Prehospital paediatric emergency care
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
26 Review Articles Medical Education
Prehospital paediatric
emergency care
Citation: Kaufmann J, Laschat M, Wappler F: Prehospital paediatric emergency care.
Anästh Intensivmed 2020;61:026–037. DOI: 10.19224/ai2020.026
Summary more, competency and technical re 1 Abteilung für Kinderanästhesie,
Kinderkrankenhaus der Kliniken der Stadt
sources are not identical to those found
Because prehospital paediatric emer- Köln gGmbH
in a specialised environment, e.g. a (Direktor: Prof. Dr. F. Wappler)
gency care is commonly rendered by
paediatric emergency department. In a 2 Fakultät für Gesundheit, Universität
non-specialist teams, always operating Witten/Herdecke
prehospital environment, paediatric
in a suboptimal environment, simple (Dekan: Prof. Dr. S. Wirth)
emergencies and – for example – en-
and feasible treatment recommendations
dotracheal intubation are so uncommon
are required. First and foremost, these
that practice solely in this environment
are provided by the resuscitation guide-
cannot provide for advanced experience
lines, which provide recommendations
[1].
consistent with the above premise not
only for cardiac arrest but for most other
important situations. The laryngeal mask More than 80% of emergency physi-
airway and the intraosseous needle are cians are afraid of being over-
essential technical adjuncts for airway whelmed by paediatric emergencies
management and venous access respec- or have experienced overwhelming
tively. Equipment must be provisioned in such a situation [2].
for each and every age bracket. Simple
basic principles and support provided Complex deficits have been described
by references and aids can increase the in the context of simulated scenarios
safety of drug administration. Sound [3] and prehospital emergencies [4]; for
individual and institutional preparations example, difficulties with endotracheal
for paediatric emergencies ensure safe intubation arose in 2/3 of children
initial care of the child prior to ongoing with head injuries, whilst the same was
treatment provided by specialists. only true of 1/5 of adults in the same
health care setting. At the same time,
Introduction intravenous access was successfully
established in 86% of adults investi
When considering prehospital paediat- gated, whilst the same could only be
ric emergency care, it is imperative to said of 66% of children [5]. The European
develop strategies based on a realistic Resuscitation Council (ERC) Guidelines
analysis of circumstances and available note that due to real-life limitations,
resources, aiming to provide care at the recommendations must be “simple
as close to optimum level as possible. and feasible” [6]. Even though it may
Because the circumstances under which seem remarkable to read this in the Keywords
prehospital care is provided – consider preamble of a guideline, it is precisely Prehospital emergency care
for example the location, e.g. at the this basic nature, seeking compromise, – Children – Drug safety –
roadside – can per se be suboptimal, avoiding excessive burdens on the user Treatment recommendations
compromise is indispensable. Further and providing a clear, easily remembered Medical Education Review Articles 27
and practicable course of action which amenable to defibrillation (approx. 5% – due to their relatively high oxygen con-
is its greatest quality. It is as such that of cases) underscores this mechanism. sumption and small pulmonary residual
these guidelines offer an essential con- volume relative to body weight – the
tribution to safe paediatric emergency Due to the typical pathophysiology reserve in children is small and they will
care. of cardiac arrest, oxygenation and suffer a decrease in oxygen saturation
Based on the aforementioned prerequi- ventilation are the most important within seconds following respiratory
sites, this review takes into account measures in paediatric resuscitation. arrest. On the other hand, the anatomy
the feasibility and effectivity of recom- is advantageous when compared with
mended measures and adjuvants. Those that of the adult, with the larynx situated
• As demonstrated by clear evidence
measures which are either indispensable relatively higher and a factually difficult
and ascertained by all international
(e.g. intraosseous access) or which – airway being rather less common. It has
guidelines, resuscitation of a newborn
whilst requiring only a small effort – been shown that experience and clear
is not possible without successful
would be expected to significantly en- strategies can significantly increase
ventilation, and chest compressions
hance the safety of paediatric emergency safety when managing the paediatric
without ventilation are actually
care (e.g. the laryngeal mask airway) airway.
neither helpful nor indicated [10,11].
are emphasised. A potential desire for • Whilst, at least for lay persons Airway management
paediatric emergency care to be rendered providing telephone-guided aid, Only approximately 5% of prehospital
solely by designated experts in the field resuscitation of adults may be emergencies in Germany involve chil-
is surely an example of the opposite – a performed forgoing ventilation and dren, and of those only approximately
measure requiring insurmountable effort, providing chest compressions only 5% require endotracheal intubation.
especially considering that the required [12], the resuscitation of children Therefore, statistically speaking, emer-
number of experts couldn’t even be pro- has been shown to be associated gency physicians will perform prehos-
vided. Good preparation in a “protected with a significantly higher rate of pital endotracheal intubation of a child
environment” (e.g. simulated scenarios), survival with good neurological once every 3 years, and of an infant once
knowledge of current, simple, structured every 13 years [1].
outcome when lay persons provide
guidelines and the use of adjuvants
chest compressions and rescue
enable non-specialised emergency phy-
breaths [13]. Airway management routine cannot
sicians to provide safe care [7].
• A further observational study involv- be established only by experience as
ing prehospital paediatric resus an emergency physician.
Typical challenges citation also showed conventional
resuscitation incorporating ventilation
Even in paediatric emergency depart-
Oxygenation to be superior. A relatively small
ments, emergency intubation performed
Significance of ventilation for paediatric group of children who received only
by paediatric medical staff was asso-
emergencies ventilations without chest com-
ciated with a serious drop in oxygen
pressions showed even better “good
In contrast to adult resuscitation, in saturation in almost half of the cases. 2
neurological” outcomes [14]. This
which cardiac arrest mostly arises from out of 116 children even suffered hy-
group was too small to deliver a
a cardiac incident, in children and poxic cardiac arrest [15]. Prehospital
statistically definitive result, but the
especially in a prehospital environment, intubation associated with a lower rate
finding underscores the importance
respiratory causes are usually foremost of complications and higher rate of suc-
of ventilation for the survival of
[8]. Here, cardiac arrest is typically the cess can only be achieved by physicians
children even outside the neonatal
result of a respiratory incident leading to who intubate children on an everyday
period.
myocardial hypoxia. Whilst in an ideal basis. It is for these reasons that the ERC
• In addition, clinical experience shows
scenario, adults whose cardiocirculatory guidelines note that only those who have
very clearly that infants and toddlers
arrest due to ventricular fibrillation is safe command of drugs required for
rapidly terminated by defibrillation cannot be resuscitated without
intubation and are proficient in preoxy-
won’t necessarily suffer tissue hypoxia, ventilation. As such, measures and genation and intubation should consider
the respiratory cause of cardiac arrest adjuncts which enable safe ventilation prehospital intubation [6]. In all other
in children means that serious organ of children are indispensable and, cases supraglottic airways should be
damage has already ensued. This is a whilst requiring only a small effort, the airway adjuncts of choice. Under no
major factor in the lower rate of survival have a significant effect on patient circumstances may repeated intubation
in infants following cardiac arrest when survival. attempts be made, as these may lead to
compared with youths or adults [9]. A Even outside of resuscitation, providing prolonged apnoea and can cause swell-
more favourable rate of survival in those oxygenation and ventilation to children ing and bleeding, leading to a total loss
few children presenting a cardiac rhythm takes on a central role. This is because of the airway.28 Review Articles Medical Education
A prehospital trial involving more than Working Group for Paediatric Anaes- recommendation that invasive tech-
800 children suffering grave conditions thesia (WAKKA) of the German Society niques (cricothyrotomy, tracheotomy,
(cardiac arrest, multiple trauma, head of Anaesthesiology and Intensive Care surgical airway) are never required.
injuries) failed to show any difference in (DGAI) [17]. However, the authors are Needle cricothyrotomy cannot real-
the survival rate or neurological outcome of the opinion that laryngoscopy should istically be performed on infants and
between those primarily successfully be performed at an early stage of man- toddlers as the location coincides with
intubated and those who were mask agement, especially in a prehospital the narrowest section of the paediatric
ventilated [16]. Seeing then that even setting. This way airway obstruction airway and the short neck forces the
successful intubation cannot positively by a foreign body or secretions can operator to adopt a very steep approach
influence the outcome, the rationale be- be detected at an early phase. It is not [18, 19]. If anything, needle tracheot-
hind intubation needs to be questioned. necessary to force the laryngoscope into omy, which likewise is difficult, should
However, mask ventilation by itself is a deep position as for intubation; instead be attempted; the procedure is possible
certainly also not an ideal ventilation it can be sufficient simply to open and with a less steep approach, and the
light up the mouth, making it possible tracheal lumen is wider at this location
strategy in a prehospital setting; it binds
to detect the aforementioned compli- [20]. If at all possible, however, surgical
at least one person continuously and can
cations, suction the airway or remove a tracheotomy – a procedure which can be
be difficult to perform. At that point at
foreign body using Magill forceps. performed by an experienced surgeon
the latest, the use of a supraglottic airway
(including paediatric surgeons) within
is required.
a small number of minutes – should be
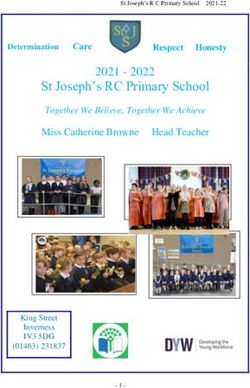
For situations when mask ventilation is It is extremely unlikely that, follow-
preferred [21].
not successful, a clear and simple strat- ing immediate and complete imple-
mentation of the measures set out, The laryngeal mask airway (LM) is the
egy needs to be available for immediate airway adjunct which has been most
ventilation should remain impossible
recall and easy implementation (Fig. 1). thoroughly examined in good clinical
by the point at which a laryngeal
The measures set out should be es- trials for both elective and emergency
mask airway is used.
calated step by step until ventilation of use, is most commonly used, and as
the child is successful. To a significant such is the supraglottic airway adjunct
extent, the algorithm equates to the Based on their own experience however, which can best be recommended for
recommendations of the Scientific the authors do not share the WAKKA use in children from 1.5 kg body weight
(BW) upwards [22]. Evidence for the
use of the laryngeal tube (LT) is not
Figure 1
comparable and consists solely of a
small number of studies demonstrating
mask ventilation impossible
successful use in children from 10 kg
body weight upwards. Despite this
fact, the LT is used surprisingly often in
activate CALL FOR HELP prehospital settings. However, according
EMERGENCY PLAN e.g. consultant, medical supervisor
to current consensus reached by numer-
ous professional bodies, provisioning
escalate until ventilation successful
the LT only whilst forgoing the LM as
DIRECT LARYNGOSCOPY the clearly “better” airway adjunct,
remove foreign bodies,
(to exclude e.g. foreign bodies, blood,
treat laryngospasm cannot be recommended. At the same
secrections, swabs, spasm)
time, provisioning both devices (LM and
LT) and thereby promoting confusion,
increasing costs and taking up addi-
1) jaw thrust, two-person mask ventilation, Guedel airway tional space would seem less than ideal
2) increase anaesthetic depth, decompress stomach
3) supraglottic airways (e.g. nasopharyngeal tube, LM) [22]. For a brief period at least, during
4) neuromuscular blockade intubation or when neither an LM nor
5) (careful) intubation attempt an LT are available, sufficient ventilation
6) intubation aids (e.g. video laryngoscope, bronchoscope)
can almost always be provided using a
7) needle tracheotomy (cricothyrotomy)
nasopharyngeal tube (pharyngeal tube;
a nasally inserted tube in the “Wendl
position”) whilst manually providing
no success: surgical airway
closure of the mouth and contralateral
Algorithm for the management of difficult mask ventilation in a child.
nostril. It is imperative that all the afore-
mentioned adjuncts and techniques Medical Education Review Articles 29
should be trained in the context of job health require larger fluid volumes. pulse oximeter plethysmograph can
shadowing or through participation in The fluid deficit can be categorised point to serious hypovolaemia.
simulated scenarios before they are used by weighing the child or by clinical Deficits resulting in haemodynamic dis-
in paediatric care. assessment (Tab. 2, taken from [27]). ruption and any other situation in which
In addition, respiratory variation of the blood pressure is insufficient with
Cardiocirculatory support
Blood pressure by age
There is good evidence that age adapted Table 1
normal blood pressure values (Tab. 1) Age adapted blood pressure range (min – max) considered safe [25].
are a sufficient therapeutic goal even in Age group Age adapted blood pressure
emergency situations with increased cer-
Preterms (approximation) Mean arterial pressure = gestational age in weeks
ebral pressure [23] and as such should
systolic pressure mean arterial pressure
be achieved, but not overstepped [24].
It is also clear that failing to reach these Preterms 55 – 75 35 – 45
values can cause serious damage. 0 – 3 months 65 – 85 45 – 55
3 – 6 months 70 – 90 50 – 65
Rational infusion therapy
Adequate fluid therapy is the basis of 6 – 12 months 80 – 100 55 – 65
sufficient circulatory support. To avoid 1 – 3 years 90 – 105 55 – 70
hyponatraemia and cerebral oedema 3 – 6 years 95 – 110 60 – 75
only balanced electrolyte solutions may 6 – 12 years 100 – 120 60 – 75
be used. When treating infants (< 1 year > 12 years 110 – 135 65 – 85
of age), the use of solutions containing
additional glucose (1%) is expedient,
if available in the prehospital setting.
Patient safety considerations, however, Table 2
mean that individual blending of such Estimating fluid loss (dehydration) based on clinical signs [27].
solutions cannot be recommended. Signs and minimal/no slight/medium severe
Instead, intravenous boli of 0.1 – 0.2 g/ Symptoms dehydration dehydration dehydration
kg BW glucose can be used to treat low Weight loss < 3% 3 – 8% ≥ 9%
blood glucose levels, which should be Consciousness, health normal agitated, irritable apathetic,
determined for every infant and when or tired lethargic,
confronted with altered consciousness. unconscious
Drinking normal thirsty, drinks greedily drinks poorly or is
Acetate-based balanced electrolyte unable to drink
solutions are the most suitable fluids Heart rate normal normal to increased tachycardia; severen
for maintenance and fluid replenish- cases: bradycardia
ment. Pulse quality normal normal to decreased weak or not palpable
(comparison of central
vs. peripheral pulses)
Basal requirements can be calculated
Respirations normal normal to deep; deep breathing
using the 4-2-1 rule:
increased resp. rate (acidosis!)
• 4 ml/kg/h for every kg for the first
Eyes normal sunken deeply sunken
10 kg BW,
• 2 ml/kg/h for every kg for the next Tears present reduced none
10 kg BW, Mucosa moist dry desiccated
• 1 ml/kg/h for every additional kg Skin folds smooth delayed smoothing, standing > 2 s
BW. immediately but ≤ 2 s
To balance deficits caused e.g. by preop- Capillary refill normal prolonged (< 3 s) severely prolonged
(> 3 s)
erative fasting, in keeping with the above
Urine production normal reduced oliguria or anuria
recommendation for basal requirements,
the basal requirement for the first hour Fluid loss < 30 mild 30 – 50 > 100
(ml/kg BW)* medium 50 – 100
can be assumed to be a blanket 10 ml/
kg/h [26]. Children suffering exsiccosis Resp.: Respiratory; BW: Body weight;
* for children < 6 years of age; school children and adults require smaller fluid volumes due to their
in the context of vomiting and diarrhoea
smaller extracellular space relative to body weight.
or inadequate fluid intake due to poor30 Review Articles Medical Education
out clear cause should be treated by adrenaline should be carefully titrat- ml, from the 7th year of life on 0.5 to
administration of a 20 ml/kg BW fluid ed and used only in conjunction with 1.0 ml administered intramuscularly
bolus with subsequent re-evaluation an inotropic catecholamine. or intravenously as a single dose…”
[6]. Current knowledge suggests that for Experience suggests that a quarter of this
children with fever and serious infec- dose should be given initially and the
In prehospital situations, safe and rapid
tious disease (e.g. pneumonia, sepsis) drug then titrated according to effect. It
treatment with catecholamines can be
fluid should, when possible, only be is also possible to bolus 0.5 (-1) µg/kg
administered in this fashion once [28] difficult to implement, particularly be
cause drug choice and dose are often adrenaline, whereby the effect is short
and catecholamines introduced early. lived and repeat doses may be required.
Repeated administration may be neces unfamiliar, and dopamine and in some
sary, especially when treating exsiccosis cases syringe drivers, are not routinely
provisioned by emergency services. Injecting the contents of a 1 ml = 1 mg
and hypovolaemia; however, an (ad-
ditional) drop in haemoglobin levels As such, it is necessary to stabilise ampoule of adrenaline into a bottle
through haemodilution should be kept the cardio-circulatory situation during containing 100 ml of isotonic saline
in mind. Whilst the use of colloids is transfer to a paediatric intensive care or (NaCl 0.9%) results in a concentra-
typically not necessary and their value emergency facility using a simple and tion of 10 µg/ml, which can then be
unclear, attempted treatment of an safe concept. Cafedrine/Theodrenaline dosed highly accurately using 1 ml
otherwise unstable circulatory situation (Akrinor®) is an example of a suitable syringes with a 0.01 ml scale.
by admin istration of 5 – 10 ml/kg BW, drug. The manufacturer’s summary of
taking the manufacturer’s recommen- product characteristics recommends the
following doses [43]: “…Children: de- Gaining access for drug administration
dations regarding contraindications and
pending on the severity of the condition, and fluid therapy
maximum doses into account (e.g. 6%
HES 130/0,42: 30 ml/kg), can be justi- in the 1st and 2nd years of life 0.2 – 0.4 Placement of an intravenous catheter
fied [27]. ml, in the 3rd to 6th years of life 0.4 – 0.6 can often be difficult in paediatric emer-
Rational use of catecholamines
The aim of treatment with catechola- Table 3
mines is to re-establish adequate perfu- Prehospital treatment of children with haemodynamic shock using catecholamines.
sion and oxygenation of the organs. A
Type of shock Catechola- Dose Rules of thumb
significant intraindividual variability in mine a) Preparation
pharmacokinetics and -dynamics [29] b) Dosing
and the effect of catecholamines can be c) Escalating treatment
observed in infants and toddlers (due, hypody dopamine 5 – 20 µg/kg/min a) 1 ampoule dopamine 5 ml = 50 mg;
amongst other things, to individual re- namic/ 1 ml = 10 mg + 29 ml NaCl 0.9%
cardiogenic, → 0.33 mg/ml
ceptor density and intracellular response b) rate (ml/h)) = body weight equating to
preterms and
[30,31]). When there is no response to newborns 6 µg/kg/min
treatment, increasing the dose by one c) dobutamine, hydrocortisone, adrenaline
order of magnitude is recommended, hypody dobutamine 5 – 20 µg/kg/min a) 1 ampoule dobutamine 50 ml = 250 mg;
titrating down once an effect ensues [32]. namic/ draw up undiluted → 5 mg/ml
cardiogenic, b) rate (ml/h) = 1/10th body weight age
Another peculiarity when compared to all other age brackets equating to 8 µg/kg/min
the treatment of adults is the use of do- brackets
pamine which, on the basis of available hypovolae- adrenaline 0.05 – 2.5 µg/kg/min a) 1 ampoule adrenaline 1 ml = 1 mg;
data, is still the most commonly used mic 6 ml = 6 mg + 44 ml NaCl 0.9%
catecholamine in newborns, infants and → 0.12 mg/ml
b) rate (ml/h) = 1/10th body weight equating
toddlers [32,33]. Table 3 summarises the to 0.2 µg/kg/min
catecholamine of choice for treatment
septic adrenaline 0.05 – 2.5 µg/kg/min a) 1 ampoule adrenaline 1 ml = 1 mg;
of different types of shock in children 6 ml = 6 mg + 44 ml NaCl 0.9%
based on current guidelines [34–42] and → 0.12 mg/ml
provides “rules of thumb” for prepara- b) rate (ml/h) = 1/10th body weight equating
to 0.2 µg/kg/min
tion of and dosing with syringe drivers. c) noradrenaline carefully titrated, only if
extremities warm
Even for septic shock, noradrenaline additionally, noradrena- 0.05 – 2.5 µg/kg/min a) 1 ampoule Noradrenalin 1 ml = 1 mg;
is not the catecholamine of choice in as required: line 6 ml = 6 mg + 44 ml NaCl 0.9%
→ 0.12 mg/ml
children because the increase in af- b) rate (ml/h) = 1/10th body weight equating
terload rapidly leads to a decrease to 0.2 µg/kg/min
in contractility [32]. As such, nor Medical Education Review Articles 31
gencies and may be impossible in some ministration of drugs, and most which point on overdosing adrenaline is
circumstances, e.g. exsiccosis or cardiac drugs achieve bioavailability similar potentially fatal, there is no doubt that
arrest. In prehospital emergencies of this to that following intravenous admin- overdosing by an order of magnitude
kind, placement of a central venous line istration. (1,000% of the recommended dose;
is inarguably not a suitable alternative. 100 µg/kg BW) is not compatible with
survival [47]. All international guidelines
Doses similar to those used for intra-
The intraosseous (IO) needle is a warn explicitly of overdosing adrena
venous administration can often be
quick, easy and safe adjunct for ac- line during resuscitation of paediatric
used for intranasal administration. The
cess to the vascular system. patients of any age. Vigilance derived
total should always be split across both
simply from awareness of the danger
nostrils so as to utilise the maximum
and recognition of personal fallibility is
Complications are rare and are only possible mucosal surface. Administered
pivotal for drug safety [48].
to be expected when the needle remains volumes should preferably be 0.2 – 0.3 ml
in situ for prolonged periods of time. The per nostril and should not exceed 1 ml. Using simple measures can help achieve
current ERC Guidelines recommend the Copious quantities of secretions or blood a significant increase in drug safety when
use of an IO needle in all critically ill can inhibit adequate resorption from the caring for children [49,59].
children in whom venous access has not nose, making cleansing or selection of an
been able to be established within one alternative method necessary. Published It can safely be assumed that any
minute [6]. The most suitable and typi- experience is available especially for measure which reduces the cogni-
cal location in children is the proximal • midazolam tive load of the prescribing physician
anterior tibia. Use of IO needles can • fentanyl will increase drug safety in children.
be trained using chicken bones, which • sufentanil
provide for very realistic conditions. • ketamine and
It is essential that training should take In a test of written orders for adrenaline
• dexmedetomidine administration for resuscitation, for ex-
place before taking on work in emer-
gency care. Intraosseous drills (EZ-IO®, ample, use of a simple table was shown
Drug safety in paediatric emergency
Teleflex), which are widely available in to avoid nine out of ten single order of
care
Germany, are not suitable for newborns magnitude errors, and the same fraction
and small infants weighing less than 3 kg. of errors by two orders of magnitude
Grave errors occur regularly during
The tibial spongiosa is so shallow in [51]. A similar effect was also seen
paediatric emergency care, even in
these children that there is a risk the when the Paediatric Emergency Ruler
specialised facilities such as paediat-
posterior cortex could be pierced, lead- (“PädNFL”; “Pädiatrisches Notfalllineal”;
ric emergency departments.
ing to serious damage or even re- www.notfalllineal.de) was used during
quiring amputation of the lower leg treatment of “real” prehospital paediat-
[44]. Instead, suitable manual needles Because suitable doses have to be cal- ric emergencies: nine out of ten severe
need to be provisioned. The authors culated on an individual basis, mistakes dosing errors (> 300% of the recom-
have had very good experience using such as misplacing the decimal point can mended dose) of all drugs studied were
18 g butterfly needles in these situations, lead to results which are off by an order avoided [52]. With regard to adrenaline,
as is also recommended elsewhere of magnitude. Whilst typical doses feel which was overdosed by more than
[45]. They can easily be gripped by the familiar when treating adults, the wide 300% of the recommended dose in all
wings, are very sharp and have a tube range of paediatric patients – ranging from cases where the PädNFL was not used,
attached, simplifying the use. infants to youths – precludes familiarity no mistakes were made when using the
For on-off administration of sedatives with correct doses. Even doses off by an PädNFL.
and analgesics, the intranasal route us- order of magnitude can be serviced from Body weight is a deciding factor for drug
ing an atomiser (“mucosal atomization a single ampoule, making recognition administration and must, as such, be
device” – MAD) is an option. The intense of the error less likely. Because prehos taken into meticulous consideration. In
vascularisation of the nasal mucosa and pital care is neither rendered in a spe- a prehospital analysis in Germany only
the close proximity to the brain lead to a cialised environment, nor by specialised 0.5% of emergency physicians’ records
rapid onset of action comparable with personnel [6], significantly increased specified the weight of the child [52].
that following intravenous administra- error rates are incurred. A study in the If the parents can give the weight of
tion. USA showed that adrenaline was ad- the child, that weight should be used.
ministered incorrectly 60% of the time, When the weight is unknown however,
Owing to venous drainage avoiding and that the average overdose was 808% estimates based on age are unhelpful
liver passage, first-pass metabolism of the recommended 10 µg/kg BW and weight should be estimated based
does not occur following nasal ad- dose [46]. Whilst it is not known from on length.32 Review Articles Medical Education
Team communication is pivotal. Regard- lymphadenopathy in the context of ing external signs (such as bruising or
less of any hierarchy, all those involved infection, and unexplained events are neurological symptoms). For this reason,
must check every order in its entirety described below. serious trauma requires neurocranial
(weight of the child, desired dose per imaging, preferably in a paediatric
Trauma
kg BW, calculated dose and quantity to radiology department. Prior to fusion
be administered) and acknowledge it by Most injuries are isolated to a single ex- of the fontanelles, ultrasound is a rapid,
repeating the entire order before a drug tremity. The same basic principles used radiation-free imaging tool, while all
is administered [53]. When 1 ml syringes in adult trauma care should be applied, other children with a score of < 12 on
with a 0.01 ml scale are used, dilution adequate analgesia provided, and the the Paediatric Glasgow Coma Scale
can be avoided for most drugs so long injury stabilised carefully. Using sup- should undergo computed tomography
as administration is followed by flushing positories in an emergency situation is (CT) or magnetic resonance imaging
with NaCl 0.9%. Every emergency unlikely to provide a rapid and adequate (MRI). Bony injuries are better seen
physician should have paediatric phar- effect. Instead, administering opioids on CT, whilst brainstem injuries and
macologic information (e.g. age-specific such as fentanyl via a nasal atomiser [54] haemorrhage are better represented on
contraindications and doses) at their or using one of the alternatives set out in MRI. Subgaleal haemorrhage represents
disposal on scene, e.g. in the shape of a Table 4 [55] is well suited. a special type of head injury which
tabular compilation or pocketbook. does not occur in adults, and which
As a rule, care for children with mul- involves haemorrhage between the scalp
Common paediatric disorders tiple trauma follows the same basic and the calvaria. As the haematoma may
Preliminary remarks principles which apply to adult care spread around the whole head, blood
[56]. loss may become life-threatening and
must be recognised as such, triggering
The three most common prehospital
blood transfusion if required. External
paediatric disorders, each account-
Owing to their proportions and skeletal compression is not helpful, and obsolete
ing for approximately a third of cas-
development, however, up to 90% in the case of open fontanelles. Those
es, are injuries, respiratory disorders
of children with serious injuries also providing prehospital care should be
and seizures.
have head injuries, while the chest and aware of subgaleal haemorrhage and
abdomen are less commonly affected include assessment for this injury in their
In addition to these three, intussuscep- when compared with adults. It is note trauma evaluation, which would other-
tion (which does not occur in adults), worthy that children may regularly suffer wise be comparable with an appropriate
abdominal pain caused by systemic serious intracranial injury without show- adult routine. In contrast, pelvic fractures
leading to significant blood loss do not
occur in toddlers.
Table 4
Examples of suitable prehospital emergency analgesia. Respiratory emergencies
Asthma
Drug, mode of delivery Dose, Dosing interval
Sudden occurrence of dyspnoea with an
Piritramide (e.g. Dipidolor)
• IV 0.05 – 0.1 mg/kg BW initial bolus expiratory stridor and prolonged expira-
0.025 mg/kg BW every 5 min until pain free tion should bring a diagnosis of asthma
Morphine to mind. In addition to auscultation,
• IV 0.05 – 0.1 mg/kg BW initial bolus the smaller the child, the more helpful
0.025 mg/kg BW every 5 min until pain free laying hands on the chest can be – bron-
Fentanyl (ampoules containing 50 µg/ml) chospasm, secretions, consolidation and
• IV 1 – 2 µg/kg BW initial bolus the breathing pattern can all be felt and
0.25 µg/kg BW every 5 min until pain free
• intranasal using MAD 1.5 µg/kg BW (0.03 ml/kg BW) localised. Therapeutic measures (Tab.
5) don’t differ from those employed in
Esketamine (e.g. Ketanest S, ampoules
containing 5 mg/ml or 25 mg/ml) adults [7], and inhaled therapies don’t
• rectal 10 mg/kg BW require age-based dose adjustment.
• IV 0.5 – 1 mg/kg BW
• intranasal using MAD 2 mg/kg KG Croup syndrome (stenosing laryngo
Ketamine (e.g. Ketamin, ampoules tracheitis)
containing 10 mg/ml or 50 mg/ml) Sudden occurrence of an inspiratory
• rectal 15 – 20 mg/kg BW
stridor together with a barking cough
• IV 1 – 2 mg/kg BW
• intranasal using MAD 4 mg/kg BW is usually caused by Croup syndrome
which generally arises in conjunction
MAD: mucosal atomization device (nasal atomiser).
with viral infections, but which may Medical Education Review Articles 33
Table 5 a smooth surface in a restive situation.
Pharmacological treatment for asthma attacks (from [7]). Initially, the foreign body enters the
trachea, causing an impressive bout of
Nebulised treatment coughing, expelling the foreign object.
Epinephrine (e.g. Infectokrupp®) up to 10 kg BW: 1 ml + 1 ml NaCl 0.9 % If instead the foreign body reaches the
(= 4 mg) from 10 kg BW: 2 ml undiluted (= 8 mg) bronchial system, the child’s condition
Salbutamol nebuliser solution (e.g. Sultanol® 5 – 10 drops (= 1.25 – 2.5 mg) will commonly improve [57]. However,
sol.) (1 drop per year or 3 kg BW, minimum 3,
in the course of things, the object may
maximum 10 drops) in 2 ml NaCl 0.9%
dislocate into the trachea causing a
Ipratropium bromide solution (z. B. Atrovent® 5 – 10 pumps (= 0.125 – 0.25 mg)
life-threatening situation. As such,
sol.) Dose as for salbutamol, in 2 ml NaCl 0.9%
following aspiration, children should
Inhalation using a spacer
always present to a competent hospital
Salbutamol (e.g. Sultanol®) 1 – 2 puffs (0.1 – 0.2 mg) where any suspicion of aspiration should
Fenoterol (e.g. Berotec®) 1 – 2 puffs (0.1 – 0.2 mg) be investigated by bronchoscopy. Chest
Terbutaline (e.g. Bricanyl®) 1 – 2 puffs (0.25 – 0.5 mg) radiographs on the other hand do not
Corticoids provide any helpful information [57].
Methylprednisolone (e.g. Urbason®) 2 – 4 mg/kg BW IV In the case of an unconscious child, the
Prednisolone (e.g. Decortin H , Solu
®
2 – 10 mg/kg BW IV oral cavity must be inspected and swept
Decortin®) without delay, followed immediately by
Prednisone (e.g. Decortin®, Rectodelt®) 5 – 10 mg/kg BW (usually 100 mg) per rectum measures as set out in the resuscitation
β2 mimetics IM
guidelines. These describe in detail the
measures to be taken in case of foreign
e.g. Epinephrine or Terbutaline 10 µg/kg BW (max. 300 µg)
body aspiration (including, amongst
Additional Options
other things, the Heimlich manoeuvre
Magnesium, Ketamine, Theophylline and back blows) [6]. The oral cavity
should be inspected using a laryngo-
scope as soon as possible, removing any
occur spontaneously, and which in ever, unlike Croup syndrome, children visible foreign objects. If the condition
turn is caused by subglottic swelling of with epiglottitis show signs of serious does not improve, the child should be
mucous membranes. Croup is seldom bacterial infection including high fever intubated. If ventilation is not possible
threatening and can be treated in an and notable poor general condition. via the correctly situated tube, attempts
equivalent fashion to asthma. The differ- Preclinical intubation should only be should be made to push the foreign body
ential diagnoses include tracheitis and attempted in dire straits and can be into one or the other main bronchus
epiglottitis (see below), both of which extremely problematic in the presence by intentional deep insertion of the
can be differentiated from Croup by a of purulent swelling of the epiglottis. The tube, following which ventilation of the
prolonged progressing course and high receiving hospital should be informed unrestricted lung should be performed
fever. In unvaccinated children espe- of the suspected diagnosis as early as after retracting the tube into the trachea.
cially, hoarseness, inspiratory stridor and possible so as to be able to have an ex- If the aforementioned measures are not
a barking cough – which can typically perienced team available for the patient successful, success is not to be expected
be triggered by applying pressure on on arrival. Tracheitis, which cannot be and the child should be transferred to
the tongue using a spatula – progressing differentiated from epiglottis clinically, hospital undergoing ongoing resusci-
over days may indicate diphtheria, a has become the most common form of tation, where the foreign body can be
disease once referred to as “real Croup”. life-threatening respiratory tract infec- removed from the trachea.
tion. The diagnosis can only be made by Seizures
Epiglottitis, Tracheitis
bronchoscopy. As a rule, these children Although seizures in children are usually
Since the introduction of the Haemophi-
can be intubated without difficulty; even febrile, other possible causes must be
lus influenza B vaccination, epiglottitis
so, intubation should be performed considered:
has become extremely rare, but does still
using a fibreoptic scope, taking samples • hypoglycaemia
occur because not all parents go through
and ensuring precise placement of the • intoxication
with recommended vaccinations – but
tube at the same time. • head injury
also because other pathogens can be
causative. The clinical picture seen Foreign body aspiration Meningitis must be excluded in infants
in epiglottitis is similar to that seen in Foreign body aspiration typically occurs suffering a febrile seizure without an
croup syndrome and is characterised by when a playing child inserts something obvious focus of infection. Repeated
inspiratory stridor and coughing. How- into their mouth or eats something with application of rectal drugs, which are34 Review Articles Medical Education
difficult to control and have a delayed risk of necrosis of the affected portions rare. Adherence to guideline-recom-
onset of action, can cause overdose and of the intestines when untreated. The mended treatment of BRUE requires the
respiratory depression. As such, the use diagnosis is made using sonography and emergency services to present children
of drugs and routes of administration set treatment by reduction of intussuscep- for treatment by a consultant paedi-
out in Table 6, leading to a rapid onset tion by insufflation of air or fluid can be atrician at a children’s hospital [58].
of action, would seem better suited [7]. provided by the radiology department of Following thorough examination by the
any paediatric hospital. paediatrician, immediate discharge from
Abdominal lymphadenopathy and
Unexplained events hospital may be justified.
intussusception
Regardless of the focus of infection, Emergency services are regularly con- The role of parents during emer-
toddlers regularly suffer swelling of fronted with reports of events perceived
gency care
the abdominal lymph nodes, causing to be life-threatening, whilst the elicited
abdominal pain. This can lead to an history doesn’t provide for clear-cut Presence of parents
erroneous diagnosis of an abdominal deductions and the child presents itself
disorder, which in turn can sometimes in good health. Formerly an apparent Whenever possible, parents should
even culminate in unwarranted surgery. life-threatening event (ALTE), this have the opportunity to be present
expression has been replaced by the during treatment of their children.
term brief resolved unexplained event
Children complaining of abdominal
(BRUE). This nomenclature was chosen
pain must always be investigated for On one hand, parents are generally well
so as to include events which had
a focus of infection outside the ab- informed of the past medical history of
not been interpreted as life-threatening.
domen, e.g. by auscultation of the their child, can tell the precise weight
Despite this, the term still defines a
lungs and inspection of the tympanic and offer the only possibility to elicit a
condition involving a change in
membranes. history. On the other hand, it has been
• muscle tone
shown time and again that relevant
• skin colour
• consciousness psychopathologies are significantly less
The swollen abdominal lymph nodes
• and/or breathing. common in parents who were present
may, however, actually cause a real
for at least some of the treatment of their
abdominal emergency, namely intus- A working diagnosis of BRUE is only child, even when the child died. As such,
susception. This usually occurs at the permissible if a detailed history and
the resuscitation guidelines recommend
ileocecal junction and involves parts of examination by a paediatrician shows
parents should be given the opportunity
the intestine folding into one another, no further irregularities. Colloquially, the
to be present during treatment of their
typically triggering abrupt, severe spas- term “unexplained event” is often used.
child, so long as their presence does not
modic pain. Bloody diarrhoea may also Generally speaking, these events have a
impact on the quality of medical care
occur. Spontaneous reduction of intus- multitude of possible causes, including
[6].
susception can occur, although delaying gastroesophageal reflux, seizures and
treatment whilst hoping for spontaneous upper respiratory tract infections. Cardi- Child abuse and neglect
resolution is not permissible as there is a opulmonary causes, however, are very It should not be overlooked, however,
that parents may play a role in or be
the cause of the illness or injury. Parents
Table 6
smoking at home, for example, may be
Pharmacological treatment for seizures.
the sole cause of asthma in their child.
Sublingual tablets To an often underestimated degree,
Lorazepam (e.g. Tavor® Expidet®) < 0.05 mg/kg BW administered as a sublingual children may be the victims of violence
tablet or neglect. The most recent available
Intranasal administration figures show an incidence of 10 – 15%
Midazolam* (e.g. Buccolam®, Dormicum®) 0.2 mg/kg BW (maximum 10 mg) in Germany, although a significant dark
figure has to be assumed. A review article
Lorazepam (e.g. Tavor® pro injectione) 0.1 mg/kg BW (maximum 4 mg)
looking at head injuries in children
Intravenous drug administration
determined that a quarter of all injuries
Clonazepam (e.g. Rivotril®) 0.05 – 0.1 mg/kg BW IV (max. 2 mg) in children under 2 years of age were
Midazolam (e.g. Dormicum®) 0.1 – 0.2 mg/kg BW IV or intranasal inflicted by others [59]. Recognising
Diazepam (e.g. Valium®) 0.05 – 0.2 mg/kg BW IV abuse gains particular importance with
Thiopental (e.g. Trapanal®) 1 mg/kg BW IV the knowledge that violence and abuse
are commonly not single occurrences
* midazolam solutions for IV administration cause smarting when administered intranasally.
but rather not only repeat themselves Medical Education Review Articles 35
but escalate. This does not mean that Epistry-Cardiac Arrest. Circulation 19. Navsa N, Tossel G, Boon JM: Dimensions
the worst should always be assumed of 2009;119:1484–1491 of the neonatal cricothyroid membrane –
parents or that forensic aspects should 10. Wyllie J, Bruinenberg J, Roehr CC, how feasible is a surgical cricothyroidot-
Rüdiger M, Trevisanuto D, Urlesberger omy? Paediatr Anaesth 2005;15:402–406
dictate treatment. Nevertheless, simple
B: European Resuscitation Council 20. Johansen K, Holm-Knudsen RJ, Charabi
attentive observation and recording
Guidelines for Resuscitation 2015. B, Kristensen MS, Rasmussen LS: Cannot
of attendant circumstances can offer a Section 7. Resuscitation and support of ventilate-cannot intubate an infant: surgi-
chance to free the child from a spiral of transition of babies at birth. Resuscitation cal tracheotomy or transtracheal cannu-
abuse through a process managed by a 2015;95:249–263 la? Paediatr Anaesth 2010;20:987–993
family court after completion of medical 11. Wyckoff MH, Aziz K, Escobedo MB, 21. Holm-Knudsen RJ, Rasmussen LS,
care (further reading regarding the legal Kapadia VS, Kattwinkel J, Perlman JM, Charabi B, Bøttger M, Kristensen MS:
framework and suitable course of action et al: Part 13: Neonatal Resuscitation: Emergency airway access in children –
is provided by [60]). 2015 American Heart Association transtracheal cannulas and tracheotomy
Guidelines Update for Cardiopulmonary assessed in a porcine model. Pediatric
Resuscitation and Emergency Anesthesia 2012;22:1159–1165
References Cardiovascular Care. Circulation 22. Hoffmann F, Keil J, Urban B, Jung P,
2015;132:S543–560 Eich C, Schiele A, et al: Interdisziplinär
1. Eich C, Roessler M, Nemeth M, konsentierte Stellungnahme:
12. Hupfl M, Selig HF, Nagele P: Chest-
Russo SG, Heuer JF, Timmermann Atemwegsmanagement mit supra-
compression-only versus standard
A: Characteristics and outcome of glottischen Atemwegs hilfen in der
cardiopulmonary resuscitation: a me-
prehospital paediatric tracheal intuba- Kindernotfallmedizin. Larynxmaske ist
ta-analysis. Lancet 2010;376:1552–1557
tion attended by anaesthesia-trained State-of-the-art. Anästh Intensivmed
emergency physicians. Resuscitation 13. Kitamura T, Iwami T, Kawamura T,
Nagao K, Tanaka H, Nadkarni VM, 2016;57:377–386
2009;80:1371–1377
et al: Conventional and chest-com- 23. Chambers IR, Jones PA, Lo TY, Forsyth
2. Zink W, Bernhard M, Keul W, Martin E, RJ, Fulton B, Andrews PJ, et al: Critical
pression-only cardiopulmonary
Volkl A, Gries A: Invasive techniques in
resuscitation by bystanders for children thresholds of intracranial pressure and
emergency medicine. I. Practice-oriented
who have out-of-hospital cardiac cerebral perfusion pressure related to
training concept to ensure adequately
arrests: a prospective, nationwide, age in paediatric head injury. J Neurol
qualified emergency physicians.
population-based cohort study. Lancet Neurosurg Psychiatry 2006;77:234–240
Anaesthesist 2004;53:1086–1092
2010;375:1347–1354 24. Catala-Temprano A, Claret Teruel G,
3. Lammers R, Byrwa M, Fales W: Root
14. Goto Y, Maeda T, Goto Y: Impact of Cambra Lasaosa FJ, Pons Odena M,
causes of errors in a simulated prehos-
dispatcher-assisted bystander cardiopul- Noguera Julian A, Palomeque Rico
pital pediatric emergency. Acad Emerg
monary resuscitation on neurological A: Intracranial pressure and cerebral
Med 2012;19:37–47
outcomes in children with out-of-hos- perfusion pressure as risk factors in
4. Heimberg E, Heinzel O, Hoffmann F: children with traumatic brain injuries.
Typical problems in pediatric pital cardiac arrests: a prospective,
nationwide, population-based cohort J Neurosurg 2007;106:463–466
emergencies: Possible solutions.
study. J Am Heart Assoc 2014;3:e000499 25. Coté CJ, Lermann J, Todres ID: A practice
Med Klin Intensivmed Notfmed
15. Kerrey BT, Rinderknecht AS, Geis GL, of anesthesia for infants and children.
2015;110:354–359
Nigrovic LE, Mittiga MR: Rapid sequence 4th Edition. Philadelphia: Saunders 2009
5. Bankole S, Asuncion A, Ross S, Aghai Z,
intubation for pediatric emergency 26. Sümpelmann R, Becke K, Brenner S,
Nollah L, Echols H, et al: First responder
patients: higher frequency of failed Breschan C, Eich C, Höhne C et al: S1-
performance in pediatric trauma: a
comparison with an adult cohort. Pediatr attempts and adverse effects found by Leitlinie: Perioperative Infusionstherapie
Crit Care Med 2011;12:e166–170 video review. Ann Emerg Med 2012;60: bei Kindern. Anästh Intensivmed
251–259 2016;57:368–376
6. Maconochie IK, Bingham R, Eich C,
López-Herce J, Rodríguez-Núñez A, 16. Gausche M, Lewis RJ, Stratton SJ, Haynes 27. Osthaus W, Ankermann T, Sümpelmann
Rajka T, et al: European Resuscitation BE, Gunter CS, Goodrich SM, et al: Effect R: Präklinische Flüssigkeitstherapie
Council Guidelines for Resuscitation of out-of-hospital pediatric endotracheal im Kindesalter. Pädiatrie up2date
2015. Section 6. Paediatric life support. intubation on survival and neurological 2013;08:67–84
Resuscitation 2015;95 223–248 outcome: a controlled clinical trial. 28. Duke T: New WHO guidelines on emer-
7. Kaufmann J, Laschat M, Wappler F: Die Jama 2000;283:783–790 gency triage assessment and treatment.
präklinische Versorgung von Notfällen 17. Weiss M, Schmidt J, Eich C, Stelzner J, Lancet 2016;387:721–724
im Kindesalter. Anästh Intensivmed Trieschmann U, Müller-Lobeck L et al: 29. Banner W, Jr., Vernon DD, Minton SD,
2012;53:254–267 Handlungsempfehlung zur Prävention Dean JM: Nonlinear dobutamine phar-
8. Turner NM: Recent developments in und Behandlung des unerwartet schwier- macokinetics in a pediatric population.
neonatal and paediatric emergencies. igen Atemwegs in der Kinderanästhesie. Crit Care Med 1991;19:871–873
Eur J Anaesthesiol 2011;28:471–477 Anästh Intensivmed 2011;52:S54–S63 30. Artman M, Kithas PA, Wike JS, Strada
9. Atkins DL, Everson-Stewart S, Sears GK, 18. Cote CJ, Hartnick CJ: Pediatric transtra- SJ: Inotropic responses change during
Daya M, Osmond MH, Warden CR, et cheal and cricothyrotomy airway devices postnatal maturation in rabbit. Am J
al: Epidemiology and outcomes from for emergency use: which are appro- Physiol 1988;255:H335–342
out-of-hospital cardiac arrest in children: priate for infants and children? Paediatr 31. Papp JG: Autonomic responses and
the Resuscitation Outcomes Consortium Anästh 2009;19 Suppl 1:66–76 neurohumoral control in the human36 Review Articles Medical Education
early antenatal heart. Basic Res Cardiol Refresher Course der DAAF 54. Borland M, Jacobs I, King B, O‘Brien D:
1988;83:2–9 2008;34:193–204 A randomized controlled trial comparing
32. Shukla A, Steven JM, McGowanJr. FX: 43. Fachinformation Akrinor, Firma AWD intranasal fentanyl to intravenous
Cardiac Physiology an Pharmacology. Pharma, Dresden. Stand Juli 2001 morphine for managing acute pain in
In: CJ Coté, J Lerman and ID Todres. A 44. Oesterlie GE, Petersen KK, Knudsen L, children in the emergency department.
practice of anesthesia for infants and Henriksen TB: Crural amputation Ann Emerg Med 2007;49:335–340
children. 4th. Saunders 2009 of a newborn as a consequence of 55. Kaufmann J, Laschat M, Wappler F:
33. Hunt R, Osborn D: Dopamine for intraosseous needle insertion and Analgesie und Narkose im Kindesalter.
prevention of morbidity and mortality calcium infusion. Pediatr Emerg Care Notfallmedizin up2date 2012;7:17–27
in term newborn infants with suspected 2014;30:413–414 56. Kaufmann J: Versorgung des kindlichen
perinatal asphyxia. Cochrane Database 45. Lake W, Emmerson AJ: Use of a butterfly Polytraumas. Anästh Intensivmed
Syst Rev 2002;CD003484 as an intraosseous needle in an oedema- 2010;51:612–614
34. Brissaud O, Botte A, Cambonie G, tous preterm infant. Arch Dis Child Fetal 57. Kaufmann J, Laschat M, Frick U,
Dauger S, de Saint Blanquat L, Durand Neonatal Ed 2003;88:F409 Engelhardt T, Wappler F: Determining the
P, et al: Experts‘ recommendations for 46. Hoyle JD, Davis AT, Putman KK, Trytko probability of a foreign body aspiration
the management of cardiogenic shock in JA, Fales WD: Medication dosing errors from history, symptoms and clinical
children. Ann Intensive Care 2016;6:14 in pediatric patients treated by emergen- findings in children. BJA: British Journal
35. Berner M, Rouge JC, Friedli B: The cy medical services. Prehosp Emerg Care of Anaesthesia 2017;118:626–627
hemodynamic effect of phentolamine 2012;16:59–66 58. Tieder JS, Bonkowsky JL, Etzel RA,
and dobutamine after open-heart 47. Perondi MB, Reis AG, Paiva EF, Nadkarni Franklin WH, Gremse DA, Herman B, et
operations in children: influence of the VM, Berg RA: A comparison of high- al: Brief Resolved Unexplained Events
underlying heart defect. Ann Thorac Surg dose and standard-dose epinephrine in (Formerly Apparent Life-Threatening
1983;35:643–650 children with cardiac arrest. N Engl J Events) and Evaluation of Lower-Risk
36. Dellinger RP, Levy MM, Rhodes A, Med 2004;350:1722–1730 Infants. Pediatrics 2016;137:e1–e32
Annane D, Gerlach H, Opal SM, et al: 48. Kaufmann J, Schieren M, Wappler F: 59. Duhaime AC, Christian CW, Rorke LB,
Surviving sepsis campaign: international Medication errors in paediatric anaesthe- Zimmerman RA: Nonaccidental head
guidelines for management of severe sia-a cultural change is urgently needed! injury in infants – the „shaken-baby
sepsis and septic shock: 2012. Crit Care Br J Anaesth 2018;120:601–603 syndrome“. N Engl J Med 1998;338:
Med 2013;41:580–637 1822–1829
49. Kaufmann J, Wolf AR, Becke K, Laschat
37. Harada K, Tamura M, Ito T, Suzuki M, Wappler F, Engelhardt T: Drug safety 60. Jacobi G, Dettmeyer R, Banaschak S,
T, Takada G: Effects of low-dose in paediatric anaesthesia. Br J Anaesth Brosig B, Herrmann B: Misshandlung
dobutamine on left ventricular diastolic 2017;118:670–679 und Vernachlässigung von Kindern –
filling in children. Pediatr Cardiol Diagnose und Vorgehen. Dtsch Arztebl
50. Kaufmann J, Laschat M, Wappler F:
1996;17:220–225 Int 2010;107:231–239.
Medikamentenfehler bei Kindernotfällen
38. Havel C, Arrich J, Losert H, Gamper G, – eine systematische Analyse. Dtsch
Mullner M, Herkner H: Vasopressors for Arztebl Int 2012;109:609–616
hypotensive shock. Cochrane Database 51. Bernius M, Thibodeau B, Jones A,
Syst Rev 2011;CD003709 Clothier B, Witting M: Prevention of
39. Lampard JG, Lang E: Vasopressors for
Correspondence
pediatric drug calculation errors by
hypotensive shock. Ann Emerg Med prehospital care providers. Prehosp address
2013;61:351–352 Emerg Care 2008;12:486–494
40. Sakr Y, Reinhart K, Vincent JL, Sprung 52. Kaufmann J, Roth B, Engelhardt T,
CL, Moreno R, Ranieri VM, et al: Does Lechleuthner A, Laschat M, Hadamitzky Jost Kaufmann
dopamine administration in shock C, et al: Development and Prospective MD, PhD
influence outcome? Results of the Sepsis Federal State-Wide Evaluation of
Occurrence in Acutely Ill Patients (SOAP)
Kinderkrankenhaus der Kliniken der
a Device for Height-Based Dose
Study. Crit Care Med 2006;34:589–597 Recommendations in Prehospital
Stadt Köln gGmbH
41. Stopfkuchen H, Racke K, Schworer H, Pediatric Emergencies: A Simple Tool Amsterdamer Straße 59
Queisser-Luft A, Vogel K: Effects of dopa- to Prevent Most Severe Drug Errors. 50735 Köln, Germany
mine infusion on plasma catecholamines Prehosp Emerg Care 2018;22:252–259 Phone: +49 0221 8907 15199
in preterm and term newborn infants. 53. Kaufmann J, Becke K, Höhne C, Eich C, Fax: +49 0221 8907 5264
Eur J Pediatr 1991;150:503–506 Goeters C, Güß T et al: S2e-Leitlinie
42. Emmel M, Roesner D, Roth B: – Medikamentensicherheit in der Mail: jost.kaufmann@uni-wh.de
Hypovolämischer Schock – Kinderanästhesie. Anästh Intensivmed ORCID-ID: 0000-0002-5289-6465
Besonderheiten des Kindesalters. 2017;58:105–118You can also read