SAMPLE CHAPTER CHAPTER 16: LIVER, BILIARY TRACT, & PANCREAS DISORDERS - MCGRAW HILL
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Sample Chapter
CHAPTER 16:
Liver, Biliary Tract, &
Pancreas Disorders
BUY NOW
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.CMDT 2022 677
16
Liver, Biliary Tract, &
Pancreas Disorders
Lawrence S. Friedman, MD
JAUNDICE & EVALUATION OF ABNORMAL hepatic uptake of bilirubin due to certain drugs; or impaired
LIVER BIOCHEMICAL TESTS conjugation of bilirubin by glucuronide, as in Gilbert syn-
drome, due to mild decreases in uridine diphosphate
(UDP) glucuronyl transferase, or Crigler-Najjar syndrome,
ESSENTIALS OF DIAGNOSIS caused by moderate decreases (type II) or absence (type I)
of UDP glucuronyl transferase. Hemolysis alone rarely
elevates the serum bilirubin level to more than 7 mg/dL
» Jaundice results from accumulation of bilirubin in (119.7 mcmol/L). Predominantly conjugated hyperbiliru-
body tissues; the cause may be hepatic or binemia may result from impaired excretion of bilirubin
nonhepatic. from the liver due to hepatocellular disease, drugs, sepsis,
» Hyperbilirubinemia may be due to abnormalities or hereditary hepatocanalicular transport defects (such as
in the formation, transport, metabolism, or excre- Dubin-Johnson syndrome, progressive familial intrahe-
tion of bilirubin. patic cholestasis syndromes, and intrahepatic cholestasis of
» Persistent mild elevations of the aminotransferase pregnancy) or from extrahepatic biliary obstruction. Fea-
levels are common in clinical practice and caused tures of some hyperbilirubinemic syndromes are summa-
most often by nonalcoholic fatty liver disease rized in Table 16–2. The term “cholestasis” denotes
(NAFLD). retention of bile in the liver, and the term “cholestatic
»
jaundice” is often used when conjugated hyperbilirubine-
Evaluation of obstructive jaundice begins with
mia results from impaired bile formation or flow. Media-
ultrasonography and is usually followed by
tors of pruritus due to cholestasis have been identified to be
cholangiography.
lysophosphatidic acid and autotaxin, the enzyme that
forms lysophosphatidic acid.
» General Considerations » Clinical Findings
Jaundice (icterus) results from the accumulation of A. Unconjugated Hyperbilirubinemia
bilirubin—a product of heme metabolism—in body tissues. Stool and urine color are normal, and there is mild jaun-
Hyperbilirubinemia may be due to abnormalities in the dice and indirect (unconjugated) hyperbilirubinemia with
formation, transport, metabolism, or excretion of bilirubin. no bilirubin in the urine. Splenomegaly occurs in all hemo-
Total serum bilirubin is normally 0.2–1.2 mg/dL (3.42– lytic disorders except in sickle cell disease.
20.52 mcmol/L). Mean levels are higher in men than
women, higher in Whites and Hispanics than Blacks, and
B. Conjugated Hyperbilirubinemia
correlate with an increased risk of symptomatic gallstone
disease and inversely with the risk of stroke, respiratory Cholestasis is often accompanied by pruritus, light-colored
disease, cardiovascular disease, and mortality, presumably stools, and jaundice, although the patient may be asymp-
because of antioxidant and intestinal anti-inflammatory tomatic. Malaise, anorexia, low-grade fever, and right
effects. Jaundice may not be recognizable until serum bili- upper quadrant discomfort are frequent with hepatocellu-
rubin levels are about 3 mg/dL (51.3 mcmol/L). lar disease. Dark urine, jaundice, and, in women, amenor-
Jaundice may be caused by predominantly unconju- rhea occur. An enlarged tender liver, spider telangiectasias,
gated or conjugated bilirubin in the serum (Table 16–1). palmar erythema, ascites, gynecomastia, sparse body hair,
Unconjugated hyperbilirubinemia may result from over- fetor hepaticus, and asterixis may be present, depending on
production of bilirubin because of hemolysis; impaired the cause, severity, and chronicity of liver dysfunction.
BUY NOW
CMDT22_Ch16_p0677-p0740.indd 677 29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.678 CMDT 2022 Chapter 16
Table 16–1. Classification of jaundice.
type of hyperbilirubinemia Location and Cause
Unconjugated hyperbilirubinemia Increased bilirubin production (eg, hemolytic anemias, hemolytic reactions, hematoma, pulmonary
(predominantly indirect bilirubin) infarction)
Impaired bilirubin uptake and storage (eg, posthepatitis hyperbilirubinemia, Gilbert syndrome,
Crigler-Najjar syndrome, drug reactions)
Conjugated hyperbilirubinemia hereditary Cholestatic Syndromes (see also Table 16–2)
(predominantly direct bilirubin) Faulty excretion of bilirubin conjugates (eg, Dubin-Johnson syndrome, Rotor syndrome) or mutation
in genes coding for bile salt transport proteins (eg, progressive familial intrahepatic cholestasis
syndromes, benign recurrent intrahepatic cholestasis, and some cases of intrahepatic cholestasis
of pregnancy)
hepatocellular Dysfunction
Biliary epithelial and hepatocyte damage (eg, hepatitis, hepatic cirrhosis)
Intrahepatic cholestasis (eg, certain drugs, biliary cirrhosis, sepsis, postoperative jaundice)
Hepatocellular damage or intrahepatic cholestasis resulting from miscellaneous causes (eg, spiro-
chetal infections, infectious mononucleosis, cholangitis, sarcoidosis, lymphomas, hyperthyroidism,
industrial toxins)
Biliary Obstruction
Choledocholithiasis, biliary atresia, carcinoma of biliary duct, sclerosing cholangitis, IgG4-related
cholangitis, ischemic cholangiopathy, choledochal cyst, external pressure on bile duct, pancreati-
tis, pancreatic neoplasms
Ig, immunoglobulin.
C. Biliary Obstruction expectancy. Truncal fat and early-onset paternal obesity are
risk factors for increased ALT levels. Levels are mildly elevated
There may be right upper quadrant pain, weight loss (sug- in more than 25% of persons with untreated celiac disease and
gesting carcinoma), jaundice, pruritus, dark urine, and in type 1 diabetic patients with so-called glycogenic hepatopa-
light-colored stools. Symptoms and signs may be intermit- thy and often rise transiently in healthy persons who begin
tent if caused by a stone, carcinoma of the ampulla, or taking 4 g of acetaminophen per day or experience rapid
cholangiocarcinoma. Pain may be absent early in pancre- weight gain on a fast-food diet. Levels may rise strikingly but
atic cancer. Occult blood in the stools suggests cancer of transiently in patients with acute biliary obstruction from
the ampulla. A palpable gallbladder (Courvoisier sign) is choledocholithiasis. NAFLD is by far the most common cause
characteristic, but neither specific nor sensitive, of a pan- of persistent mildly to moderately elevated aminotransferase
creatic head tumor. Fever and chills are more common in levels. Elevated ALT and AST levels, often greater than
benign obstruction with associated cholangitis. 1000 units/L (20 mckat/L), are the hallmark of hepatocellular
» Diagnostic Studies
necrosis or inflammation. Modest elevations are frequent in
systemic infections, including coronavirus disease 2019
(See Tables 16–3 and 16–4.) (COVID-19). The differential diagnosis of any liver test eleva-
tion always includes toxicity caused by drugs, herbal and
A. Laboratory Findings dietary supplements, and toxins.
Elevated alkaline phosphatase levels are seen in cho-
Elevated serum alanine and aspartate aminotransferase lestasis or infiltrative liver disease (such as tumor, granulo-
(ALT and AST) levels reflect hepatocellular injury. Normal matous disease, or amyloidosis). Isolated alkaline
reference values for ALT and AST are lower than generally phosphatase elevations of hepatic rather than bone, intesti-
reported when persons with risk factors for fatty liver are nal, or placental origin are confirmed by concomitant ele-
excluded. The upper limit of normal for ALT is vation of gamma-glutamyl transpeptidase or 5′-nucleotidase
29–33 units/L in men and 19–25 units/L in women. Levels levels. Serum gamma-glutamyl transpeptidase levels
decrease with age and correlate with body mass index and appear to correlate with the risk of mortality and disability
mortality from liver disease and inversely with caffeine in the general population.
consumption and physical activity. There is controversy
about whether a persistently elevated ALT level is associ-
B. Imaging
ated with a low or high vitamin D level and, in the general
population, with mortality from coronary artery disease, Demonstration of dilated bile ducts by ultrasonography or
cancer, diabetes mellitus, and all causes; elevated AST lev- CT indicates biliary obstruction (90–95% sensitivity).
els have been reported to be associated with shorter life Ultrasonography, CT, and MRI may also demonstrate
CMDT22_Ch16_p0677-p0740.indd 678 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.LIVer, BILIarY traCt, & paNCreaS DISOrDerS CMDT 2022 679
Table 16–2. Hyperbilirubinemic disorders.
type of
Nature of Defect hyperbilirubinemia Clinical and pathologic Characteristics
Gilbert syndrome1 Reduced activity of Unconjugated Benign, asymptomatic hereditary jaundice. Hyperbilirubinemia
uridine diphosphate (indirect) bilirubin increased by 24- to 36-hour fast. No treatment required. Asso-
glucuronyl transferase ciated with reduced mortality from cardiovascular disease.
Dubin-Johnson Reduced excretory Conjugated (direct) Benign, asymptomatic hereditary jaundice. Gallbladder does
syndrome2 function of bilirubin not visualize on oral cholecystography. Liver darkly pig-
hepatocytes mented on gross examination. Biopsy shows centrilobular
brown pigment. Prognosis excellent.
Rotor syndrome3 Reduced hepatic reuptake Conjugated (direct) Similar to Dubin-Johnson syndrome, but liver is not pigmented
of bilirubin conjugates bilirubin and the gallbladder is visualized on oral cholecystography.
Prognosis excellent.
Recurrent or Cholestasis, often on a Predominantly Episodic attacks of or progressive jaundice, itching, and malaise.
progressive familial basis conjugated (direct) Onset in early life and may persist for a lifetime. Alkaline
intrahepatic bilirubin phosphatase increased. Cholestasis found on liver biopsy.
cholestasis4 (Biopsy may be normal during remission.) Prognosis is gener-
ally excellent for “benign” recurrent intrahepatic cholestasis
but may not be for familial forms.
Intrahepatic Cholestasis Predominantly Benign cholestatic jaundice, usually occurring in the third trimester
cholestasis of conjugated (direct) of pregnancy. Itching, gastrointestinal symptoms, and abnormal
pregnancy5 bilirubin liver excretory function tests. Cholestasis noted on liver biopsy.
Prognosis excellent, but recurrence with subsequent pregnan-
cies or use of oral contraceptives is characteristic.
1
Gilbert syndrome generally results from the addition of extra dinucleotide(s) TA sequences to the TATA promoter of the conjugating
enzyme UGT1A1.
2
Dubin-Johnson syndrome is caused by a mutation in the ABCC2 gene coding for organic anion transporter multidrug resistance protein 2
in bile canaliculi on chromosome 10q24.
3
Rotor syndrome is caused by mutations in the genes coding for organic anion transporting polypeptides OATP1B1 and OATP1B3 on chro-
mosome 12p.
4
Mutations in genes that control hepatocellular transport systems that are involved in the formation of bile and inherited as autosomal
recessive traits are on chromosomes 18q21–22, 2q24, 7q21, and others in families with progressive familial intrahepatic cholestasis. Gene
mutations on chromosome 18q21–22 alter a P-type ATPase expressed in the small intestine and liver and on chromosome 2q24 alter the
bile acid export pump and also cause benign recurrent intrahepatic cholestasis. Mutations in the ABCB4 gene on chromosome 7 that
encodes multidrug resistance protein 3 account for progressive familial intrahepatic cholestasis type 3. Less common causes of progressive
familial intrahepatic cholestasis are mutations in genes that encode TJP2, FXR, and MY05B.
5
Mutations in genes (especially ABCB4 and ABCB11) that encode biliary canalicular transporters account for many cases of intrahepatic
cholestasis of pregnancy.
Table 16–3. Liver biochemical tests: normal values and changes in hepatocellular and obstructive jaundice.
tests Normal Values hepatocellular Jaundice Obstructive Jaundice
Bilirubin1
Direct 0.1–0.3 mg/dL (1.71–5.13 mcmol/L) Increased Increased
Indirect 0.2–0.7 mg/dL (3.42–11.97 mcmol/L) Increased Increased
Urine bilirubin None Increased Increased
Serum albumin 3.5–5.5 g/dL (35–55 g/L) Decreased Generally unchanged
Alkaline phosphatase 30–115 units/L (0.6–2.3 mkat/L) Mildly increased (+) Markedly increased (++++)
Prothrombin time INR of 1.0–1.4. After vitamin K, 10% Prolonged if damage is severe; Prolonged if obstruction is
decrease in 24 hours does not respond to marked; generally responds to
parenteral vitamin K parenteral vitamin K
ALT, AST ALT, ≤ 30 units/L (0.6 mkat/L) (men), Increased, as in viral hepatitis Minimally increased
≤ 19 units/L (0.38 mkat/L) (women);
AST, 5–40 units/L (0.1–0.8 mkat/L)
1
Measured by the van den Bergh reaction, which overestimates direct bilirubin in normal persons.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; INR, international normalized ratio.
CMDT22_Ch16_p0677-p0740.indd 679
BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.680 CMDT 2022 Chapter 16
stones, strictures, and dilatation; however, it is less reliable
Table 16–4. Causes of serum aminotransferase than endoscopic retrograde cholangiopancreatography
elevations.1 (ERCP) for distinguishing malignant from benign stric-
tures. ERCP requires a skilled endoscopist and may be used
Mild elevations Severe elevations
to demonstrate pancreatic or ampullary causes of jaundice,
(< 5 × normal) (> 15 × normal)
carry out sphincterotomy and stone extraction, insert a
Hepatic: ALT-predominant Acute viral hepatitis stent through an obstructing lesion, or facilitate direct
Chronic hepatitis B, C, and D (A–E, herpes) cholangiopancreatoscopy. Complications of ERCP include
Acute viral hepatitis (A-E, EBV, CMV) Medications/toxins pancreatitis (5% or less) and, less commonly, cholangitis,
Steatosis/steatohepatitis Ischemic hepatitis bleeding, or duodenal perforation after sphincterotomy.
Hemochromatosis Autoimmune hepatitis
Risk factors for post-ERCP pancreatitis include female sex,
Medications/toxins Wilson disease
Autoimmune hepatitis Acute bile duct pregnancy, prior post-ERCP pancreatitis, suspected
Alpha-1-antitrypsin obstruction sphincter of Oddi dysfunction, and a difficult or failed can-
(alpha-1-antiprotease) deficiency Acute Budd-Chiari nulation. Percutaneous transhepatic cholangiography
Wilson disease syndrome (PTC) is an alternative approach to evaluating the anatomy
Celiac disease Hepatic artery ligation of the biliary tract. Serious complications of PTC occur in
Glycogenic hepatopathy 3% and include fever, bacteremia, bile peritonitis, and
Hepatic: AST-predominant intraperitoneal hemorrhage. Endoscopic ultrasonography
Alcohol-related liver injury (EUS) is the most sensitive test for detecting small lesions
(AST:ALT > 2:1)
of the ampulla or pancreatic head and for detecting portal
Cirrhosis
Nonhepatic
vein invasion by pancreatic cancer. It is also accurate for
Strenuous exercise detecting or excluding bile duct stones.
Hemolysis
Myopathy C. Liver Biopsy
Thyroid disease
Macro-AST
Percutaneous liver biopsy is considered the definitive
study for determining the cause and histologic severity of
1
Almost any liver disease can cause moderate aminotransferase hepatocellular dysfunction or infiltrative liver disease,
elevations (5–15 × normal). although it is subject to sampling error. It is generally
ALT, alanine aminotransferase; AST, aspartate aminotransferase; performed under ultrasound or, in some patients with
CMV, cytomegalovirus; EBV, Epstein-Barr virus. suspected metastatic disease or a hepatic mass, CT guid-
Adapted, with permission, from Green RM et al. AGA technical ance. A transjugular route can be used in patients with
review on the evaluation of liver chemistry tests. Gastroenterology. coagulopathy or ascites, and in selected cases endoscopic
2002 Oct;123(4):1367–84. Copyright © Elsevier.
ultrasound-guided liver biopsy has proved advantageous.
The risk of bleeding after a percutaneous liver biopsy is
approximately 0.6% and is increased in persons with a
hepatomegaly, intrahepatic tumors, and portal hyperten- platelet count of 50,000/mcL (50 × 109/mcL) or less. The
sion. Use of color Doppler ultrasonography or contrast risk of death is less than 0.1%. Panels of blood tests (eg,
agents that produce microbubbles increases the sensitivity of FibroSure, NAFLD fibrosis score, enhanced liver fibrosis
transcutaneous ultrasonography for detecting small neo- score) and, more accurately, elastography (vibration-
plasms. MRI is the most accurate technique for identifying controlled transient, shear wave, acoustic radiation force
isolated liver lesions such as hemangiomas, focal nodular impulse, or magnetic resonance elastography) to measure
hyperplasia, or focal fatty infiltration and for detecting liver stiffness are used for estimating the stage of liver
hepatic iron overload. The most sensitive techniques for fibrosis and degree of portal hypertension without the
detection of individual small hepatic metastases in patients need for liver biopsy; they are most useful for excluding
eligible for resection are multiphasic helical or multislice CT; advanced fibrosis.
MRI with use of gadolinium or ferumoxides as contrast
agents; CT arterial portography, in which imaging follows » When to Refer
intravenous contrast infusion via a catheter placed in the
superior mesenteric artery; and intraoperative ultrasonogra- Patients with jaundice should be referred for diagnostic
phy. Dynamic gadolinium-enhanced MRI and MRI follow- procedures.
» When to Admit
ing administration of superparamagnetic iron oxide show
promise in visualizing hepatic fibrosis. Because of its much
lower cost, ultrasonography is preferable to CT (~six times Patients with liver failure should be hospitalized.
more expensive) or MRI (~seven times more expensive) as a
screening test for hepatocellular carcinoma in persons with Fix OK et al. Clinical best practice advice for hepatology and
cirrhosis. Positron emission tomography (PET) can be used liver transplant providers during the COVID-19 pandemic:
to detect small pancreatic tumors and metastases. Ultraso- AASLD Expert Panel Consensus Statement. Hepatology.
nography can detect gallstones with a sensitivity of 95%. 2020;72:287. [PMID: 32298473]
Magnetic resonance cholangiopancreatography (MRCP) Loomba R et al. Advances in non-invasive assessment of hepatic
fibrosis. Gut. 2020;69:1343. [PMID: 32066623]
is a sensitive, noninvasive method of detecting bile duct
CMDT22_Ch16_p0677-p0740.indd 680
BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.LIVer, BILIarY traCt, & paNCreaS DISOrDerS CMDT 2022 681
The incubation period averages 30 days. HAV is
Neuberger J et al. Guidelines on the use of liver biopsy in clinical
practice from the British Society of Gastroenterology, the excreted in feces for up to 2 weeks before clinical illness but
Royal College of Radiologists and the Royal College of rarely after the first week of illness. The mortality rate for
Pathology. Gut. 2020;69:1382. [PMID: 32467090] hepatitis A is low, and acute liver failure due to hepatitis A
is uncommon except for rare instances in which it occurs
in a patient with concomitant chronic hepatitis C. There is
º
DISeaSeS OF the LIVer no chronic carrier state. In the United States, about 30% of
the population have serologic evidence of previous HAV
See Chapter 39 for Hepatocellular Carcinoma.
infection.
ACUTE HEPATITIS A » Clinical Findings
A. Symptoms and Signs
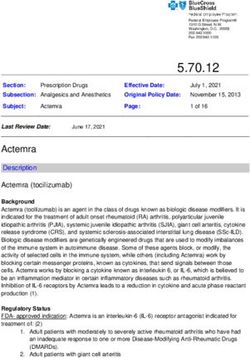
ESSENTIALS OF DIAGNOSIS Figure 16–1 shows the typical course of acute hepatitis A.
Clinical illness is more severe in adults than in children, in
» Prodrome of anorexia, nausea, vomiting, malaise, whom it is usually asymptomatic. The onset may be abrupt
aversion to smoking. or insidious, with malaise, myalgia, arthralgia, easy fatiga-
» Fever, enlarged and tender liver, jaundice. bility, upper respiratory symptoms, and anorexia. A dis-
»
taste for smoking, paralleling anorexia, may occur early.
Normal to low white cell count; markedly elevated
Nausea and vomiting are frequent, and diarrhea or consti-
aminotransferases.
pation may occur. Fever is generally present but is low-
grade except in occasional cases in which systemic toxicity
» General Considerations
may occur. Defervescence and a fall in pulse rate often
coincide with the onset of jaundice.
Hepatitis can be caused by viruses, including the five hepa- Abdominal pain is usually mild and constant in the
totropic viruses—A, B, C, D, and E—and many drugs and right upper quadrant or epigastrium, often aggravated by
toxic agents; the clinical manifestations may be similar jarring or exertion, and rarely may be severe enough to
regardless of cause. Hepatitis A virus (HAV) is a 27-nm simulate cholecystitis. Jaundice occurs after 5–10 days but
RNA hepatovirus (in the picornavirus family) that causes may appear at the same time as the initial symptoms. In
epidemics or sporadic cases of hepatitis. HAV infection is many patients, jaundice never develops. With the onset of
hyperendemic in developing countries. Globally, 15 million jaundice, prodromal symptoms often worsen, followed by
people are infected with HAV annually. The virus is trans- progressive clinical improvement. Stools may be acholic
mitted by the fecal-oral route by either person-to-person
contact or ingestion of contaminated food or water, and its
spread is favored by crowding and poor sanitation. Since Jaundice
introduction of the HAV vaccine in the United States in Symptoms
1995, the incidence rate of HAV infection has declined
↑ ALT
from as much as 14 to 0.4 per 100,000 population, with a
corresponding decline in the mortality rate from 0.1 to 0.02 HAV in serum
death per 100,000 population and an increase in the mean
age of infection and death. Nevertheless, over 80% of per-
Titer
sons aged 20–60 years in the United States are still suscep-
tible to HAV, and vulnerable populations are especially at
risk. The highest incidence rate (2.1 per 100,000) is in
adults aged 30–39. Common source outbreaks resulting
from contaminated food, including inadequately cooked
shellfish, or untreated ground water from wells continue to
occur, although no drinking water–associated outbreaks
have occurred in the United States since 2009. In 2017, an 0 4 8 12 16 20
outbreak beginning in California and extending to 33 other
Weeks after exposure
states affected a large number of homeless persons and
Fecal IgM IgG
resulted in many deaths. Outbreaks among people who
HAV anti-HAV anti-HAV
inject drugs or who are unvaccinated residents in institu-
tions and cases among international adoptees and their ▲ Figure 16–1. The typical course of acute type A
contacts also occur. In the United States, international hepatitis. (HAV, hepatitis A virus; anti-HAV, antibody to
travel emerged as an important risk factor, accounting for hepatitis A virus; ALT, alanine aminotransferase.)
over 40% of cases in the early 2000s but a lower percentage (Reprinted, with permission, from Koff RS. Acute viral
in the 2010s. Overall, however, reports of HAV infection hepatitis. In: Friedman LS, Keeffe EB [editors]. Handbook of
increased by nearly 300% during 2016–2018 compared to Liver Disease, 4th ed. Philadelphia: Saunders Elsevier, 2018.
2013–2015. Copyright © Elsevier.)
CMDT22_Ch16_p0677-p0740.indd 681 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.682 CMDT 2022 Chapter 16
during this phase. Hepatomegaly—rarely marked—is » Prevention
present in over half of cases. Liver tenderness is usually
present. Splenomegaly is reported in 15% of patients, and Strict isolation of patients is not necessary, but hand wash-
soft, enlarged lymph nodes—especially in the cervical or ing after bowel movements is required. Unvaccinated per-
epitrochlear areas—may be noted. sons who are exposed to HAV are advised to receive
The acute illness usually subsides over 2–3 weeks with postexposure prophylaxis with a single dose of HAV vac-
complete clinical and laboratory recovery by 9 weeks. In cine or immune globulin (0.01 mL/kg), or both, within
some cases, clinical, biochemical, and serologic recovery 2 weeks of exposure. The vaccine is preferred in healthy
may be followed by one or two relapses, but recovery is the persons aged 1 year to 40 years, whereas immune globulin
rule. Acute cholecystitis occasionally complicates the and the vaccine is preferred in those who are younger than
course of acute hepatitis A. Other occasional extrahepatic 1 year or older than 40 years, are immunocompromised, or
complications include acute kidney injury, arthritis, vascu- have chronic liver disease.
litis, acute pancreatitis, aplastic anemia, and a variety of Vaccination with one of two effective inactivated hepatitis
neurologic manifestations. A vaccines available in the United States provides long-term
immunity and is recommended for persons living in or trav-
eling to endemic areas (including military personnel), per-
B. Laboratory Findings
sons over age 40, patients with chronic liver disease upon
The white blood cell count is normal to low, especially in diagnosis after prescreening for immunity (although the
the preicteric phase. Large atypical lymphocytes may occa- cost-effectiveness of vaccinating all patients with concomi-
sionally be seen. Mild proteinuria is common, and bilirubi- tant chronic hepatitis C has been questioned), men who have
nuria often precedes the appearance of jaundice. Strikingly sex with men, persons with HIV infection, animal handlers,
elevated ALT or AST levels occur early, followed by eleva- persons who use injection or noninjection drugs, persons
tions of bilirubin and alkaline phosphatase; in a minority of experiencing homelessness, persons who are incarcerated,
patients, the latter persist after aminotransferase levels close personal contacts of international adoptees, persons
have normalized. Cholestasis is occasionally marked. Anti- living in group settings for those with developmental disabili-
body to hepatitis A (anti-HAV) appears early in the course ties, and persons who request protection against HAV. For
of the illness (Figure 16–1). Both IgM and IgG anti-HAV healthy travelers, a single dose of vaccine at any time before
are detectable in serum soon after the onset. Peak titers of departure can provide adequate protection. Routine vaccina-
IgM anti-HAV occur during the first week of clinical dis- tion is advised by the Advisory Committee on Immunization
ease and usually disappear within 3–6 months. Detection Practices of the Centers for Disease Control and Prevention
of IgM anti-HAV is an excellent test for diagnosing acute (CDC) in all children aged 12–23 months in the United
hepatitis A but is not recommended for the evaluation of States, with catch-up vaccination for children and adoles-
asymptomatic persons with persistently elevated serum cents aged 2–18 years who have not previously received the
aminotransferase levels because false-positive results occur. HAV vaccine. HAV vaccine is also effective in the prevention
False-negative results have been described in a patient of secondary spread to household contacts of primary cases.
receiving rituximab for rheumatoid arthritis. Titers of IgG The recommended dose for adults is 1 mL (1440 ELISA
anti-HAV rise after 1 month of the disease and may persist units) of Havrix (GlaxoSmithKline) or 1 mL (50 units) of
for years. IgG anti-HAV (in the absence of IgM anti-HAV) Vaqta (Merck) intramuscularly, followed by a booster dose at
indicates previous exposure to HAV, noninfectivity, and 6–18 months. A combined hepatitis A and B vaccine
immunity. (Twinrix, GlaxoSmithKline) is available. HIV infection
impairs the response to the HAV vaccine, especially in
» Differential Diagnosis persons with a CD4 count less than 200/mcL (0.2 × 109/L).
» Treatment
The differential diagnosis includes other viruses that cause
hepatitis, particularly hepatitis B and C, and diseases such
as infectious mononucleosis, cytomegalovirus infection, Bed rest is recommended only if symptoms are marked. If
herpes simplex virus infection, Middle East respiratory nausea and vomiting are pronounced or if oral intake is sub-
syndrome, and infections caused by many other viruses, stantially decreased, intravenous 10% glucose is indicated.
including influenza, Ebola virus, and SARS-CoV-2; spiro- Dietary management consists of palatable meals as tol-
chetal diseases such as leptospirosis and secondary syphi- erated, without overfeeding; breakfast is usually tolerated
lis; brucellosis; rickettsial diseases such as Q fever; best. Strenuous physical exertion, alcohol, and hepatotoxic
drug-induced liver injury; and ischemic hepatitis (shock agents should be avoided. Small doses of oxazepam are safe
liver). Occasionally, autoimmune hepatitis may have an because metabolism is not hepatic; morphine sulfate
acute onset mimicking acute viral hepatitis. Rarely, meta- should be avoided.
static cancer of the liver, lymphoma, or leukemia may pres- Corticosteroids have no benefit in patients with viral
ent as a hepatitis-like picture. hepatitis, including those with acute liver failure.
The prodromal phase of viral hepatitis must be distin-
guished from other infectious disease such as influenza
and COVID-19, upper respiratory infections, and the pro-
» Prognosis
dromal stages of the exanthematous diseases. Cholestasis In most patients, clinical recovery is generally complete
may mimic obstructive jaundice. within 3 months. Laboratory evidence of liver dysfunction
CMDT22_Ch16_p0677-p0740.indd 682 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.LIVer, BILIarY traCt, & paNCreaS DISOrDerS CMDT 2022 683
may persist for a longer period, but most patients recover transmission. Other groups at risk include patients and
completely. Hepatitis A does not cause chronic liver dis- staff at hemodialysis centers, physicians, dentists, nurses,
ease, although it may persist for up to 1 year, and clinical and personnel working in clinical and pathology labora-
and biochemical relapses may occur before full recovery. tories and blood banks. Half of all patients with acute
The mortality rate is less than 1.0%, with a higher rate in hepatitis B in the United States have previously been
older adults than in younger persons. incarcerated or treated for a sexually transmitted disease.
The risk of HBV infection from a blood transfusion in the
» When to Admit United States is no higher than 1 in 350,000 units trans-
fused. Screening for HBV infection is recommended for
• Encephalopathy is present. high-risk groups by the US Preventive Services Task
• International normalized ratio (INR) greater than 1.6. Force.
• The patient is unable to maintain hydration. The incubation period of hepatitis B is 6 weeks to
6 months (average 12–14 weeks). The onset of hepatitis B
is more insidious, and the aminotransferase levels are
Desai AN et al. Management of hepatitis A in 2020–2021. JAMA. higher on average, than in HAV infection. Acute liver fail-
2020;324:383. [PMID: 32628251] ure occurs in less than 1%, with a mortality rate of up to
Freedman M et al. Recommended adult immunization schedule,
United States, 2020. Ann Intern Med. 2020;172:337. [PMID: 60%. Following acute hepatitis B, HBV infection persists in
32016359] 1–2% of immunocompetent adults, but in a higher per-
Nelson NP et al. Prevention of hepatitis A virus infection in the centage of children and immunocompromised adults.
United States: recommendations of the Advisory Committee There are an estimated 1.59 (range, 1.25–2.49) million
on Immunization Practices, 2020. MMWR Recomm Rep. persons (including an estimated 1.32 million foreign-born
2020;69:1. [PMID: 32614811] persons from endemic areas) with chronic hepatitis B in
the United States and 248 million worldwide. Compared
ACUTE HEPATITIS B with the general population, the prevalence of chronic
HBV infection is increased 2- to 3-fold in non-Hispanic
Blacks and 10-fold in Asians. Persons with chronic
ESSENTIALS OF DIAGNOSIS hepatitis B, particularly when HBV infection is acquired
early in life and viral replication persists, are at substantial
»
risk for cirrhosis and hepatocellular carcinoma (up to
Prodrome of anorexia, nausea, vomiting, malaise,
25–40%); men are at greater risk than women.
aversion to smoking.
» Clinical Findings
» Fever, enlarged and tender liver, jaundice.
» Normal to low white blood cell count; markedly
elevated aminotransferases early in the course. A. Symptoms and Signs
» Liver biopsy shows hepatocellular necrosis and The clinical picture of viral hepatitis is extremely variable,
mononuclear infiltrate but is rarely indicated. ranging from asymptomatic infection without jaundice to
acute liver failure and death in a few days to weeks.
Figure 16–2 shows the typical course of acute HBV infec-
» General Considerations tion. The onset may be abrupt or insidious, and the clinical
features are similar to those for acute hepatitis A. Serum
Hepatitis B virus (HBV) is a 42-nm hepadnavirus with a sickness may be seen early in acute hepatitis B. Fever is
partially double-stranded DNA genome, inner core protein generally present and is low-grade. Defervescence and a
(hepatitis B core antigen, HBcAg), and outer surface coat fall in pulse rate often coincide with the onset of jaundice.
(hepatitis B surface antigen, HBsAg). There are 10 different Infection caused by HBV may be associated with glomeru-
genotypes (A–J), which may influence the course of infec- lonephritis and polyarteritis nodosa.
tion and responsiveness to antiviral therapy. HBV is usually The acute illness usually subsides over 2–3 weeks with
transmitted by inoculation of infected blood or blood complete clinical and laboratory recovery by 16 weeks. In
products or by sexual contact and it is present in saliva, 5–10% of cases, the course may be more protracted, but
semen, and vaginal secretions. HBsAg-positive mothers less than 1% will develop acute liver failure. Hepatitis B
may transmit HBV at delivery; the risk of chronic infection may become chronic.
in the infant is as high as 90%.
Since 1990, the incidence of HBV infection in the
B. Laboratory Findings
United States has decreased from 8.5 to 1.5 cases per
100,000 population. The prevalence is 0.27% in persons The laboratory features are similar to those for acute
aged 6 or older. Because of universal vaccination since hepatitis A, although serum aminotransferase levels are
1992, exposure to HBV is now very low among persons higher on average in acute hepatitis B, and marked cholesta-
aged 18 or younger. HBV is prevalent in men who have sis is not a feature. Marked prolongation of the prothrombin
sex with men and in people who inject drugs (about 7% time in severe hepatitis correlates with increased mortality.
of HIV-infected persons are coinfected with HBV), but There are several antigens and antibodies as well as
the greatest number of cases result from heterosexual HBV DNA that relate to HBV infection and that are useful
CMDT22_Ch16_p0677-p0740.indd 683 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.684 CMDT 2022 Chapter 16
recovery from HBV infection, noninfectivity, and
Jaundice immunity.
Symptoms
↑ ALT 3. Anti-HBc—IgM anti-HBc appears shortly after HBsAg
HBeAg Anti-HBe is detected. In the setting of acute hepatitis, IgM anti-HBc
HBV DNA indicates a diagnosis of acute hepatitis B, and it fills the
serologic gap in rare patients who have cleared HBsAg
Titer
but do not yet have detectable anti-HBs. IgM anti-HBc
can persist for 3–6 months, and sometimes longer. IgM
anti-HBc may also reappear during flares of previously
inactive chronic hepatitis B. IgG anti-HBc also appears
during acute hepatitis B but persists indefinitely, whether
the patient recovers (with the appearance of anti-HBs in
serum) or chronic hepatitis B develops (with persistence
0 4 8 12 16 18 20 24 28 32 36 40 52
of HBsAg). In asymptomatic blood donors, an isolated
Weeks after exposure
anti-HBc with no other positive HBV serologic results
IgG Anti- IgM
HBsAg may represent a falsely positive result or latent infection
anti-HBc HBs anti-HBc
in which HBV DNA is detectable in serum only by poly-
▲ Figure 16–2. The typical course of acute type B merase chain reaction (PCR) testing.
hepatitis. (anti-HBs, antibody to HBsAg; HBeAg, hepatitis
Be antigen; HBsAg, hepatitis B surface antigen; anti-HBe, 4. HBeAg—HBeAg is a secretory form of HBcAg that
antibody to HBeAg; anti-HBc, antibody to hepatitis B core appears in serum during the incubation period shortly
antigen; ALT, alanine aminotransferase.) (Reprinted, with after the detection of HBsAg. HBeAg indicates viral repli-
permission, from Koff RS. Acute viral hepatitis. In: Friedman cation and infectivity. Persistence of HBeAg beyond
LS, Keeffe EB [editors]. Handbook of Liver Disease, 3rd ed. 3 months indicates an increased likelihood of chronic
Philadelphia: Saunders Elsevier, 2012. Copyright © Elsevier.) hepatitis B. Its disappearance is often followed by the
appearance of anti-HBe, generally signifying diminished
viral replication and decreased infectivity.
in diagnosis. Interpretation of common serologic patterns
is shown in Table 16–5. 5. HBV DNA—The presence of HBV DNA in serum gener-
ally parallels the presence of HBeAg, although HBV DNA
1. HBsAg—The appearance of HBsAg in serum is the first is a more sensitive and precise marker of viral replication
evidence of infection, appearing before biochemical evi- and infectivity. In some patients with chronic hepatitis B,
dence of liver disease, and persisting throughout the clini- HBV DNA is present at high levels without HBeAg in
cal illness. Persistence of HBsAg more than 6 months after serum because of development of a mutation in the core
the acute illness signifies chronic hepatitis B. promoter or precore region of the gene that codes HBcAg;
2. Anti-HBs—Specific antibody to HBsAg (anti-HBs) these mutations prevent synthesis of HBeAg in infected
appears in most individuals after clearance of HBsAg and hepatocytes. When additional mutations in the core gene
after successful vaccination against hepatitis B. Disappear- are also present, the severity of HBV infection is enhanced
ance of HBsAg and the appearance of anti-HBs signal and the risk of cirrhosis is increased.
Table 16–5. Common serologic patterns in hepatitis B virus (HBV) infection and their interpretation.
hBsag anti-hBs anti-hBc hBeag anti-hBe Interpretation
+ – IgM + – Acute hepatitis B
+ – IgG1 + – Chronic hepatitis B with active viral replication
+ – IgG – + Inactive HBV carrier state (low HBV DNA level) or
HBeAg-negative chronic hepatitis B with active viral
replication (high HBV DNA level)
+ + IgG + or – + or – Chronic hepatitis B with heterotypic anti-HBs (about
10% of cases)
– – IgM + or – – Acute hepatitis B
– + IgG – + or – Recovery from hepatitis B (immunity)
– + – – – Vaccination (immunity)
– – IgG – – False-positive; less commonly, infection in remote past
1
Low levels of IgM anti-HBc may also be detected.
CMDT22_Ch16_p0677-p0740.indd 684 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.LIVer, BILIarY traCt, & paNCreaS DISOrDerS CMDT 2022 685
» Differential Diagnosis for adults in 2017. Immunization requires only two injec-
tions, and Heplisav-B appears to be more effective than
The differential diagnosis includes hepatitis A and the previous HBV vaccines. When documentation of serocon-
same disorders listed for the differential diagnosis of acute version is considered desirable, postimmunization anti-
hepatitis A. In addition, coinfection with HDV must be HBs titers may be checked. Protection appears to be
considered. excellent even if the titer wanes—persisting for at least
» Prevention
20 years—and booster reimmunization is not routinely
recommended but is advised for immunocompromised
Strict isolation of patients is not necessary. Thorough hand persons in whom anti-HBs titers fall below 10 milli-
washing by medical staff who may contact contaminated international units/mL. For vaccine nonresponders, three
utensils, bedding, or clothing is essential. Medical staff additional vaccine doses may elicit seroprotective anti-HBs
should handle disposable needles carefully and not recap levels in 30–50% of persons. Doubling of the standard dose
them. Screening of donated blood for HBsAg, anti-HBc, and may also be effective. Universal vaccination of neonates in
anti-HCV has reduced the risk of transfusion-associated countries endemic for HBV has reduced the incidence of
hepatitis markedly. All pregnant women should undergo test- hepatocellular carcinoma. Incomplete immunization is the
ing for HBsAg. HBV-infected persons should practice safe most important predictor of liver disease among vaccinees.
sex. Immunoprophylaxis of the neonate reduces the risk of Unfortunately, approximately 64 million high-risk adults in
perinatal transmission of HBV infection; when the mother’s the United States remain susceptible to HBV.
» Treatment
serum HBV DNA level is 200,000 international units/mL or
higher (or the mother’s serum HBsAg level is above 4–4.5 log10
international units/mL), antiviral treatment of the mother Treatment of acute hepatitis B is the same as that for acute
should also be initiated in the third trimester (see Chronic hepatitis A. Encephalopathy or severe coagulopathy indi-
Hepatitis B & Chronic Hepatitis D). HBV-infected health cates acute liver failure, and hospitalization at a liver trans-
care workers are not precluded from practicing medicine or plant center is mandatory. Antiviral therapy is generally
dentistry if they follow CDC guidelines. unnecessary in patients with acute hepatitis B but is usually
Hepatitis B immune globulin (HBIG) may be protective— prescribed in cases of acute liver failure caused by HBV as
or may attenuate the severity of illness—if given within well as in spontaneous reactivation of chronic hepatitis B
7 days after exposure (adult dose is 0.06 mL/kg body presenting as acute-on-chronic liver failure (see Acute
weight) followed by initiation of the HBV vaccine series. Liver Failure).
This approach is recommended for unvaccinated persons
exposed to HBsAg-contaminated material via mucous » Prognosis
membranes or through breaks in the skin and for individu-
als who have had sexual contact with a person with HBV In most patients, clinical recovery is complete in
infection (irrespective of the presence or absence of HBeAg 3–6 months. Laboratory evidence of liver dysfunction may
in the source). HBIG is also indicated for newborn infants persist for a longer period, but most patients recover com-
of HBsAg-positive mothers, with initiation of the vaccine pletely. The mortality rate for acute hepatitis B is 0.1–1%
series at the same time, both within 12 hours of birth but is higher with superimposed hepatitis D.
(administered at different injection sites). Chronic hepatitis, characterized by elevated amino-
The CDC recommends HBV vaccination of all infants transferase levels for more than 3–6 months, develops in
and children in the United States and all adults who are at 1–2% of immunocompetent adults with acute hepatitis B,
risk for hepatitis B (including persons under age 60 with but in as many as 90% of infected neonates and infants and
diabetes mellitus) or who request vaccination; the vaccine a substantial proportion of immunocompromised adults.
appears to be underutilized in adults for whom vaccination Ultimately, cirrhosis develops in up to 40% of those with
is recommended. Over 90% of recipients of the vaccine chronic hepatitis B; the risk of cirrhosis is even higher in
mount protective antibody to hepatitis B; immunocompro- HBV-infected patients coinfected with hepatitis C or HIV.
mised persons, including patients receiving dialysis (espe- Patients with cirrhosis are at risk for hepatocellular carci-
cially those with diabetes mellitus), respond poorly (see noma at a rate of 3–5% per year. Even in the absence of
Table 30–7). Reduced response to the vaccine may have a cirrhosis, patients with chronic hepatitis B—particularly
genetic basis in some cases and has also been associated those with active viral replication—are at increased risk for
with age over 40 years and celiac disease. The standard hepatocellular carcinoma.
» When to Refer
regimen for adults is 10–20 mcg (depending on the formu-
lation) repeated again at 1 and 6 months, but alternative
schedules have been approved, including accelerated Refer patients with acute hepatitis who require liver biopsy
schedules of 0, 1, 2, and 12 months and of 0, 7, and 21 days for diagnosis.
plus 12 months. For greatest reliability of absorption, the
deltoid muscle is the preferred site of inoculation. Vaccine » When to Admit
formulations free of the mercury-containing preservative
thimerosal are given to infants under 6 months of age. A • Encephalopathy is present.
newer vaccine, Heplisav-B, which uses a novel immune • INR greater than 1.6.
system–stimulating ingredient, was approved by the FDA • The patient is unable to maintain hydration.
CMDT22_Ch16_p0677-p0740.indd 685 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.686 CMDT 2022 Chapter 16
infection, and HIV coinfection, unprotected receptive anal
Chou R et al. Screening for hepatitis B virus infection in non-
pregnant adolescents and adults: updated evidence report and intercourse with ejaculation, and sex while high on meth-
systematic review for the US Preventive Services Task Force. amphetamine increase the risk of HCV transmission in
JAMA. 2020;324:2423. [PMID: 33320229] men who have sex with men. Transmission via breastfeed-
Hwang JP et al. USPSTF 2020 Hepatitis B Screening Recommen- ing has not been documented. An outbreak of hepatitis C
dation: evidence to broaden screening and strengthen linkage in patients with immune deficiencies has occurred in some
to care. JAMA. 2020;324:2380. [PMID: 33320206] recipients of intravenous immune globulin. Hospital- and
Lim JK et al. Prevalence of chronic hepatitis B virus infection
in the United States. Am J Gastroenterol. 2020;115:1429. outpatient facility–acquired transmission has occurred via
[PMID: 32483003] multidose vials of saline used to flush Portacaths; through
US Preventive Services Task Force; Krist AH et al. Screening for reuse of disposable syringes; through drug “diversion” and
hepatitis B virus infection in adolescents and adults: US Pre- tampering with injectable opioids by an infected health
ventive Services Task Force Recommendation Statement. care worker; through contamination of shared saline,
JAMA. 2020;324:2415. [PMID: 33320230] radiopharmaceutical, and sclerosant vials; via inadequately
US Preventive Services Task Force; Owens DK et al. Screening
for hepatitis B virus infection in pregnant women: US Preven- disinfected endoscopy equipment; and between hospitalized
tive Services Task Force reaffirmation recommendation state- patients on a liver unit. In the developing world, unsafe
ment. JAMA. 2019;322:349. [PMID: 31334800] medical practices lead to a substantial number of cases of
HCV infection. Covert transmission during bloody fisticuffs
has even been reported, and incarceration in prison is a risk
ACUTE HEPATITIS C & OTHER CAUSES OF factor, with a seroprevalence of 26% in the United States and
ACUTE VIRAL HEPATITIS rates as high as 90% in some states. In many patients, the
source of infection is unknown. Coinfection with HCV is
Viruses other than HAV and HBV that can cause hepatitis
found in at least 30% of HIV-infected persons. HIV infec-
are hepatitis C virus (HCV), hepatitis D virus (HDV) (delta
tion leads to an increased risk of acute liver failure and more
agent), and hepatitis E virus (HEV) (an enterically transmit-
rapid progression of chronic hepatitis C to cirrhosis; in addi-
ted hepatitis seen in epidemic form in Asia, the Middle East,
tion, HCV increases the hepatotoxicity of antiretroviral
and North Africa and sporadically in Western countries).
therapy. The number of cases of chronic HCV infections in
Human pegivirus (formerly hepatitis G virus [HGV]) rarely,
the United States is reported to have decreased from
if ever, causes frank hepatitis. A related virus has been
3.2 million in 2001 to 2.3 million in 2013 with a small increase
named human hepegivirus-1. A DNA virus designated the
to 2.4 million between 2013 and 2016, although estimates of at
TT virus (TTV) has been identified in up to 7.5% of blood
least 4.6 million exposed and 3.5 million currently infected
donors and found to be transmitted readily by blood trans-
have also been reported. The incidence of new cases of acute,
fusions, but an association between this virus and liver dis-
symptomatic hepatitis C declined from 1992 to 2005, but an
ease has not been established. A related virus known as
increase was observed in persons aged 15 to 24 after 2002, as
SEN-V has been found in 2% of US blood donors, is trans-
a result of injection drug use, with a 3.8-fold increase in over-
mitted by transfusion, and may account for some cases of
all incidence since 2010. An increase has also been observed
transfusion-associated non-ABCDE hepatitis. In immuno-
in women of reproductive age. Worldwide, 71 million people
compromised and rare immunocompetent persons, cyto-
are infected with HCV, with the highest rates in Central and
megalovirus, Epstein-Barr virus, and herpes simplex virus
East Asia, North Africa, and the Middle East.
should be considered in the differential diagnosis of hepati-
tis. Middle East respiratory syndrome (MERS), severe acute » Clinical Findings
respiratory syndrome (SARS), SARS coronavirus infection
(SARS-CoV-2), Ebola virus infection, and influenza may be A. Symptoms and Signs
associated with elevated serum aminotransferase levels
Figure 16–3 shows the typical course of HCV infection.
(occasionally marked). Unidentified pathogens account for a
The incubation period for hepatitis C averages 6–7 weeks,
small percentage of cases of acute viral hepatitis.
and clinical illness is often mild, usually asymptomatic, and
characterized by waxing and waning aminotransferase
1. hepatitis C elevations and a high rate (greater than 80%) of chronic
hepatitis. Spontaneous clearance of HCV following acute
HCV is a single-stranded RNA virus (hepacivirus) with
infection is more common (64%) in persons with the CC
properties similar to those of flaviviruses. Seven major
genotype of the IFNL3 (IL28B) gene than in those with the
genotypes of HCV have been identified. In the past, HCV
CT or TT genotype (24% and 6%, respectively). In persons
was responsible for over 90% of cases of posttransfusion
with the CC genotype, jaundice is more likely to develop
hepatitis, yet only 4% of cases of hepatitis C were attribut-
during the course of acute hepatitis C. In pregnant patients
able to blood transfusions. Over 50% of cases are transmit-
with chronic hepatitis C, serum aminotransferase levels
ted by injection drug use, and both reinfection and
frequently normalize despite persistence of viremia, only to
superinfection of HCV are common in people who actively
increase again after delivery.
inject drugs. Body piercing, tattoos, and hemodialysis are
risk factors. The risk of sexual and maternal–neonatal
B. Laboratory Findings
transmission is low and may be greatest in a subset of
patients with high circulating levels of HCV RNA. Having Diagnosis of hepatitis C is based on an enzyme immunoas-
multiple sexual partners may increase the risk of HCV say (EIA) that detects antibodies to HCV. Anti-HCV is not
CMDT22_Ch16_p0677-p0740.indd 686 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.LIVer, BILIarY traCt, & paNCreaS DISOrDerS CMDT 2022 687
less than 0.1% [very rare]). Screening of all pregnant women
Jaundice for HCV infection has also been recommended by profes-
sional societies. HCV-infected persons should practice safe
Symptoms sex, but there is little evidence that HCV is spread easily by
Anti-HCV sexual contact or perinatally, and no specific preventive
ALT measures are recommended for persons in a monogamous
relationship or for pregnant women. Because a majority of
cases of HCV infection are acquired by injection drug use,
HCV RNA (PCR) public health officials have recommended avoidance of
shared needles and access to needle exchange programs for
injection drug users. As yet, there is no vaccine for HCV.
Vaccination against HAV (after prescreening for prior
immunity) and HBV is recommended for patients with
0 1 2 3 4 5 6 1 2 3 4 5 6
chronic hepatitis C, just as vaccination against HAV is rec-
ommended for patients with chronic hepatitis B.
Months Years
Time after exposure
» Treatment
▲ Figure 16–3. The typical course of acute and
In the past, treatment of patients with acute hepatitis C
chronic hepatitis C. (ALT, alanine aminotransferase; Anti-
with a peginterferon-based regimen for 6–24 weeks was
HCV, antibody to hepatitis C virus by enzyme immuno-
shown to appreciably decrease the risk of chronic hepatitis
assay; HCV RNA [PCR], hepatitis C viral RNA by
in patients in whom serum HCV RNA levels had failed to
polymerase chain reaction.)
clear spontaneously after 3 months. Oral direct-acting
agents have supplanted interferon-based therapy (see
protective, and in patients with acute or chronic hepatitis, Chronic Viral Hepatitis), and a 6-week course of ledipasvir
its presence in serum generally signifies that HCV is the and sofosbuvir has been shown to prevent chronic hepatitis
cause. Limitations of the EIA include moderate sensitivity in patients with acute genotype-1 hepatitis C. Treatment of
(false-negatives) for the diagnosis of acute hepatitis C early acute hepatitis C may be cost effective.
in the course and low specificity (false-positives) in some
persons with elevated gamma-globulin levels. A diagnosis » Prognosis
of hepatitis C may be confirmed by using an assay for HCV
RNA. Occasional persons are found to have anti-HCV In most patients, clinical recovery is complete in
without HCV RNA in the serum, suggesting recovery from 3–6 months. Laboratory evidence of liver dysfunction may
HCV infection in the past. persist for a longer period. The overall mortality rate is less
than 1%, but the rate is reportedly higher in older people.
» Complications Acute liver failure due to HCV is rare in the United States.
Chronic hepatitis, which progresses very slowly in
HCV is a pathogenic factor in mixed cryoglobulinemia and many cases, develops in as many as 85% of all persons with
membranoproliferative glomerulonephritis and may be acute hepatitis C. Ultimately, cirrhosis develops in up to
related to lichen planus, autoimmune thyroiditis, lympho- 30% of those with chronic hepatitis C; the risk of cirrhosis
cytic sialadenitis, idiopathic pulmonary fibrosis, sporadic and hepatic decompensation is higher in patients coin-
porphyria cutanea tarda, and monoclonal gammopathies. fected with both HCV and HBV or HIV. Patients with cir-
HCV infection confers a 20–30% or more increased risk of rhosis are at risk for hepatocellular carcinoma at a rate of
non-Hodgkin lymphoma, and chronic HCV infection 3–5% per year. Long-term morbidity and mortality in
(especially genotype 1) is associated with an increased risk patients with chronic hepatitis C is lower in Black than in
of end-stage renal disease. Hepatic steatosis is a particular White patients and lowest in those infected with HCV
feature of infection with HCV genotype 3 and may also genotype 2 and highest in those with HCV genotype 3.
occur in patients infected with other HCV genotypes who
have risk factors for fatty liver. On the other hand, chronic
Awan AA et al. Hepatitis C in chronic kidney disease: an over-
HCV infection is associated with a decrease in serum cho-
view of the KDIGO Guideline. Clin Gastroenterol Hepatol.
lesterol and low-density lipoprotein levels. 2020;18:2158. [PMID: 31376491]
» Prevention
Schillie S et al. CDC recommendations for hepatitis C screening
among adults—United States, 2020. MMWR Recomm Rep.
2020;69:1. [PMID: 32271723]
Testing donated blood for HCV has helped reduce the risk of Spearman CW et al. Hepatitis C. Lancet. 2019;394:1451. [PMID:
transfusion-associated hepatitis C from 10% in 1990 to 31631857]
about 1 case per 2 million units in 2011. The US Preventive
Services Task Force recommends that asymptomatic adults
ages 18–79 be screened for HCV infection. The CDC rec-
2. hepatitis D (Delta agent)
ommends HCV screening for all persons over age 18 at least HDV is a defective RNA virus that causes hepatitis only in
once in a lifetime and all pregnant women (in both cases association with HBV infection and specifically only in the
except in settings where the prevalence of HCV infection is presence of HBsAg; it is cleared when the latter is cleared.
CMDT22_Ch16_p0677-p0740.indd 687 BUY NOW
29/06/21 8:39 PM
mhprofessional.com
728129654 – ©2021 McGraw Hill LLC. All Rights Reserved.You can also read