Review The axial spondyloarthritis clinical phenotype in idiopathic hypoparathyroidism: critical review of concept that muscular ...
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Review
The axial spondyloarthritis clinical phenotype in idiopathic
hypoparathyroidism: critical review of concept that muscular
hypercontractility can induce enthesopathy lesions
A.T. Masi1, L.C. Jorgenson2, S. Ilahi3
1
Department of Medicine, University ABSTRACT contractility may predispose to axial
of Illinois College of Medicine at Idiopathic hypoparathyroidism (iH- radiographic enthesopathy lesions and
Peoria (UICOMP), Peoria, IL, USA; PoPT) is a rare condition infrequently contribute knowledge on biomechanical
2
Transitional Resident, University
associated with axial spondyloarthri- contributions and pathways for further
of Illinois College of Medicine at
Peoria (UICOMP), Peoria, IL, USA; tis (SpA) which may mimic ankylosing research.
3
Family Medicine Resident, Niagara spondylitis (AS). Axial SpA is a unifying
Falls Memorial Medical Center, clinical term for chronic inflammatory Introduction
Niagara Falls, NY, USA. spinal disorders, although biomechani- Parathyroid diseases are associated
Alfonse T. Masi, MD, DR.PH cal factors may play a role. The prima- with rare and well-recognised muscu-
Laura C. Jorgenson, MD ry objective of this review is to critically loskeletal disorders, like spondyloar-
Sadia Ilahi, MD describe the iHPoPT/SpA phenotype thritis (SpA) and mimics of ankylosing
Please address correspondence to: defined by established criteria and its spondylitis (AS) (1-3). Hypoparathy-
Alfonse T. Masi, differentiation from AS. Five databases roid syndromes, whether idiopathic,
Department of Medicine, were comprehensively searched without iatrogenic, or familial, are character-
University of Illinois College
of Medicine at Peoria,
time limit to retrieve 14 (11M, 3F) iH- ised by decreased parathyroid hormone
One Illini Drive, PoPT/SpA cases. Their demographic, (PTH), hypocalcaemia, hyperphos-
Peoria, IL 61605, USA. clinical, laboratory, radiographic, and phataemia, neuromuscular hyperir-
E-mail: amasi@uic.edu HLA-B27 status were compared to two ritability, subcutaneous calcifications,
ORCID ID: 0000-0002-9695-6634 national series of AS patients. Mean and normal or increased bone mineral
Received on February 15, 2021; accepted (SD) onset age of musculoskeletal density (BMD) (2). Pseudohypopar-
in revised form on April 26, 2021. symptoms [32.5 (9.7)] was significant- athyroidism (PHP) is a genetic form
Clin Exp Rheumatol 2021; 39: 1422-1431. ly older than 943 German AS patients of hypoparathyroidism with increased
© Copyright Clinical and [25.1 (8.5), (p=0.004)] and 842 Span- PTH which may have similar SpA
Experimental Rheumatology 2021. ish AS patients [26.1 (9.7), (p=0.030)]. manifestations (4) as primary hypopar-
Radiographic lesions of iHPoPT/SpA athyroidism (1, 2).
Key words: spondyloarthritis, differ morphologically from skeletal Primary hyperparathyroid syndromes
idiopathic hypoparathyroidism, alterations in hyperparathyroid and are caused by hypersecretion of PTH
ankylosing spondylitis, hypophosphataemic syndromes which resulting in low serum phosphate lev-
neuromuscular hypercontractility, often have inadequate bone mineralisa- els, normo- or hyper-calcaemia, and
resting axial hypertonicity tion and decreased bone mineral den- increased bone resorption at the sub-
sity (BMD). Clinical musculoskeletal periosteal and bone marrow interface
manifestations were greater (pSpA in idiopathic hypoparathyroidism / A.T. Masi et al. in impaired bone metabolism and in- tous and entheseal ossifications, sub- clude reports of diffuse idiopathic skel- adequate mineralisation, causing os- cutaneous and ectopic calcification, etal hyperostosis (DISH) or ossification teomalacia or softening and weaken- and ankylosing spondylitis-like back of the posterior longitudinal ligament ing of bones (6). Hypophosphataemic disease (1-3, 12, 15). (OPLL). Cited references of retrieved osteomalacia in adults can result in The primary objective of this critical articles were searched for additional exuberant enthesopathic calcification narrative case review is to describe the case reports (Table I). The lead author of tendon, ligament, and joint capsule clinical-radiographic consistency of determined that accepted cases were insertions in the axial and appendicular reported iHPoPT/SpA cases. The sec- documented as primary or idiopathic skeleton without known pathogenesis ondary aim is to differentiate its “neu- hypoparathyroidism and not including (7). romuscular hypercontractility” mecha- pseudohypoparathyroidism (2,4, 12). The association of parathyroid dis- nistic feature (1, 2, 13, 15) from the Data were summarised into pre-defined eases and osteomalacia with various previously proposed “innate resting tables by the lead author. musculoskeletal disorders and skeletal (passive) axial myofascial hypertonic- Diagnostic features at presentation of abnormalities are not well defined (7). ity” in AS (11,16). accepted cases (17-30) are summarised Skeletal abnormalities in XLH, as oste- Since 1953, 14 symptomatic cases of (Table I). Cases qualified for serum hy- omalacia, enthesopathy, and periosteal iHPoPT were reported to show radio- pocalcaemia level below 8.0 mg/dl or hyperostosis, are age related and clini- graphic syndesmophyte and entheso- 2.0–2.12 mmol/L (21 reported 2.2) and cally encountered along sites of muscu- phyte lesions associated with a clini- serum hyperphosphataemia above 4.5 lar attachment (8). Since bone spur for- cal axial spondyloarthritis phenotype mg/dl (20 reported 4.3) or 1.46 mmol/L mation at entheses (enthesophytes) can (iHPoPT/SpA) (17-30). Unlike AS, (2, 12). Only the initial accepted case occur as an adaptive tissue reaction to iHPoPT/SpA cases do not have the report in 1953 (17) was longitudinal in mechanical stress (9), bony malforma- typical structural sacroiliac joint (SIJ) the sense of a follow-up after a 13-year tions in osteomalacia may theoretically plain radiographic lesions of erosions earlier report in 1940 (31). The majority result from decreased physical resist- or bony bridging nor its high frequency of iHPoPT/SpA cases had documenta- ance to entheseal stresses. Regarding of HLA-B27 positivity (1-3, 12). No tion of hypocalcaemia only at presenta- BMD, tibial bone mass in children and mechanistic pathway has been offered tion (Table I), although a number had adults is increased with greater muscle to explain the similarity and differen- earlier neuromotor manifestations of force, suggesting the pathway of myo- tiation of iHPoPT/SpA and AS. Further hypoparathyroidism. Each case report fascial stress stimulating bone develop- study of parathyroid disorders (1, 2, 4, was reviewed for authors’ diagnoses ment (10). Younger adult AS patients 5) and hypophosphataemic syndromes (Table I). Each of the 14 reported iH- were reported to have greater resting (6-8) promise to clarify respective PoPT/SpA cases (17-30) was evaluated (passive) lumbar extensor myofascial structural stresses, strains, microin- in terms of quality of a case report (32) stiffness than normal volunteers (11). jury, and repair processes in relation and CARE guidelines (33) indepen- Idiopathic hypoparathyroidism (iH- to the axial iHPoPT/SpA phenotype. dently by both co-authors. Individual PoPT) is a rare disease associated with scores and CARE checklist assess- other endocrine dysfunction and mus- Methods ments can be provided on request. De- culoskeletal manifestations (1, 2, 12). This critical literature review searched mographic, clinical, and radiographic In 1939, six new cases of iHPoPT were PubMed and Embase databases, Med- findings at presentation (Table II) were reported with review of eight previous line via Ovid, the Cochrane Database compared to large series of AS patients patients (13). This disorder was defined of Systematic Reviews, and the Cen- from the German and Austrian ankylos- as having neuromuscular manifesta- tral Registry of Controlled Trials by a ing spondylitis societies (34) and the tions of stiffness, cramps, and rigidity medical reference librarian with input National Registry of Spondyloarthritis of extremities or whole body (13). The from the principal investigator. The of the Spanish Society of Rheumatol- proposed criteria for iHPoPT included: key words searched without time limits ogy (REGISPONSER database) (35, low serum calcium; high serum inor- were: “hypoparathyroidism”; “spondy- 36). The comparator AS cohorts (34- ganic phosphate; chronic tetany, and loarthropathy” or “spondylarthritis” or 36) were selected because of their large absence of other explanatory causative “spondylitis”, or “ankylosing spondy- size, national sampling, and recognition conditions for the serum abnormalities litis.” The search process was initially in the literature. Statistical probability (13). In 1952, a new case of iHPoPT performed on 03-28-19 and repeated of differences in binomial frequencies and detailed review of the total previ- on 04-28-20, yielding an additional of attributes in iHPoPT/SpA cases ous literature yielded 52 patients, none report of post-thyroidectomy hypopar- versus comparison series was deter- having a possibility of post-operative athyroidism, not eligible in this review. mined by Fisher’s exact test calcula- hypoparathyroidism (14). Rheumatic For greater consistency among reported tor and by t-test of mean (SD) of recognised to include muscle cramps cluded only those describing iHPoPT. continuous variables in case subgroups and myopathies, increased neuromus- Unless titles also included the key- . Clinical and Experimental Rheumatology 2021 1423
SpA in idiopathic hypoparathyroidism / A.T. Masi et al. Table I. Diagnostic features at presentation of spondyloarthritis in cases associated with idiopathic hypoparathyroidism, 1953-2016* Reference no., Age Duration Tests at presentation Authors’ Prior cases First author, and of low Ca2+ diagnoses cited Year reported sex (years) Low Ca2+ High P Low PT 17, Salvesen, ’53 57 M 9 5.4 mg/dL 5.7 mg/dL ND Ossification Earlier adm 18, Gibberd, ’65 29 F present 7.4 mg/dL 5.8 mg/dL ND Abn bone (17) 19, Chaykin, ’69 59 M present 6.6 mg/dL 6.4 mg/dL ND SpA (17,18) 20, Adams, ’77 62 M 2 5.9 mg/dL WNLs Und Ossification (17-19) 21, Korkmaz, ’05 45 M 7 2.2 mmol/L 4.6 mmol/L
SpA in idiopathic hypoparathyroidism / A.T. Masi et al.
tion (LOM) affecting the neck, back, Table III. Ages at diagnosis and onset and years of diagnosis delay of spondyloarthritis
and hips in the 13 iHPoPT/SpA cases cases in idiopathic hypoparathyroidism vs. patients with idiopathic hypoparathyroidism
and series of ankylosing spondylitis.
(excluding 23) with specified data (Ta-
ble II). The mean (SD) duration of mus- Spondyloarthritis in idiopathic hypoparathyroidism (iHPoPT/SpA)
culoskeletal manifestations at presenta-
tion and diagnosis was 15.6 (7.9) years Diagnosis age Onset age Diagnosis delay
(n=14) (n=11) (n=11)
(range 8-35 years) in 11 specified cases
Mean (SD) Mean (SD) Mean (SD)
(Tables II, III). In the total 14 iHPoPT/
SpA cases, 54 radiographic syndesmo- 48.8 (10.3) 32.5 (9.7) 15.6 (7.9)
phyte and enthesophyte lesions were re-
ported involved: 30 syndesmophyte (7 Idiopathic hypoparathyroidism (iHPoPT)
cervical, 10 thoracic, 13 lumbar), 9 pel- Diagnosis age Onset age Diagnosis delay p difference
vic, and 15 other enthesophyte lesions Mean (SD) Mean (SD) Mean (SD) (from iHPoPT/SpA)
(2 shoulders, 1 sternal, 12 hips) (Table
II). Postural abnormalities simulating Steinberg et al., (14) Diagnosis: pSpA in idiopathic hypoparathyroidism / A.T. Masi et al.
Table IV. Presenting musculoskeletal manifestations by regional localisations in idiopathic A counterpart non-radiographic axial
hypoparathyroid spondyloarthritis cases compared to ankylosing spondylitis from the Spa- SpA includes patients where sacroiliitis
nish National Registry by all ages and early- vs. late-onset disease.*
is evident only on magnetic resonance
Spanish AS patients by onset age imaging (MRI) (3, 40). Axial SpA is
characterised pathologically by new
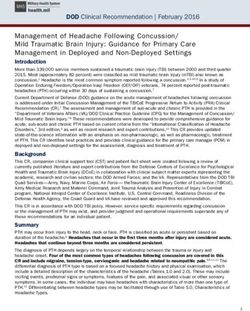
Presenting regional iHPoPT/SpA All agesSpA in idiopathic hypoparathyroidism / A.T. Masi et al. ing anti-inflammatory therapy, com- BMD, most notable at the lumbar spine, etal and ligamentous changes resem- parative studies performed for over a was found in a small cross-sectional bling AS.” However, no iHPoPT/SpA decade have not definitely determined study of hypoparathyroid patients with case report inferred a sequential cau- that TNF inhibitor (TNFi) therapy over either iHPoPT or post-thyroidectomy sality of hypocalcaemia from iHPoPT 2 years can inhibit bone proliferation or and attributed to optimised bone min- causing neuromuscular irritability and progression of spinal structural damage eralisation (59). The influence of aging hypercontractility, thereby contributing in AS patients (50). Such results (50) and maleness will require further study to micro-injury and skeletal entheso- enhance the present study focusing on in iHPoPT/SpA. pathic lesions, which is the proposed biomechanical influences which may The SpA in iHPoPT may be a “natural mechanism in this review. precede micro-injury and inflammatory experiment” (60) which allows probing An earlier proposed biomechanical con- markers not addressed in the preceding if chronic axial neuromuscular hyper- cept of AS (11, 16) was extended to il- TNFi studies (50) and deserve future irritability and hyper-contractility con- lustrate how hypocalcaemia in iHPoPT critical attention. tributes to syndesmophyte and entheso- increases axial neuromuscular irritabil- In a systematic review of SpA which phyte lesions of the spine and pelvis. A ity and hypercontractility and differs analysed plain radiography or ultra- 2018 review of axial SpA (61) stressed from AS (Fig. 1). The hypercontractil- sound (US) techniques (none with that the new technique of low dose CT ity in iHPoPT is differentiated from in- MRI), a greater BMI was considered a is a major step forward in assessing syn- nate resting (passive) axial myofascial biomechanical factor which may trigger desmophyte score and new bone forma- hypertonicity proposed in AS (11, 16). an inflammatory process and new bone tion, which may be applied in future to The SIJs are not entheses, but cartilagi- formation in healing at those sites (51). comparison of iHPoPT/SpA and AS. nous joints which primarily support the Biomechanical factors may also be a Reports of iHPoPT consistently sup- vertical load of the spine and trunk (66). main contributor to entheseal changes of port hypocalcaemia causing increased The proposed mechanistic concept lower extremities in normal adults (52). neuronal and muscular excitability and (Fig. 1) needs further documentation In a study of 80 healthy adults, the prev- stiffness (1, 2, 12, 62-64), which may for its support, e.g. a “dose-response” alence of ultrasound (US) enthesitis le- plausibly contribute to development of relation of chronic hypocalcaemic axial sions defined by the OMERACT group associated SpA in susceptible persons. neuromuscular hypercontractility in (53) increased with age, body mass in- The pattern of syndesmophytes in iH- iHPoPT leading to development of SpA dex (BMI), and high physical activity PoPT/SpA are described to originate (23). Longitudinal analysis of separate (54). Stratification of subjects
SpA in idiopathic hypoparathyroidism / A.T. Masi et al.
Fig. 1. Proposed pathways
of axial spondyloarthritis in
idiopathic hypoparathyroid-
ism (active, pink) vs. anky-
losing spondylitis (resting,
yellow) and common demo-
graphy and mechanobiology
factors (orange).
cited 2 previously reported cases in this with other cohorts or with series of axi- strength of evidence (SOE) and quality
review (19, 20) as being different from al spondyloarthritis patients. This liter- of an observational study may be in-
his patient. The duration and degree of ature review is also limited in its ability creased by additional strong evidence
hypocalcaemia is an essential determi- to determine if a causative sequential of association, consistency and homo-
nant for future research in the co-occur- relation occurs between iHPoPT and geneity of the data, and evidence of a
rence of iHPoPT and SpA. SpA versus a coincidental or statistical dose response gradient (74, 75).
A limitation of this review is restriction association. A strength of this critical analysis in-
only to cross-sectional case reports Randomised clinical trials (RCTs) are cludes not detecting bias in case reports
of individual patients with short-term often classified as “high quality” evi- regarding descriptions of muscular
follow-up after iHPoPT/SpA diagnosis dence regarding efficacy of new treat- spasticity or skeletal enthesopathy le-
and treatment of hypocalcaemia (17- ments for patients with a specific dis- sions (Tables I, II). All analysed cases
31). Selection bias cannot be excluded ease, whereas case reports and other had sufficient data to qualify for a con-
in the reporting of age, gender, or dura- observational data are considered as firmed iHPoPT diagnosis. Only symp-
tion of SpA manifestations in the ana- hypothesis generators with initially tomatic SpA patients with radiographic
lysed cases (Tables I, II). Additional classified lower grade of evidence (69- documentation of syndesmophytes or
iHPoPT/SpA cases may be available in 72). However, an increasing argument axial enthesophytes associated with
the literature or textbooks which were is being made in defense of case re- iHPoPT were included in the review for
not retrieved in our comprehensive ports and its restoration as a prominent greater consistency and comparability
search of five databases. Unrecognised and useful medical reporting strategy of the case subjects. Cases had compa-
potential confounders may not allow (73). Methods to improve the validity rable SpA manifestations of pain, stiff-
generalisability of the findings. Com- of results from aggregation of single ness or LOM of the neck, back, or hips
parison of the iHPoPT/SpA cases was cases are increasingly needed, includ- (Table II) and all but 2 reports (24, 25)
made with two national series of AS ing estimation of an effect size and had cited preceding cases of iHPoPT/
patients (34-36) and results may differ generalisability of the data (73). The SpA, reflecting consistency (Table I).
1428 Clinical and Experimental Rheumatology 2021SpA in idiopathic hypoparathyroidism / A.T. Masi et al. Also, t-test comparison of the continu- A widely accepted view among axSpA tion resulting in increased muscle tone ous variables (Tables I, II) between ear- experts is the chronologic transition of rather that overt shivering (80). Wheth- lier versus later cases was performed chronic back pain clinical manifesta- er α-actinin-3 deficient individuals also to assess consistency. Mean (SD) age tions, to SIJ inflammatory changes on display an increased passive muscle at presentation and diagnosis (Table I) MRI, and further radiographic structur- tone (i.e. without neuronal activation) was closely similar between the 7 earlier al lesions on conventional radiography requires further clinical assessment, in- [49.7 (11.2)] and 7 later [47.9 (10.1)] (CR), as mainly preceding syndesmo- cluding myotonometry (11). reported cases (p=0.750). Mean (SD) phyte formation (78, Fig. 1). The pre- The concept in this review could be serum Ca (mg/dL) was similar in the ceding sequence differs from current tested independently in a follow-up de- earlier [6.3 (1.4)] and later [4.8 (1.6)] findings in the iHPoPT/SpA phenotype termination of SpA occurrence in the cases (p=0.097), as was serum P (mg/ which has prominent syndesmophyte large HypoparaNet iHPoPT cohort (81) dL) of [7.1 (3.3)] and [6.4 (1.0)], respec- formation without SIJ structural le- compared to a population and disease tively (p=0.578) (Table I). Parathyroid sions. The newly developed scoring control. This large-scale national data- hormone (pg/ml) was only reported in method of bone formation on low dose base of chronic hypoparathyroidism is 8 cases since 2005, with similar mean computed tomography (LD-CT) of the derived from expert medical-surgical (SD) levels in 4 earlier [3.9 (2.3)] and 4 whole spine is a more sensitive method centres in Italy and includes 61 adult later [2.8 (1.5)] reports (p=0.453). The for assessing the formation and growth iHPoPT, 352 post-surgical and 37 ge- mean (SD) number of total radiographic of syndesmophytes than CR (79). New- netic and other forms (81). Association lesions per patient was also similar be- ly detected iHPoPT/SpA cases can be and development of SpA could be a fu- tween earlier [3.9 (1.1)] and later [3.7 analysed with LD-CT and compared to ture research objective of this project (1.3)] cases (p=0.822) as was ESR [36.6 axSpA patients to compare the respec- (81). Such further SpA outcome stud- (8.4)] vs. [39.8 (23.5)], respectively tive degrees of syndesmophyte forma- ies can incorporate newly standard- (p=0.782) (Table II). Such agreement tion in relation to SIJ changes. ised myotonometry (11) or shear wave suggests that quantitatively combining The novel translational mechanobio- elastography (82) techniques to meas- case reports may improve conclusions in logical proposal of innate lumbar hu- ure axial myofascial stiffness. Future the field of rare diseases (70, 73). A nov- man resting myofascial tone (HRMT) longitudinal study of adult iHPoPT and el hypothesis on causation can derive contributing to AS physiopathogenesis other parathyroid disorders is needed to from a critical review of well-document- (Fig. 1) are supported by preceding determine an objective dose-response ed case reports describing association of studies (11, 16, 41, 44-47, 75). Genetic effect of degree and duration of hypoc- two distinct conditions, especially in- factors contribute essentially all risk to alcaemia interacting with age and sex in volving a rare disorder (32, 70). AS development and HLA-B27 strong- the development of SpA. As important Alamanos et al. (76) recently published ly (circa 40-100-fold) associates with new quality evidence becomes available a systematic review of incidence stud- risk (44). Both HLA-B27 and AS prev- (83), the proposed hypothesis can be ies of SpA subtypes indexed in Pub- alence increase with colder climates, reconsidered and appropriately revised. Med electronic database during the last hypothesised to be an evolutionary 25 years (1-1-1995 to 12-31-2019). In thermogenesis trait related to increased Conclusions the latter review (76), the most recent passive lumbar HRMT (44). The rare iHPoPT/SpA phenotype pre- cohort study of SpA incidence (2014- A recent physiologic, proteomic, and sents mainly in middle-aged males as 2016) was by Hočevar et al. (77) and genetic muscle study of α-actinin-3 widespread axial pain and LOM, par- the only general population comparison deficient healthy young males (n=8) ticularly in cervical, lumbar, and hip re- of axial and peripheral SpA, based on versus normal males (n=11), as well as gions. Its radiographic syndesmophyte ASAS criteria (48,78). Of the total 302 wild type (n=18) and knockout (n=16) and enthesophyte lesions simulate AS. SpA cases, 98 (32.5%) were classified mice for this trait, found that absence of The mean ESR was similar to 2 cohorts as axial versus 204 (67%) peripheral protein α-actinin-3, normally expressed of active AS patients by physician as- SpA. The axial SpA group included 57 in fast-twitch skeletal muscle, is asso- sessment. The iHPoPT/SpA cases dif- (58.2%) AS and 31 (31.6%) undiffer- ciated with improved thermogenesis fer from AS by a paucity of structural entiated SpA (without conventional during cold-water emersion (80). The SIJ lesions of erosions and bony bridg- radiographic SIJ structural changes) population frequency of this deficiency ing and infrequent HLA-B27 positivity. for a combined annual incidence rate trait increases with distance from Afri- Its hypocalcaemic axial neuromuscular of 4.6 cases per 100,000 persons per ca and is inferred to have resulted from hyperirritability and hypercontractil- year. As expected, median (IQR) age modern humans migrating from Africa ity are differentiated from a previously was significantly (p=0.004) less in axial to colder climates over 50,000 years proposed resting (passive) innate axial [39.8 (33.1–55.4)] than peripheral [49.8 ago (80), as previously inferred for muscular hypertonicity and increased (36.0–58.2)] SpA (77) and axial had AS and HLA-B27 (44). The improved stiffness in AS. The iHPoPT/SpA cas- significantly (p
SpA in idiopathic hypoparathyroidism / A.T. Masi et al.
Acknowledgements (‘entheses’) in relation to exercise and/or curring hypoparathyroidism. Rheumatol Int
mechanical load. J Anat 2006; 208: 471-90. 2011; 31: 681-3.
D.M.F.M. van der Heijde, Professor
10. ANLIKER E, RAWER R, BOUTELLIER U, TOI- 27. KAJITANI TR, SILVA RV, BONFÁ E, PEREIRA
of Rheumatology, Leiden University GO M: Maximum ground reaction force in RM: Hypoparathyroidism mimicking anky-
Medical Center contributed her essen- relation to tibial bone mass in children and losing spondylitis and myopathy: a case re-
tial critique, particularly on clarifying adults. Med Sci Sports Exerc 2011; 43: 2102- port. Clinics (Sao Paulo) 2011; 66: 1287-90.
9. 28. JAKKANI RK, SUREKA J, MATHEW J: Spon-
study aims and justification of selected 11. ANDONIAN BJ, MASI AT, ALDAG JC et al.: dyloarthropathy occurring in long-standing
control ankylosing spondylitis cohorts. Greater resting lumbar extensor myofascial idiopathic hypoparathyroidism. Radiol Case
Brian Andonian MD, Assistant Pro- stiffness in younger ankylosing spondylitis Rep 2015; 6: 545.
fessor, Rheumatology Division, Duke patients than age-comparable healthy volun- 29. JOHN DR, SUTHAR PP: Radiological features
teers quantified by myotonometry. Arch Phys of long-standing hypoparathyroidism. Pol J
University Medical Center contributed Med Rehabil 2015; 96: 2041-7. Radiol 2016; 81: 42-5.
his overall critique, particularly on de- 12. MANNSTADT M, BILEZIKIAN JP, THAKKER 30. ILLEEZ MEMETOGLU O, UNLU OZKAN F,
scriptions of postural abnormalities of RV et al.: Hypoparathyroidism. Nat Rev Dis TARAKTAS A, AKTAS I, NAZIKOGLU C:
the cases and responses to treatment of Primers 2017; 3: 17055. Idiopathic hypoparathyroidism mimicking
13. DRAKE TG, ALBRIGHT F, BAUER W, CASTLE- ankylosing spondylitis: a case report. Acta
hypocalcaemia. MAN B: Chronic idiopathic hypoparathy- Reumatol Port 2016; 41: 82-5.
Deborah L Lauseng, AMLS, Assistant roidism; report of 6 cases with autopsy findings 31. KOBRO M: Latent idiopathic tetany. Nord
Professor and Regional Head Librar- in one. Ann Intern Med 1939; 12: 1751-65. Med 1940; 8: 2256.
ian, Library of the Health Sciences – 14. STEINBERG H, WALDRON BR: Idiopathic 32. PIERSON DJ: How to read a case report (or
hypoparathyroidism; an analysis of fifty-two teaching case of the month). Respir Care
Peoria, University of Illinois Chicago cases, including the report of a new case. 2009; 54: 1372-8.
contributed her expertise with the lit- Medicine (Baltimore) 1952; 31: 133-54. 33. RILEY DS, BARBER MS, KIENLE GS et al.:
erature searching and in the review of 15. van OFFEL JF, DE GENDT CM, de CLERCK LS, CARE guidelines for case reports: explana-
STEVENS WJ: High bone mass and hypocal- tion and elaboration document. J Clin Epide-
the Methods section.
caemic myopathy in a patient with idiopathic miol 2017; 89: 218-35.
All acknowledged persons gave per- hypoparathyroidism. Clin Rheumatol 2000; 34. FELDTKELLER E, KHAN MA, van der HEI-
sonal permission to Dr Masi to publish 19: 64-6. JDE D, van der LINDEN S, BRAUN J: Age at
this statement. 16. MASI AT, NAIR K, ANDONIAN BJ et al.: disease onset and diagnosis delay in HLA-
Integrative structural biomechanical con- B27 negative vs. positive patients with anky-
cepts of ankylosing spondylitis. Arthritis losing spondylitis. Rheumatol Int 2003; 23:
References 2011; 2011: 205904. 61-6.
1. WEN HY, SCHUMACHER HR JR, ZHANG LY: 17. SALVESEN HA, BÖE J: Idiopathic hypopar- 35. COLLANTES E, ZARCO P, MUÑOZ E et al.:
Parathyroid disease. Rheum Dis Clin North athyroidism; observations on two cases, one Disease pattern of spondyloarthropathies in
Am 2010; 36: 647-64. complicated by moniliasis and idiopathic Spain: description of the first national regis-
2. MANNSTADT M, MITCHELL DM: Clinical steatorrhea and one with an unusual degree of try (REGISPONSER) extended report. Rheu-
manifestations of hypoparathyroidism. In: calcium deposition in the bones. Acta Endo- matology (Oxford) 2007; 46: 1309-15.
BILEZIKIAN JP, MARCUS R, LEVINE MA, crinol (Copenh) 1953; 14: 214-26. 36. MONTILLA C, DEL PINO-MONTES J et al.:
MARCOCCI C, SILVERBERG SJ, POTTS JT JR 18. GIBBERD FB: Idiopathic hypoparathyroidism Clinical features of late-onset ankylosing
(Eds.). The Parathyroids: Basic and Clinical with unusual bone changes and spastic para- spondylitis: comparison with early-onset dis-
Concepts, Third Edition, Elsevier, Inc. (Am- plegia. Acta Endocrinol (Copenh) 1965; 48: ease. J Rheumatol 2012; 39: 1008-12.
sterdam, Boston) 2015, Ch 53:761-70. 23-30. 37. NAKAMURA Y, MATSUMOTO T, TAMAKOSHI
3. SLOBODIN G, LIDAR M, ESHED I: Clinical 19. CHAYKIN LB, FRAME B, SIGLER JW: Spon- A et al.: Prevalence of idiopathic hypopar-
and imaging mimickers of axial spondyloar- dylitis: a clue to hypoparathyroidism. Ann athyroidism and pseudohypoparathyroidism
thritis. Semin Arthritis Rheum 2017; 47: 361- Intern Med 1969; 70: 995-1000. in Japan. J Epidemiol 2000; 10: 29-33.
8. 20. ADAMS JE, DAVIES M: Paravertebral and pe- 38. MUÑOZ-VILLANUEVA MC, MUÑOZ-GOMA-
4. SHARMA M, NOLKHA N, SHARMA A et al.: ripheral ligamentous ossification: an unusual RIZ E, ESCUDERO-CONTRERAS A, PÈREZ-
Spondyloarthropathy-like findings and dif- association of hypoparathyroidism. Postgrad GUIJO V, COLLANTES-ESTÉVEZ E: Biological
fuse osteosclerosis as the presenting feature Med J 1977; 53: 167-72. and clinical markers of disease activity in an-
of pseudohypoparathyroidism. J Clin Rheu- 21. KORKMAZ C, YAŞAR S, BINBOĞA A: Hypo- kylosing spondylitis. J Rheumatol 2003; 30:
matol 2016; 22: 102-4. parathyroidism simulating ankylosing spon- 2729-32.
5. SILVA BC, BILEZIKIAN JP: Skeletal abnor- dylitis. Joint Bone Spine 2005; 72: 89-91. 39. UGUR M, BAYGUTALP NK, MELIKOGLU
malities in hypoparathyroidism and in prima- 22. SIVRIOGLU K, OZCAKIR S, KAMAY O: MA, BAYGUTALP F, ALTAS EU, SEFEROGLU
ry hyperparathyroidism. Rev Endocr Metab Hypoparathyroidism: a rare cause of spondy- B: Elevated serum interleukin-23 levels in
Disord 2020 Nov 16 [Online ahead of print]. loarthropathy. Scand J Rheumatol 2006; 35: ankylosing spondylitis patients and the rela-
6. CARPENTER TO: The expanding family of 494-5. tionship with disease activity. Nagoya J Med
hypophosphatemic syndromes. J Bone Miner 23. GOSWAMI R, RAY D, SHARMA R et al.: Sci 2015; 77: 621-7.
Metab 2012; 30: 1-9. Presence of spondyloarthropathy and its 40. PODDUBNYY D, APPEL H, SIEPER J: Inves-
7. BURNSTEIN MI, LAWSON JP, KOTTAMASU clinical profile in patients with hypoparathy- tigation of involved tissue in axial spondy-
SR, ELLIS BI, MICHO J: The enthesopathic roidism. Clin Endocrinol 2008; 68: 258-63. loarthritis--what have we learnt from immu-
changes of hypophosphatemic osteomala- 24. BEN FREDJ H, HALIFA M, HAMMOUDA M, nohistochemical studies? Best Pract Res Clin
cia in adults: radiologic findings. AJR Am J ZEGLAOUI H, BEL HAJ SLAMA K, BOUAJINA Rheumatol 2010; 24: 715-9.
Roentgenol 1989; 153: 785-90. E: [Hypoparathyroidism simulating ankylos- 41. NEERINCKX B, LORIES R: Mechanisms,
8. HARDY DC, MURPHY WA, SIEGEL BA, REID ing spondylitis.] Tunis Med 2010; 88: 767-8. impact and prevention of pathological bone
IR, WHYTE MP: X-linked hypophosphatemia 25. GEDIK A, YILMAZ M, ERAYDIN A, GUNES regeneration in spondyloarthritis. Curr Opin
in adults: prevalence of skeletal radiographic M, ERASLAN S: Hypoparathyroidism mim- Rheumatol 2017; 29: 287-92.
and scintigraphic features. Radiology 1989; icking ankylosing spondylitis. Endocrine 42. LORIES RJ, HAROON N: Evolving concepts
171: 403-14. Abstracts 2010; 22 (P96). of new bone formation in axial spondyloar-
9. BENJAMIN M, TOUMI H, RALPHS JR, BY- 26. IBN YACOUB YI, ROSTOM S, HAJJAJ-HAS- thritis: insights from animal models and hu-
DDER G, BEST TM, MILZ S: Where tendons SOUNI N: Uncommon case of ankylosing man studies. Best Pract Res Clin Rheumatol
and ligaments meet bone: attachment sites spondylitis associated with spontaneous oc- 2017; 31: 877-86.
1430 Clinical and Experimental Rheumatology 2021SpA in idiopathic hypoparathyroidism / A.T. Masi et al.
43. SIEPER J, PODDUBNYY D: Axial spondyloar- 26: S182 and Osteoporos Int 2012; 23 (Sup- based medicine in rare diseases. Mol Genet
thritis. Lancet 2017; 390: 73-84. pl. 2): S215-6. Metab 2018; 123: 69-75
44. MASI AT, WALSH EG: Ankylosing spondyli- 57. KIM TJ, KIM TH, JUN JB, JOO KB, UHM WS: 71. KAMIYA H, PANLAQUI OM: Prognostic fac-
tis: integrated clinical and physiological per- Prevalence of ossification of posterior longi- tors for acute exacerbation of idiopathic pul-
spectives. Clin Exp Rheumatol 2003; 21: 1-8. tudinal ligament in patients with ankylosing monary fibrosis: protocol for a systematic
45. MASI AT: Might axial myofascial properties spondylitis. J Rheumatol 2007; 34: 2460-2. review and meta-analysis. BMJ Open 2019;
and biomechanical mechanisms be relevant 58. WESTERVELD LA, van UFFORD HM, VER- 9: e028226.
to ankylosing spondylitis and axial spondy- LAAN JJ, ONER FC: The prevalence of diffuse 72. GIOVANNUCCI E, RIMM E: Red and pro-
loarthritis? Arthritis Res Ther 2014; 16: 107. idiopathic skeletal hyperostosis in an outpa- cessed meat consumption and risk for all-
46. JACQUES P, LAMBRECHT S, VERHEUGEN E tient population in The Netherlands. J Rheu- cause mortality and cardiometabolic out-
et al.: Proof of concept: enthesitis and new matol 2008; 35: 1635-8. comes. Ann Intern Med 2020; 172: 510-1.
bone formation in spondyloarthritis are driv- 59. CHAN FK, TIU SC, CHOI KL, CHOI CH, KONG 73. NAKAMURA T, IGARASHI H, ITO T, JENSEN
en by mechanical strain and stromal cells. AP, SHEK CC: Increased bone mineral density RT: Important of case-reports/series, in rare
Ann Rheum Dis 2014; 73: 437-45. in patients with chronic hypoparathyroidism. diseases: using neuroendocrine tumors as an
47. van MECHELEN M, GULINO GR, de VLAM K, J Clin Endocrinol Metab 2003; 88: 3155-9. example, World J Clin Cases 2014; 2: 608-13.
LORIES R: Bone disease in axial spondyloar- 60. SNELL A, REEVES A, RIEGER M et al.: 74. KATZ DL, KARLSEN MC, CHUNG M et al.:
thritis. Calcif Tissue Int 2018; 102: 547-58. WHO regional office for Europe’s Natural Hierarchies of evidence applied to life-
48. RUDWALEIT M, van der HEIJDE D, LANDE- Experiment Studies Project: an introduction style medicine (HEALM): introduction of
WÉ R et al.: The development of Assessment to the series. Eur J Public Health 2018; 28 a strength-of-evidence approach based on a
of SpondyloArthritis International Society (Suppl. 2): 1-3. methodological systematic review. BMC Med
classification criteria for axial spondyloar- 61. CARLI L, CALABRESI E, GOVERNATO G, Res Methodol 2019; 19: 178.
thritis (part II): validation and final selection. BRAUN J: One year in review 2018: axial 75. MASI AT: Do microinjury mechanisms com-
Ann Rheum Dis 2009; 68: 777-83. spondyloarthritis. Clin Exp Rheumatol 2019; plement inflammation in sacroiliac joint an-
49. RAMIRO S, VAN DER HEIJDE D, VAN TUBER- 37: 889-88. kylosis on magnetic resonance imaging of
GEN A et al.: Higher disease activity leads to 62. ZAMBELIS T, LICOMANOS D, LEONARDOS young spondyloarthritis patients? Comment
more structural damage in the spine in an- A, POTAGAS C: Neuromyotonia in idiopathic on the article by Bray et al. Arthritis Rheu-
kylosing spondylitis: 12-year longitudinal hypoparathyroidism. Neurol Sci 2009; 30: matol 2019; 71: 2129-30.
data from the OASIS cohort. Ann Rheum Dis 495-7. 76. ALAMANOS Y, PELECHAS E, VOULGARI PV,
2014; 73: 1455-61. 63. AGRAWAL L, HABIB Z, EMANUELE NV: DROSOS AA: Incidence of spondyloarthritis
50. van der HEIJDE D, LANDEWÉ R: Inhibition Neurologic disorders of mineral metabolism and its subtypes: a systematic review. Clin
of spinal bone formation in AS: 10 years after and parathyroid disease. Handb Clin Neurol Exp Rheumatol 2021; 39: 660-7.
comparing adalimumab to OASIS. Arthritis 2014; 120: 737-48. 77. HOČEVAR A, POTOČNIK PUCELJ N, JEŠE R,
Res Ther 2019; 21: 225. 64. HAN P, TRINIDAD BJ, SHI J: Hypocalcemia- PAVIČ-NIKOLIČ M, TOMŠIČ M, ROTAR Z:
51. BAKIRCI S, DABAGUE J, EDER L, McGONA- induced seizure: demystifying the calcium The incidence of spondyloarthritis in Slove-
GLE D, AYDIN SZ: The role of obesity on in- paradox. ASN Neuro 2015; 7: 1-9. nia. Medicine (Baltimore) 2019; 98: e16177.
flammation and damage in spondyloarthritis: 65. CHAKRAVARTY SD, MARKENSON JA: 78. RUDWALEIT M: New approaches to diag-
a systematic literature review on body mass Rheumatic manifestations of endocrine dis- nosis and classification of axial and periph-
index and imaging. Clin Exp Rheumatol ease. Curr Opin Rheumatol 2013; 25: 37-43. eral spondyloarthritis. Curr Opin Rheumatol
2020; 38: 144-8. 66. VLEEMING A, SCHUENKE MD, MASI AT, 2010; 22: 375-80.
52. MASI AT, ANDONIAN B, van der HEIJDE CARREIRO JE, DANNEELS L, WILLARD FH: 79. de KONING A, DE BRUIN F, van den BERG R et
D: Biomechanical factors may be the main The sacroiliac joint: an overview of its anat- al.: Low-dose CT detects more progression of
contributor to entheseal changes in normal omy, function and potential clinical implica- bone formation in comparison to conventional
adults. J Rheumatol 2021; 48: 618-9. tions. J Anat 2012; 221: 537-67. radiography in patients with ankylosing spon-
53. BALINT PV, TERSLEV L, AEGERTER P et 67. SASI S, RAHIL A, VATTOTH S, CACKAMVAL- dylitis. Ann Rheum Dis 2018; 77: 293-9.
al.: Reliability of a consensus-based ultra- LI P, ABDULLAH W: Primary hypoparathy- 80. WYCKELSMA VL, VENCKUNAS T, HOUWE-
sound definition and scoring for enthesitis in roidism mimicking ankylosing spondylitis in LING PJ et al.: Loss of α-actinin-3 during
spondyloarthritis and psoriatic arthritis: an a young man with Fahr’s syndrome: a case human evolution provides superior cold resil-
OMERACT US initiative. Ann Rheum Dis report. Cureus 2020; 12: e10426. ience and muscle heat generation. Am J Hum
2018; 77: 1730-5. 68. SCHEN RJ: Unusual manifestation of hypoc- Genet 2021; 108: 446-57.
54. BAKIRCI S, SOLMAZ D, STEPHENSON W, alcemia. Brit Med J 1979; 2: 610. 81. MARCUCCI G, CIANFEROTTI L, PARRI S et
EDER L, ROTH J, AYDIN SZ: Entheseal chang- 69. COOK MC: Medical case reports in the age al.: HypoparaNet: A database of chronic hy-
es in response to age, body mass index, and of genomic medicine, Clin Transl Immunol poparathyroidism based on expert medical-
physical activity: An ultrasound study in 2015; 4: e45. surgical centers in Italy. Calcif Tissue Int
healthy people. J Rheumatol 2020; 47: 968- 70. SAMPAYO-CORDERO M, MIGUEL-HUGUET 2018; 103: 151-63.
72. B, PARDO-MATEOS A, MOLTÓ-ABAD M, MU- 82. MASAKI M, AOYAMA T, MURAKAMI T et
55. SOLMAZ D, BAKIRCI S, EDER L, ROTH J, ÑOZ-DELGADO C, PÉREZ-LÓPEZ J: Agree- al.: Association of low back pain with mus-
AYDIN SZ: Reply. J Rheumatol 2021; 48: ment between the results of meta-analyses cle stiffness and muscle mass of the lumbar
619-20. from case reports and from clinical studies back muscles, and sagittal spinal alignment in
56. CLARKE BL, LEIBSON TL, EMERSON JA, regarding the efficacy of laronidase therapy young and middle-aged medical workers. Clin
RANSON JE, LAGAST H: Co-morbid medi- in patients with mucopolysaccharidosis type Biomech (Bristol, Avon) 2017; 49: 128-33.
cal conditions associated with prevalent hy- I who initiated enzyme replacement therapy 83. MURAD MH: Clinical practice guidelines: a
poparathyroidism: a population-based study. in adult age: An example of case reports primer on development and dissemination.
[abstract SA0170]. J Bone Miner Res 2011; meta-analyses as a useful tool for evidence- Mayo Clin Proc 2017; 92: 423-33.
Clinical and Experimental Rheumatology 2021 1431You can also read