complex healthcare
cer (CoC) released standards ability of public transportation); landscape (including its pay-
that reflected the goal of ensur- race/ethnicity; median age; and ment system) has evolved over
ing patient-centered care.7 One behavioral and psychosocial the past 4 decades and will
of the more recent standards health characteristics (eg, rates continue to evolve in the future.II. PAST, PRESENT, AND FUTURE OF NAVIGATION 7
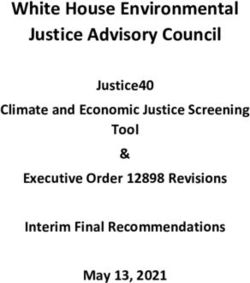
FIGURE 1. Requirements of a Community Needs Assessment (CNA)
incentives, including perfor-
The CNA Must Define/Identify: mance-based payments, to im-
The cancer program’s community and local population(s) prove care coordination, ap-
Description of facility, number of patients with cancer served, range propriateness of care, and
of cancer-related clinical services, prevention and detection programs access for beneficiaries under-
Health disparities (numerous factors can contribute to disparities in going chemotherapy.11,13 It tar-
cancer incidence and death rates, such as race, ethnicity, gender, under- gets oncology practices deliv-
served groups, and socioeconomic status)
ering chemotherapy treatment
Use local, state, and national resources to compile data
Compare cancer program data with national and regional data and the spectrum of care pro-
Barriers to care, which may include patient-centered, provider-centered, vided to a patient during a
or health system–centered barriers 6-month episode following the
Resources available to overcome barriers on-site or by formal referral start of chemotherapy.13 The
Perform internal and external resource mapping to examine OCM is meant to shift reimburse-
existing resources ment and payment to val-
Gaps in the availability of resources to overcome barriers ue-based quality care, which
Create an action plan with SMART goals to address gaps includes patient navigation as a
SMART indicates specific, measurable, achievable, realistic, and timely. foremost component.13 The
Sources: Commission on Cancer (CoC). Cancer Program Standards: Ensuring Patient-Centered Care. Merit-Based Incentive Payment
2016 ed. Chicago, IL: American College of Surgeons. www.facs.org/quality-programs/cancer/coc/
standards. Accessed June 13, 2018; and The George Washington University Cancer Center.
System (MIPS) is another pay-
Implementing the Commission on Cancer Standard 3.1 Patient Navigation Process: A Road Map for ment mechanism instituted by
Comprehensive Cancer Control Professionals and Cancer Program Administrators. Washington, DC: the Centers for Medicare &
September 2017.
Medicaid Services that will pro-
vide annual updates to physi-
In today’s healthcare environ- patient populations and health- cians starting in 2018, based on
ment, key organizations drive care settings. performance in 4 categories:
the focus on quality, outcomes, The Center for Medicare & quality, resource use/cost, clini-
and evidence-based practice. Medicaid Innovation (the Inno- cal practice improvement ac-
The Institute for Healthcare Im- vation Center) is developing tivities, and advancing care in-
provement Triple Aim Initiative new alternative payment and formation.14 Using a composite
seeks to improve the patient delivery models aimed at im- performance score, eligible pro-
experience of care (including proving the effectiveness and fessionals may receive a pay-
quality and satisfaction), im- efficiency of specialty care.11 ment bonus, a payment penal-
prove the health of populations, An alternative payment model ty, or no payment adjustment.
and reduce the per capita cost (APM) is a payment approach The importance of care coordi-
of healthcare.9 Value-based that gives added incentive pay- nation is highlighted under the
cancer care is a highly coordi- ments for the provision of high- MIPS improvement activities.
nated, patient-centered solu- quality and cost-efficient care. The premise of value-based
tion to address rising healthcare APMs can apply to a specific care is that better coordinated
costs, ineffective duplication of clinical condition, a care epi- and connected patient care
services, and barriers to care.10 sode, or a population.12 Among will improve outcomes and
Navigation is integral to meet- specialty models is the Oncolo- lower costs. Navigators play a
ing these goals by facilitating gy Care Model (OCM) launched critical role in the coordination
effective interprofessional col- in July 2016, which aims to pro- of care and patient empower-
laboration and promoting pa- vide higher quality, better coor- ment through education, pa-
tient satisfaction and care qual- dinated oncology care at the tient-reported outcomes, and
ity, as well as the efficient use of same or lower cost as Medi- emotional support. Patients who
healthcare resources to de- care.11,13 The OCM is a 5-year have access to “easy to under-
crease costs across oncology model that combines financial stand” information, education,8 NAVIGATING THE C ANCER CONTINUUM
and self-care instructions are fessional navigation framework: elabo- fessionals and Cancer Program Adminis-
ration and validation in a Canadian trators. Washington, DC: September 2017.
better prepared to adhere to context. Oncol Nurs Forum. 2012;39(1): 9. Institute for Healthcare Improvement.
treatment, manage side ef- E58-E69. IHI Triple Aim Initiative. www.ihi.org/en
4. American Cancer Society (ACS). A gage/initiatives/TripleAim/Pages/de
fects, and, ultimately, have the summary of the American Cancer Society fault.aspx. Accessed June 11, 2018.
potential for achieving better Report to the Nation: cancer in the poor. 10. Strusowski T. Navigation metrics and
CA Cancer J Clin. 1989;39(5):263-265. value-based care. https://aonnonline.org/
outcomes. Navigators serve pa- 5. National Institutes of Health (NIH). Na- expert-commentary/navigation-101/867-
tients by acting as direct tional Cancer Institute. Voices of a Bro- navigation-metrics-and-value-based-
ken System: Real People, Real Problems. care. Accessed June 13, 2018.
contacts to whom patients may President’s Cancer Panel Report of the 11. Centers for Medicare & Medicaid
Chairman, 2000-2001. Bethesda, MD. Services (CMS). Oncology Care Model.
report symptoms as they arise, 6. H.R. 1812, 109th Congress of the Unit- https://innovation.cms.gov/initiatives/
as opposed to allowing the ed States (2005-2006). Patient Navigator Oncology-Care/. Accessed June 11, 2018.
Outreach and Chronic Disease Preven- 12. Centers for Medicare & Medicaid
consequences of underreport- tion Act of 2005. www.congress.gov/ Services (CMS). APMs overview. https://
ing symptoms to escalate in se- bill/109th-congress/house-bill/1812/text/ qpp.cms.gov/apms/overview. Accessed
pl. Accessed June 16, 2018. June 11, 2018.
verity, potentially leading to 7. Commission on Cancer (CoC). Can- 13. Centers for Medicare & Medicaid
hospitalization. cer Program Standards: Ensuring Pa- Services (CMS). Oncology care model
tient-Centered Care. 2016 ed. Chicago, [press release]. Baltimore, MD: CMS;
IL: American College of Surgeons. www. June 29, 2016. www.cms.gov/Newsroom/
References facs.org/quality-programs/cancer/coc/ MediaReleaseDatabase/Fact-sheets/
1. Freeman H, Rodriguez RL. History and standards. Accessed June 13, 2018. 2016-Fact-sheets-items/2016-06-29.html.
principles of patient navigation. Cancer. 8. The George Washington University Accessed June 16, 2018.
2011;117:3539-3542. Cancer Center. Implementing the 14. Centers for Medicare & Medicaid
2. Shockney L. Evolution of patient navi- Commission on Cancer Standard 3.1 Services (CMS). MIPs overview. https://
gation. Clin J Oncol Nurs. 2010;14:405-407. Patient Navigation Process: A Road Map qpp.cms.gov/mips/overview. Accessed
3. Fillion L, Cook S, Veillette A, et al. Pro- for Comprehensive Cancer Control Pro- June 11, 2018.III. DEFINING NAVIGATION 9
III. DEFINING NAVIGATION
The importance of naviga- families, and caregivers to assist ation of Oncology Social Work,
tion and the roles of nurse and in overcoming barriers to re- and the National Association of
III. Defining Navigation
patient navigators have been ceiving care and facilitating Social Workers developed a
recognized by various organiza- timely access to clinical services joint position on navigation. The
tions, such as the Commission and resources. Navigation pro- position adapted an earlier defi-
on Cancer (CoC), the Ameri- cesses encompass prediagnosis nition of patient navigation in
can Cancer Society, the Acad- through all phases of the cancer the cancer care setting from
emy of Oncology Nurse & Pa- experience. The navigation ser- C-Change, modifying it slightly
tient Navigators (AONN+), and vices implemented will depend to consist of “[i]ndividualized as-
the Oncology Nursing Society upon the particular type, severi- sistance offered to patients,
(ONS). Although these organiza- ty, and/or complexity of the families, and caregivers to help
tions sometimes use overlap- identified barriers.”1 AONN+ de- overcome healthcare system
ping terminology, they have fines the navigation process as barriers and facilitate timely ac-
cess to quality health and psy-
chosocial care from prediagno-
Navigation is the process of “[h]elping patients sis through all phases of the
overcome healthcare system barriers and cancer experience.”3
providing them with the timely access to quality
References
medical and psychosocial care from before 1. Commission on Cancer (CoC). Can-
cer Program Standards: Ensuring Pa-
cancer diagnosis through all phases of their tient-Centered Care. 2016 ed. Chicago,
IL: American College of Surgeons. www.
cancer experience.”2 facs.org/quality-programs/cancer/coc/
standards. Accessed March 26, 2018.
2. Academy of Oncology Nurse & Pa-
tient Navigators (AONN+). Helpful def-
nonetheless each been signifi- “[h]elping patients overcome initions. www.aonnonline.org/education/
helpful-definitions. Accessed June 13, 2018.
cant in developing guidance, healthcare system barriers and 3. Oncology Nursing Society (ONS), Asso-
competencies, and standards providing them with timely ac- ciation of Oncology Social Work (AOSW),
National Association of Social Workers
for the profession of navigation. cess to quality medical and psy- (NASW). Oncology Nursing Society, the
Association of Oncology Social Work,
According to the CoC, “[p]a- chosocial care from before and the National Association of Social
tient navigation in cancer care cancer diagnosis through all Workers joint position on the role of on-
cology nursing and oncology social
refers to specialized assistance phases of their cancer experi- work in patient navigation. Oncol Nurs
for the community, patients, ence.”2 In 2010, ONS, the Associ- Forum. 2010;37(3):251-252.IV. NAVIGATION CORE COMPETENCIES 11
IV. NAVIGATION CORE COMPETENCIES
Navigators serve in many roles recognized domains of compe- the development of an evi-
as educators, care facilitators, tency recommended by the dence-based or promising/best
counselors, and patient advo- NNRT for patient navigation: practice patient-centered plan
cates by providing education of care, which is inclusive of the
and psychosocial support, coor- I. Domain: Ethical, patient’s personal assessment as
dinating care across the continu- Cultural, Legal, and well as healthcare provider sys-
um of care and its disciplines, Professional Issues tem and community resources.
and assisting with financial needs. Competency: Demonstrates The navigator acts as a liaison
Navigators must demonstrate sensitivity and responsiveness to among all team members to ad-
IV. Navigation Core
competence in oncology, as a diverse patient population, vocate for patients to optimize
Competencies
well as the psychosocial and spir- including but not limited to: re- health and wellness with the over-
itual aspects of care for patients specting confidentiality; organi- all focus of improving access to
and families. Based on the needs zational rules and regulations; services for all patients. Naviga-
of the community and the navi- ethical principles; and diversity tors conduct patient assessments
gation program, elements of the in gender, age, culture, race, (needs, goals, self-management,
skill set should include knowledge ethnicity, religion, abilities, sexu- behaviors, strategies for improve-
in health promotion; past work or al orientation, and geography. ment) integrating patients’ per-
personal experience within the sonal and cultural values.
healthcare field; language skills II. Domain: Patient/Client
to effectively communicate with and Care Team Interaction V. Domain: Practice-
the populations served; and ca- Competency: Applies insight Based Learning
pability in forming relationships, and understanding concerning Competency: Optimizes navi-
working well on a team, prob- human emotional responses to gator practice through continual
lem-solving, and demonstrating create and maintain positive professional development and
leadership when required. interpersonal interactions lead- the assimilation of scientific evi-
The recently created National ing to trust and collaboration dence to continuously improve
Navigation Roundtable (NNRT), between patient/family/care- patient care, based on individual
sponsored by the American Can- givers and the healthcare team. navigator gaps in knowledge,
cer Society, is a national coalition Patient safety and satisfaction skills, attitudes, and abilities.
of more than 40 member organi- are priorities.
zations and individuals who are VI. Domain: Systems-
dedicated to achieving health III. Domain: Health Based Practice
equity and access to care across Knowledge Competency: Advocates for
the cancer continuum. Its goal is Competency: Demonstrates quality patient care by acknowl-
to advance navigation efforts breadth of knowledge about edging and monitoring needed
that eliminate barriers to cancer health, the cancer continuum, (desirable) improvements in sys-
care, reduce disparities in health psychosocial and spiritual as- tems of care for patients, from
outcomes, and foster ongoing pects, and attitudes and be- enhancing community relation-
health equity.1 The NNRT website haviors specific to their patient ships and outreach through end-
(www.navigationroundtable.org) navigation (clinical/licensed or of-life care. This includes en-
will have updates and additions nonmedical licensure) role. hancing community relationships
to the national work being done and developing skills and knowl-
around training and education IV. Domain: Patient edge to monitor and evaluate
(competencies) for navigation.2 Care Coordination patient care and the effective-
The following are the 7 nationally Competency: Participates in ness of the program.12 NAVIGATING THE C ANCER CONTINUUM
VII. Domain: barriers, solutions, and re- References
1. Patient Navigator Training Collaborative.
Communication/ sources. Resolution of conflict Colorado patient navigation leaders help
Interpersonal Skills among patients, family mem- launch National Navigation Roundtable.
http://patientnavigatortraining.org/color
Competency: Promotes ef- bers, community partners, and ado-leaders-help-launch-national-naviga
fective communication and in- members of the oncology care tion-roundtable. Accessed June 13, 2018.
2. American Cancer Society National
teractions with patients in team is demonstrated in profes- Navigation Roundtable Training & Certifi-
cation Working Group. Navigator Core
shared decision-making based sional and culturally accept- Competencies. 2018. www.navigation
on their needs, goals, strengths, able behaviors. roundtable.org.V. NAVIGATOR ROLE DELINE ATION 13
V. NAVIGATOR ROLE DELINEATION
Clinically licensed navigators issues that may confront pa- type of evaluation based on
(ie, community health workers tients with cancer. Working at their scopes of practice and li-
[CHWs], patient navigators, nurse the top of their licensure, a nurse censure. During the course of
navigators, and social work navi- navigator or social work naviga- their work, CHWs focus their
gators) are 3 professional types tor should have knowledge of evaluation on the community’s
of navigation specialists with the clinical impacts of cancer needs and health behaviors.
overlapping yet distinct roles/re- on patients, caregivers, and Patient navigators straddle the
sponsibilities and competencies families, as well as the skills boundary between the com-
based on licensure. All 3 profes- needed to intervene on their munity and the healthcare set-
sional types of navigation are behalf (eg, assess functional ting by evaluating barriers to
involved with individual or pa- and psychosocial health and care and health disparities with-
tient education, but the types of manage symptoms).1 in the community against quali-
information provided can vary Regardless of the navigator ty indicators of the healthcare
based on training or education title, these 3 professional types system. For clinically licensed
and professional level. Although must have a solid knowledge navigators, such as the nurse
CHWs should have general base and the expertise needed navigator or social work naviga-
V. Navigator Role
Delineation
knowledge on health issues to perform job-related duties tor within the healthcare sys-
such as cancer and chronic and tasks, including understand- tem, the focus of evaluation
diseases, the oncology patient ing one’s scope of practice, should be clinical outcomes
navigator should have knowl- supporting evaluation efforts, and quality indicators.1
edge of cancer screening and identifying and exercising
guidelines, diagnostic process- self-care strategies.1 Although Reference
1. Willis A, Reed E, Pratt-Chapman M, et
es, treatment options, and survi- these professional types share al. Development of a framework for pa-
tient navigation: delineating roles across
vorship, as well as related physi- the similarity of supporting eval- navigator types. J Oncol Navig Surviv.
cal, psychological, and social uation efforts, they differ in the 2013;4:20-26.VI. MODELS OF NAVIGATION 15
VI. MODELS OF NAVIGATION
Various models of navigation There are also hybrid models key. Community is the popu-
have evolved from Freeman’s of navigation in which programs lation as a whole, including
Patient Navigation Model, utiliz- can implement one type of the medically underserved, low-
ing community members known model or a combination of the income, or minority subpopula-
as lay navigators. Navigators various models of navigation to tions within the geographic area
who assist patients may come achieve the goal of eliminating served by the healthcare facility.
from oncology programs, as barriers to care and enabling The CNA helps identify the rele-
well as from within the commu- patients to move seamlessly vant healthcare disparities and
nity itself. Current models of across the care continuum. Insti- barriers to care that exist within a
navigation include clinical nurse tutions/oncology programs are community so that a plan can
navigators (also known as on- able to develop and implement be developed to meet these
cology nurse navigators), social a useful navigation program challenges. The specific require-
workers, patient navigators (also based on their type of naviga- ments of the target population
referred to as nonclinically li- tion model and the specific will dictate the greatest service
censed navigators), community needs and goals of the pro- needs, and the skill set and
healthcare workers as volun- gram, as well as address the model of navigation should align
teers or advocacy/organiza- needs of the community served. with these. For example, rural
tional employees, and financial To effectively formulate the populations may find that the
navigators specializing in finan- navigation process for a particu- greatest service need is transpor-
cial issues that impact care lar cancer program, the commu- tation to and from appointments,
(Figure 1).1,2 nity needs assessment (CNA) is for which the navigator will focus
VI. Models of
FIGURE 1. Navigation Models
Navigation
Nurse Navigator Patient or Nonclinically Licensed
A professional registered nurse with Navigator/ACS Patient Resource
oncology-specific knowledge. Using Navigator
the nursing process, the nurse With a basic understanding of
navigator provides education and cancer, healthcare systems, and
resources to facilitate informed how patients access care and
decision-making and timely access services across the cancer
to quality health and psychosocial care throughout all continuum, they connect patients to information,
phases of the cancer continuum resources, and support
Social Work Navigator
Social worker with oncology-specific
Other
clinical knowledge, who offers
individualized assistance to patients, Community Healthcare Workers
families, and caregivers to help Financial Navigators
overcome healthcare system barriers
and psychosocial assessment and Volunteer Navigator
intervention
Source : Adapted from Bellomo C. Navigating the Cancer Continuum: Best Practices in Navigation. Presented at: Western Colorado Oncology Nursing
Conference; October 21, 2017; Grand Junction, CO.16 NAVIGATING THE C ANCER CONTINUUM
on finding vouchers or resources revalence of health
P Goals of Navigation
to provide low-cost transporta- conditions Navigators may assist patients,
tion. In addition, immigrant com- Insurance their families, and caregivers in
munities benefit from navigators Environmental factors rural or urban communities or
who offer services in their lan- Causes of death academic settings. Clinical nurse
guage and possess a keen un- Sources of data navigators may function as a
derstanding of relevant cultural Cancer registry tumor-specific navigator (eg,
issues. Navigation programs can Organization’s marketing breast, thoracic, hematologic)
be focused on the nonclinical or department or as a multisite/general naviga-
lay navigator’s perspective, with US Census Bureau tor. No matter the setting or dis-
the navigator performing non- Centers for Disease ease type, navigators share the
clinical tasks that include sched- Control and Prevention same roles, responsibilities, com-
uling, interpreter services, and State department of petencies, and goals within their
identifying and/or addressing fi- health scope of practice. Their focus is
nancial needs. Other navigation Centers for Medicare & to offer individualized assistance
programs may focus on the clini- Medicaid Services to the patient and family, reduce
cal nurse navigator, who has American Cancer Society’s barriers, and increase access to
oncology-specific knowledge to Cancer Facts & Figures medical and psychosocial care
provide education and resourc- reports. across the entire continuum.
es to facilitate informed deci- Step 3: Within the multidisciplinary
sion-making; is able to address Administer surveys team, the navigator works as an
symptom management and Patient, families, and advocate, care provider, edu-
clinical aspects of care; and can caregivers cator, counselor, and facilitator
provide psychosocial care. Healthcare professionals to ensure that every patient re-
Based on the needs of the com- Key stakeholders. ceives comprehensive, timely,
munity served, navigation pro- Step 4: and quality healthcare ser-
grams may incorporate social Collect and analyze all data. vices.3 The goals of navigation
workers to assist with logistical Step 5: can be described by 5 catego-
needs, as well as provide psy- Community Health Needs ries (Figure 2)1,4:
chosocial care and support. Assessment written report Coordination of care –
Report findings to cancer Coordination of care
How to Conduct a CNA3 committee involves ensuring timely
Step 1: Discuss findings access to support services,
Establish a work group Formulate patient navigation appointments, tests, and
responsible for conducting process and discuss the procedures
and reporting the CNA process with the cancer Education of patients –
Multidisciplinary team committee. Navigators provide patient-
approach Step 6: centered education to
Create a timeline of SWOT analysis patients, families, and
activities. Develop strategic caregivers on the cancer
Step 2: implementation on how the diagnosis; treatment; side
Collect and review data organization plans to effects and management;
of the community prioritize needs that were and clinical trials, to ensure
Demographic data of identified in the assessment. that they are informed and
primary service area involved in the shared
Population trends See Appendix for Sample decision-making process
Poverty rates Work Plan for Community Needs Providing psychosocial
Educational attainment Assessment. support – Facilitating theVI. MODELS OF NAVIGATION 17
FIGURE 2. The Goals of Oncology Navigation
COORDINATE CARE
Timely access to care
and support service,
appointment, referrals,
test, procedures, and
other consults
EDUCATE
ADVOCATE
Diagnosis
Serve as the patient Treatment
advocate to ensure Management of side
their voice is heard effects
Clinical trials
Shared decision-making
IDENTIFY
Barriers to care
Resources for patients PROVIDE
and caregivers Psychosocial support
Patients’ life goals to patient and family
and incorporate
into treatment plan
Source : Adapted from Strusowski T. Navigation and Survivorship 101. Presented at: Academy of Oncology Nurse & Patient Navigators (AONN+) 6th Annual
Navigation & Survivorship Conference; October 1-4, 2015; Atlanta, GA.
development of coping skills, resources while ensuring as Presented at: Western Colorado Oncolo-
and referral to psychosocial the patient’s advocate that gy Nursing Conference; October 21,
2017; Grand Junction, CO.
resources their goals, preferences, and 3. Johnston D. Evidence into Practice
Identification of barriers and voice are heard. Subcommittee Meeting. Commission on
Cancer Standard 3.1: Patient Navigation
resources – Helping to Process. Presented at: Academy of Oncol-
improve access to needed References ogy Nurse & Patient Navigators (AONN+)
1. Strusowski T. Navigation and Survivor- 6th Annual Navigation & Survivorship Con-
patient resources ship 101. Presented at: Academy of ference; October 1-4, 2015; Atlanta, GA.
Oncology Nurse & Patient Navigators 4. Strusowski T, Sein E, Johnston D, et al.
Advocating for patients – (AONN+) 6th Annual Navigation & Survi- Standardized evidence-based oncolo-
Identifying and overcoming vorship Conference; October 1-4, 2015; gy navigation metrics for all models: a
Atlanta, GA. powerful tool in assessing the value and
barriers to care by providing 2. Bellomo C. Navigating the Cancer impact of navigation programs. J Oncol
individualized assistance/ Continuum: Best Practices in Navigation. Navig Surviv. 2017;8:220-237.VII. BARRIERS TO C ARE 19
VII. BARRIERS TO CARE
To effectively coordinate care, compared with other patient navigators work closely with pa-
navigators must have an under- populations. Such obstacles can tients and families, they devel-
standing of health disparities (ie, include financial barriers; com- op a therapeutic and trusting
poverty, social injustice, or ra- munication barriers; healthcare relationship through open and
cial and ethnic biases) and literacy and healthcare system honest communication, there-
healthcare barriers (ie, cultural, barriers; and fear and distrust. by helping ensure that patients
socioeconomic, geographic, Many patients, particularly the and their families feel comfort-
and logistic) that patients may underserved and uninsured, able disclosing their specific
face. Although the term dispari- face significant barriers to re- needs and concerns related to
ty is often interpreted to mean ceiving timely diagnosis and care. Navigators should know
racial or ethnic inequalities, many quality of care (Table 1).2 the proper questions to ask to
dimensions of disparity exist in
the United States, particularly in
healthcare. If a health outcome A key function of the navigator is the provision
is seen in a greater or lesser ex- of tailored, culturally appropriate education
tent between populations, there
is a disparity.
to facilitate communication and collaboration
In phase I of the US Depart- based on findings of a learning needs assessment
ment of Health and Human Ser-
conducted to establish the patient’s
vices’ public health objectives
referred to as Healthy People current health literacy, preferred language,
2020, the term health disparity is motivation, and attitude.3
defined as “…a particular type
of health difference that is close-
ly linked with social or economic Barriers may be related to the elicit appropriate responses (eg,
disadvantage. Health disparities patient, physician, or healthcare “What would keep you from
adversely affect groups of peo- system. Socioeconomic barri- getting or undergoing care?”).
ple who have systematically ers—including poverty, lack of Navigators also conduct com-
experienced greater social or health insurance, inadequate prehensive assessments, such as
VII. Barriers to Care
economic obstacles to health insurance/inability to pay out-of- distress screenings, to elicit infor-
based on their racial or ethnic pocket costs, poor education, mation regarding physical, so-
group, religion, socioeconomic and unemployment—can have cial, emotional, cultural, and
status, gender, mental health, the greatest impact on the exis- spiritual needs. Based on the in-
cognitive, sensory, or physical tence of health disparities. The dividual needs and specific bar-
disability, sexual orientation, core principle of navigation is riers identified by the assess-
geographic location, or other the elimination of barriers to ments, navigators collaborate
characteristics historically linked timely, quality care throughout with other healthcare profes-
to discrimination or exclusion.”1 all phases of healthcare, includ- sionals and members of the mul-
ing prevention, detection, diag- tidisciplinary team to develop a
Barriers nosis, treatment, and survivorship. plan to address these issues.
Barriers to healthcare are ob- Increasingly, navigation pro- Navigators must understand
stacles that prevent vulnerable grams have been used as a and practice cultural awareness
patient populations from getting strategy to improve the timely in recognizing how culture can
the care they need or that cause receipt of needed healthcare influence healthcare. A key
them to get inferior healthcare services. During the time that function of the navigator is the20 NAVIGATING THE C ANCER CONTINUUM
TABLE 1. Barriers to Care Addressed by Navigators
Barriers Definition
Patient Focused
Co-morbidity Disability Disability (physical or mental) that makes getting healthcare difficult
Co-morbidity Medical or mental health problems that make getting healthcare difficult
Financial Insurance Paying for direct aspects of healthcare is a problem
Financial problems Dealing with financial problems (not directly related to healthcare) is
interfering with receiving healthcare (eg, not being able to pay food bills)
Housing Worrying about housing during healthcare
Attitudinal Attitudes toward providers Perceptions and beliefs about the healthcare providers who impact
receiving healthcare
Perceptions/beliefs about Personal or cultural beliefs that affect receiving healthcare
test or treatment
Not a priority Other issues take priority over healthcare
Fear Fear about any aspect of health or health-related care
Other Focused
Transportation Transportation Difficulty getting from home to healthcare site
Out of town/country Out of area during healthcare
Location of facility Distance from healthcare facility even if transportation is available
Interpersonal Social support Lacks a person/community for assistance during healthcare
Child care Not having child care when needed during healthcare
Adult care Difficulty finding support for other family members during healthcare
Employment demands Work demands make getting healthcare difficult
System Communication concerns Lacks understanding of the information provided by healthcare
with providers personnel
Literacy Difficulty understanding written communication from the healthcare
system
Language/interpreters Not sharing a common language for communication
System problems Care provided is not convenient/efficient to patient needs (eg, waiting
too long on the phone or in the office, days and hours of operation)
Source: Adapted from Katz ML, Young GS, Reiter PL, et al. Barriers reported among patients with breast and cervical abnormalities in the patient navigation
research program: impact on timely care. Womens Health Issues. 2014;24(1):e155-e162.
provision of tailored, culturally ventions to address barriers expe- preter assistance, referral to fi-
appropriate education to facili- rienced by patients with cancer. nancial assistance programs
tate communication and col- In an effort to remove barriers, (community, state, or national),
laboration based on findings of navigators connect patients to advocating for appointments
a learning needs assessment resources and support systems, with oncology specialists and
conducted to establish the pa- assist in the healthcare provider members of the multidisciplinary
tient’s current health literacy, interaction, and streamline ap- team, and connecting patients
preferred language, motivation, pointments and paperwork. Nav- with available community and
and attitude.3 igator interventions can include national support resources.
Navigators must be compe- arranging for logistical support Resources that connect pa-
tent in addressing, developing, (such as transportation, lodging, tients with available community
and implementing plans/inter- or child care), language inter- and national services includeVII. BARRIERS TO C ARE 21
CancerCare® and Advocacy connect with relevant cancer Healthy People 2020. Section IV: Advisory
Committee findings and recommenda-
Connector. CancerCare® (www. advocacy group resources. (See tions. Washington, DC: HHS; October 28,
cancercare.org/helpinghand) Navigation Resources section for 2008. www.healthypeople.gov/sites/de
fault/files/PhaseI_0.pdf. Accessed June
is a searchable, online database more information.) 13, 2018.
2. Katz ML, Young GS, Reiter PL, et al.
of financial and practical assis- Barriers reported among patients with
tance available for people with References breast and cervical abnormalities in the
1. US Department of Health and Human patient navigation research program:
cancer. Advocacy Connector Services (HHS), The Secretary’s Advisory impact on timely care. Womens Health
(https://advocacyconnector. Committee on National Health Promo- Issues. 2014;24(1):e155-e162.
tion and Disease Prevention Objectives 3. McDonald C. A first-hand look at the
com) is a resource designed to for 2020. Phase I Report: Recommenda- role of the breast cancer nurse naviga-
help patients and caregivers tions for the Framework and Format of tor. Care Manag. 2011;17:11-13, 27-28.VIII. DISTRESS AND PSYCHOSOCIAL NEEDS 23
VIII. DISTRESS AND PSYCHOSOCIAL NEEDS
The cancer experience can FIGURE 1. Periods of Increased Vulnerability for Distress
have a life-changing impact on
Finding a suspicious symptom Medical follow-up and surveillance
individuals, including the need
to accept loss, a perceived lack During diagnostic workup Treatment failure
of control in some situations, and Awaiting treatment Recurrence/progression
fear of recurrence.1 Psychologi- Changing treatment modality Advanced cancer
cal problems created or exacer-
End of treatment End of life
bated by the diagnosis of cancer
can include depression, anxiety, Discharge from hospital
stress, and other emotional is- Source : Adapted with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN
Guidelines®) for Distress Management V.2.2018. © 2018 National Comprehensive Cancer Network,
sues, which can be compound- Inc. All rights reserved. The NCCN Guidelines® and illustrations herein may not be reproduced in
ed by psychosocial aspects such any form for any purpose without the express written permission of NCCN. To view the most recent
and complete version of the NCCN Guidelines, go online to NCCN.org. The NCCN Guidelines are a
as a lack of information or skills work in progress that may be refined as often as new significant data becomes available.
needed to manage the illness; a
lack of transportation or sup-
portive services; financial pres- abling, such as depression, anx- treatment modality, end of treat-
sures; and disruptions in work, iety, panic, social isolation, and ment, discharge from the hospi-
school, and family life. Distress existential and spiritual crisis.”2 tal following treatment, medical
encompasses the emotional, To deliver high-quality cancer follow-up and surveillance, treat-
physical, and psychological as- care, the Commission on Cancer ment failure, recurrence/pro-
pects of facing a cancer diag- (CoC) Standard 3.2 incorporates gression, advanced cancer, and
nosis and its treatment. Patients, distress screening into routine end of life (Figure 1).2 In addition,
families, and treatment teams cancer care. The CoC recom- documentation of each pa-
should be informed that man- mends that all patients with can- tient’s screening process and as-
agement of distress is an inte- cer be screened for distress a sociated findings is encouraged,
gral part of total medical care minimum of 1 time during a piv- to properly assess psychosocial
and includes appropriate infor- otal medical visit such as post- needs so that they may be ad-
mation about psychosocial ser- surgical visits, the initial discussion dressed through tools, resources,
vices in the treatment center of chemotherapy with a medi- and support services designed
and the community.1,2 The Na- cal oncologist, at a routine visit to improve patient outcomes.2,3
tional Comprehensive Cancer with a radiation oncologist, or at A failure to acknowledge and
Network® (NCCN®) defines dis- a postchemotherapy follow-up measure distress stemming from
tress as “…a multifactorial un- visit. Pivotal medical visits that clinical depression in patients
pleasant emotional experience confer the greatest risk for dis- can cause impaired functioning
of a psychological (ie, cognitive, tress could be given preference, and decreased adherence to
Psychosocial Needs
behavioral, emotional), social, such as at the time of diagnosis, treatment and medication usage, VIII. Distress and
spiritual, and/or physical nature transitions during treatment (ie, which in turn may lead to poorer
that may interfere with the ability from chemotherapy to radiation clinical outcomes.4,5 Depression
to cope effectively with cancer, therapy), or transitions off treat- is a common psychological
its physical symptoms, and its ment. Other periods of increased symptom experienced by pa-
treatment. Distress extends along vulnerability for distress among tients with cancer that, if left un-
a continuum ranging from com- patients with cancer may include checked, can cause significant
mon normal feelings of vulner- finding a suspicious symptom, distress that may lessen quality of
ability, sadness, and fears to during diagnostic workup, while life.4 Many studies confirm that
problems that can become dis- awaiting treatment, changing distress is often overlooked and24 NAVIGATING THE C ANCER CONTINUUM
that many patients do not re- developed as a visual analog counseling, or chaplaincy ser-
ceive appropriate screening or tool for patients to indicate the vices) would best serve the pa-
treatment for it.4,6 level of distress they encounter tient for referral.2
As early as 2007, the Institute of in the week preceding a health- Screening for psychosocial
Medicine (IOM) highlighted the care-related visit. This tool is de- distress along the cancer con-
serious implications of unmet psy- signed to screen for distress only tinuum allows navigators to
chosocial needs faced by pa- and is not a diagnostic tool for address patients’ perceptions of
tients with cancer and their fami- measuring depression or anxiety.2 quality of life. Effective psycho-
lies in its report, Cancer Care for This single-page tool includes social care, consisting of a multi-
the Whole Patient: Meeting Psy- a visual representation of a ther- disciplinary team approach, has
chosocial Health Needs. The IOM mometer with numbers ranked been shown to positively influ-
report emphasized the impor- from lowest (no distress) to high- ence patient outcomes and
tance of screening patients for est (extreme distress), and in- quality of life.8 The NCCN Distress
distress and conducting a psy- cludes a list of potential prob- Thermometer has a secondary
chosocial needs assessment to lems at the right for patients to benefit of connecting many pa-
formulate the provision of self-identify (Figure 2).2 The Dis- tients to services that might not
high-quality healthcare. The re- tress Thermometer can facilitate otherwise have been identified.
port acknowledged that these a conversation between the pa- Distress screening provides pa-
tools can be used as part of stan- tient and healthcare provider to tients an opportunity to partner
dard clinical care and to en- better elicit what is contributing with their healthcare team,
hance patient–provider commu- to the patient’s concerns and overcomes patients’ reluctance
nication. A variety of screening how these issues can be effec- to ask for help, destigmatizes the
instruments were reviewed, many tively resolved. Asking patients, issue and allows patients to
of which are brief and can be “On a scale of 1 to 10 and in- share their vulnerabilities, and
self-administered by the patient.7 cluding today, how much dis- ensures timely referral to sup-
In general, screening helps tress have you been experienc- portive services.
identify the risk for having psy- ing in the past week?” opens a Evidence suggests that dis-
chosocial health needs. Needs dialogue with the oncologist or tress screening alone is not suffi-
assessment requires more time navigator and gives permission cient to improve patient out-
than screening and involves a for a discussion of emotions.2 comes. A critical component of
more in-depth evaluation that According to the NCCN a successful distress manage-
confirms the presence of specif- Guidelines®, patients should be ment program is making appro-
ic psychosocial health needs screened during the initial visit priate and timely referrals, and
and describes their nature. Each and then as clinically indicated then following up with patients
yields personalized information throughout treatment. Scores of postreferral to gauge results of
that can be used to develop ≥4 suggest a moderate to se- the experience and provide
strategies to address an individu- vere level of distress. If the pa- feedback as necessary.9 Navi-
al’s psychosocial needs. Provid- tient’s distress is mild (score is gators are instrumental in the
ing this type of emotional sup-VIII. DISTRESS AND PSYCHOSOCIAL NEEDS 25
FIGURE 2. NCCN Distress Therometer
NCCN Distress Thermometer and Problem List for Patients
NCCN DISTRESS THERMOMETER PROBLEM LIST
Instructions: Please circle the number Please indicate if any of the following has been a problem for you in the
(0-10) that best describes how much past week including today.
distress you have been experiencing Be sure to check YES or NO for each
in the past week including today.
YES NO Practical Problems
YES NO Physical Problems
Child care Appearance
Housing Bathing/dressing
Insurance/financial
Breathing
Extreme distress Transportation Changes in urination
10 Work/school Constipation
9 Treatment decisions
Diarrhea
Eating
8 Family Problems
Fatigue
7 Dealing with children
Feeling swollen
Dealing with partner
6 Fevers
Ability to have children
Getting around
5 Family health issues
Indigestion
4 Emotional Problems Memory/concentration
3 Depression Mouth sores
Fears Nausea
2
Nervousness Nose dry/congested
1 Sadness Pain
No distress Worry Sexual
0
Loss of interest in Skin dry/itchy
usual activities Sleep
Spiritual/religious Substance use
concerns Tingling in hands/feet
Other Problems: _____________________________________________________
______________________________________________________________________
Source: Adapted with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Distress Management V.2.2018. © 2018
National Comprehensive Cancer Network, Inc. All rights reserved. The NCCN Guidelines® and illustrations herein may not be reproduced in any form for any
purpose without the express written permission of NCCN. To view the most recent and complete version of the NCCN Guidelines, go online to NCCN.org. The
NCCN Guidelines are a work in progress that may be refined as often as new significant data becomes available.
and families with psychosocial problems with healthcare com- issues. Regular interaction with
services, and coordinating psy- munication. Navigators can navigators allows periodic eval-
chosocial and biomedical care.9 focus on resolving barriers to uation of the success of inter-
Common barriers to physical care, which can be assessed ventions to reduce barriers.
and psychosocial care include during interviews with patients, The supportive role of naviga-
lack of social support, financial and gathering data on psycho- tion in addressing potential con-
and insurance concerns, and social, financial, and practical cerns that extend beyond coor-26 NAVIGATING THE C ANCER CONTINUUM
dination of care and side effect ment utilizing the NCCN Distress On the Distress Thermometer,
management should help to Thermometer. The nurse naviga- Stan reported difficulty with
alleviate issues related to dis- tor instructed Stan on the role of emotional problems in regard to
tress as they arise. Navigators the Distress Thermometer and treatment decisions and feel-
may strengthen physical and encouraged its completion by ings of “sadness,” “fears,” and
psychosocial adjustment to a having him mark problem areas “worry.” In his discussion with the
cancer diagnosis by identifying relevant to his situation. Stan oncology social worker and the
and promoting effective cop- scored an 8 on a scale of 0 to 10 nurse navigator, Stan expressed
ing strategies such as relaxation, on the Distress Thermometer. In concern about his disease and
meditation, counseling, educa- the areas regarding practical its treatment, and the possibility
tion sessions, group social sup- problems, emotional problems, that they may affect his ability
port, or exercise. and physical problems, Stan indi- to care for his family and con-
cated that he was experiencing tribute to loss of “normal life.”
Case Scenario: Patient difficulty and distress. Based on Stan was encouraged to partic-
Distress Stan’s self-reporting (score of 8 ipate in the cancer center’s
Stan is a 44-year-old divorced on the Distress Thermometer), the Coping Skills program, which
father with sole custody of 2 nurse navigator referred him to was facilitated by the oncology
teenaged children. He is self-em- the oncology social worker, who social worker to help patients
ployed as a landscaper to sup- contacted him within 48 hours. with cancer develop skills to
port his family. After a 2- to 3- Stan met with the oncology cope with the emotional and
week history of abdominal pain social worker and the nurse physical impact of cancer.
and rectal bleeding, he was navigator to address the areas Under the physical problems
sent for a colonoscopy. A com- of difficulty he reported on the portion of the Distress Thermom-
plete colonoscopy could not be Distress Thermometer. An analy- eter tool, Stan reported difficulty
performed, as Stan was found sis of the screening revealed with “constipation,” “eating,”
to have a neoplastic mass of concerns with practical, emo- and “fatigue.” He also expressed
the rectum narrowing the lumen tional, and physical problems. concern regarding possible side
to preclude advancement of Stan also reported difficulty with effects of his planned treat-
the scope. An immediate on- insurance/financial issues. As a ment, including neuropathy, di-
cology consultation was ar- self-employed landscaper and arrhea, and neutropenia, and
ranged. Upon meeting with the sole provider for his family, Stan their effect on his livelihood and
medical oncologist, Stan was lacked medical insurance cov- quality of life. The nurse naviga-
sent for a PET scan, which showed erage and expressed concern tor provided education on side
intensive uptake spanning 12 cm regarding his ability to pay med- effect management and re-
of the rectum and uptake within ical bills related to his cancer ferred Stan to the oncology
a perirectal lymph node. treatment. The oncology social nurse practitioner for supportive
Based on the PET scan results, worker and nurse navigator re- care/symptom management
Stan discussed the treatment ferred Stan to the facility’s finan- and to the facility’s dietitian for
recommendations of neoadju- cial counselor, state Medicaid nutritional support.
vant chemoradiation therapy outreach officer, and the local With the use of the NCCN
with continuous infusion of 5-fluo- Social Security Administration Distress Thermometer tool, the
rouracil for 6 weeks, followed by office. The nurse navigator also nurse navigator and oncology
surgical resection, and conclud- referred Stan to the national fi- social worker were able to iden-
ing with adjuvant chemothera- nancial assistance resources of tify Stan’s specific needs and
py. Stan met with the nurse nav- CancerCare® and the Chronic address them accordingly. The
igator for chemotherapy and Disease Fund®, and to the rele- nurse navigator and oncology
radiation therapy education, as vant pharmaceutical drug assis- social worker utilized a multidis-
well as for a psychosocial assess- tance programs. ciplinary approach to addressYou can also read