Association between Use of Spermicide-coated Condoms and Escherichia coli Urinary Tract Infection in Young Women
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
American Journal of Eptdemiotogy Vol. 144, No. 5
Copyright O 1996 by The Johns Hopkins University School of Hygiene and Public Health Printed In U.S.A
All rights reserved
Association between Use of Spermicide-coated Condoms and Escherichia
coli Urinary Tract Infection in Young Women
Stephan D. Finn,1"3 Edward J. Boyko, 1 - 24 Esther H. Normand,5 Chi-Ling Chen,4 Jane R. Grafton,6
Marcia Hunt,5 Patricia Yarbro,5 Delia Scholes,4-5 and Andy Stergachis6
Diaphragm/spermicide use increases the risk of urinary tract infection (UTI). To determine whether spermi-
cide-coated condoms are also associated with an increased risk of UTI, the authors conducted a case-control
study at a large health maintenance organization in Seattle, Washington. Cases were sexually active young
women with acute UTI caused by Escherichia coli, identified from computerized laboratory files during
1990-1993. Age-matched controls were randomly selected from the enrollment files of the plan. Of 1,904
eligible women, 604 cases and 629 controls (65%) were interviewed. During the previous year, 40% of the
cases and 31 % of the controls had been exposed to any type of condom. The unadjusted odds ratio for UTI
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
increased with frequency of condom exposure from 0.91 (95% confidence interval (Cl) 0.65-1.28) for weekly
or less during the previous month to 2.11 (95% Cl 1.37-3.26) for more than once weekly. Exposure to
spermicide-coated condoms conferred a higher risk of UTI, with odds ratios ranging from 1.09 (95% Cl
0.58-2.05) for use weekly or less to 3.05 (95% Cl 1.47-6.35) for use more than once weekly. In multivariate
analyses, intercourse frequency (odds ratio (OR) = 1.14 per weekly episode), history of UTI (OR = 2.64), and
frequency of spermicide-coated condom exposure (OR = 3.34 for more than once weekly and 5.65 for use
more than twice weekly) were independent predictors of UTI. Spermicide-coated condoms were responsible
for 42% of the UTIs among women who were exposed to these products. Am J Epidemiol 1996;144:512-20.
case-control studies; condom; Escherichia coli; spermicidal agents; urinary tract infections
Women who use a diaphragm along with a spermi- have disproved this notion and have suggested that the
cide are at increased risk of acquiring a urinary tract effects of the spermicide on the vaginal flora are the
infection (UTI). Studies from several different coun- dominant factor (8). Diaphragm/spermicide users,
tries employing a variety of different methodologies even those with no history of UTI, typically have
have shown the risk to be approximately two- to higher levels of introital and periurethral colonization
3.5-fold greater than that for sexually active women with uropathogenic organisms than do women using
who were not using a diaphragm (1-7). Initially, the other means of contraception (9-11). The levels of
mechanism of this effect was attributed to ill-fitting colonization approximate those seen in women with
diaphragms that impinged upon the urethra, causing recurrent UTI (12). Among women using spermicidal
obstruction and residual urine. Subsequent studies foam or diaphragm/spermicides, bacteriuria with
Escherichia coli after intercourse is more frequent
Received for publication July 24, 1995, and in final form February (usually in levels of 102 to 103 bacteria per milliliter)
20, 1996.
Abbreviations: Cl, confidence Interval; GHC, Group Health Co-
(13).
operative; N-9, nonoxynol-9; OR, odds ratio; UTI, urinary tract in- Accumulating evidence suggests that spermicidal
fection. agents promote colonization of the vaginal introitus,
1
Northwest Hearth Services Research and Development Reid
Program, Veterans Affairs Medical Center, Seattle, WA an important step in the pathogenesis of UTI, by
2
Department of Medicine, University of Washington, Seattle, altering the normal vaginal flora and enhancing adher-
WA
3
Department of Health Services, University of Washington, Se-
ence of pathogens to the vaginal mucosa (14). In vitro,
attle, WA pharmacologic concentrations of nonoxynol-9 (N-9),
4
Department of Epidemiology, University of Washington, Seat- the most commonly used spermicidal agent in the
tle, WA.
5
Center for Health Studies, Group Health Cooperative of Puget
United States, inhibit the growth of the normal con-
Sound, Seattle, WA stituents of the vaginal flora, i.e., lactobacilli and
6
School of Pharmacy, University of Washington, Seattle, WA Gardnerella vaginalis, while failing to exert a similar
Reprint requests to Dr. Stephan D. Finn, Health Services Re-
search Program, Seattle Veterans Affairs Medical Center (152), 1660 effect on uropathogenic E. coli. Moreover, certain
S. Columbian Way, Seattle, WA 98108. strains of E. coli demonstrate greater adherence to
512Condom Use and Urinary Tract Infection 513
vaginal cells treated with N-9 than to control cells only as many as we expected to be able to interview
(14). Because diaphragm/spermicide users are more within the subsequent 4 weeks. This was done by
prone to UTI, they may also be more easily infected by selecting potential cases consecutively in reverse chro-
organisms that possess fewer virulence factors than the nologic order on the basis of the date of their UTI. We
bacteria that infect women who use other forms of chose cases in this manner to minimize the interval
contraceptives (15). between their UTI and the study interview, thereby
A major current source of exposure to N-9 is via reducing recall inaccuracies (17). The number of po-
condoms coated with this agent. One recent study of tential cases selected each month varied according to
women experiencing a first-time UTI found that the interviewers' schedules and the backlog of subjects
use of a condom within the previous 2 weeks was from the previous month. On average, the size of the
associated with a 43 percent increase in the odds of case group chosen monthly was 75. Women not se-
UTI compared with women using oral contraceptives lected as potential cases at this point were eligible to
or no method of birth control, after adjustment for serve as cases in a subsequent month if they experi-
sexual activity and other confounding factors (16). enced another UTI.
Women who used condoms five or more times during We then reviewed the medical records of potential
the same time period had a fivefold increase in the cases to ascertain whether there was documentation of
odds of UTI. an acute, symptomatic UTI, defined as the presence of
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
Unfortunately, the exposure data from this study dysuria, frequency, or urgency for 2 weeks or less. We
lacked specification regarding spermicide coating. To excluded women whose index culture was obtained
address this question directly, we performed a case- during treatment for a previously diagnosed UTI, who
control study to ascertain the risk of UTI among had asymptomatic bacteriuria, or who had been preg-
women who used spermicide-coated condoms com- nant within the previous year. The remaining women
pared with women who did not use them. We also were eligible for interview. After securing permission
sought to compare the risk of UTI related to condom from their primary physician, we sent a letter describ-
and diaphragm/spermicide use. ing the study, advising that we would call to schedule
an interview, and explaining how to decline participa-
tion.
MATERIALS AND METHODS Selection of controls. From GHC enrollment files,
Study setting and participants we randomly selected women to serve as controls.
The study was conducted at Group Health Cooper- Like cases, controls had to have been GHC enrollees
ative (GHC) of Puget Sound, a staff-model health for the preceding 12 months. Controls were frequency
maintenance organization, that has 380,000 contract matched to cases for date of birth (within 2 years). We
enrollees and is the oldest cooperative health mainte- also reviewed the hospital discharge and laboratory
nance organization in the United States. To aid in files to eliminate women who had a clinical record of
obtaining medical records and reduce the number of having a UTI, had had a urine culture positive for
potential subjects to be screened, we limited eligibility ^ 1 0 5 uropathogenic organisms per milliliter within
to women receiving care in Pierce, King, Thurston, the previous month, or had been pregnant within the
and Snohomish counties in Washington State. There previous year. After receiving permission from their
were approximately 75,600 female GHC enrollees be- primary physician, we also contacted potentially eli-
tween ages 18 and 40 years who obtained care in the gible controls by mail and instructed them on how to
four counties during the period of study, 1990-1993. decline participation.
Selection of cases. Cases were women aged Final selection of cases and controls. Potential
18-40 years who had been members of GHC for at cases and controls who had not notified us that they
least a year and had an acute UTI with E. coli diag- wished to be excluded were contacted by telephone to
nosed within the previous month. Each month, we make a final determination of their eligibility and
reviewed the computerized laboratory files to identify willingness to participate. We made up to 10 attempts
all women who had had a positive urine culture during to reach each woman by telephone. When they were
the preceding month. We defined a positive culture as contacted, we asked potential participants whether
yielding s l O 5 colonies per milliliter. We eliminated they had received materials about the study and con-
women who had received a GHC discharge diagnosis firmed that they had been active members of GHC for
for any condition related to pregnancy or who had had the previous year and had not been pregnant during
a positive pregnancy test within the previous year. that time. We eliminated any women who did not meet
Because the process for identifying cases yielded these eligibility criteria as well as those who no longer
many more individuals than necessary, we selected lived in the area or who told us that they had not been
Am J Epidemiol Vol. 144, No. 5, 1996514 Fihn et al.
sexually active during the previous month. We also sexual partners. We collected detailed information
eliminated women with certain medical conditions, about contraceptive practices during the previous year
including neurologic problems that might interfere and the previous month, including frequency and man-
with voiding, known anatomic abnormalities of the ner of use and specific brands of products used. To
urinary tract, an indwelling urinary catheter, and dia- classify the type of condom used, we inquired about
betes mellitus. whether the product was coated with a lubricant or a
We then described the study procedures, requested spermicide (and specifically, N-9). The interviewers
verbal consent, and scheduled an interview with those used a notebook that listed 107 commercially available
who consented. All procedures used in the study were condoms (18) and provided color photographs of the
approved by the Human Subjects Committees of the packaging for 58 major brands. They used the note-
University of Washington and GHC. book to assist subjects in identifying products by
prompting with brand names and descriptions of pack-
Data collection aging. The interviewer was also asked to record a
subjective judgment about how confident she was
We performed all interviews by telephone with the about the subject's classification regarding exposures
aid of computer software that employed branching to a specific type of condoms.
logic and was programmed to perform automatic range
The final set of questions asked during the interview
checking and examine internal consistency (CLU, Saw-
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
related to the subject's history of previous UTIs. Until
tooth Software, Ketchum, Idaho). The questionnaire
that point, the interviewer was uninformed about
was extensively pretested and revised prior to the
whether she was speaking with a case or a control to
study. During the first and last months of the study, 10
minimize any possible bias in ascertaining the sub-
percent of interviews were monitored by a second
ject's exposure status.
interviewer who simultaneously recorded subject re-
sponses to assess reliability. Interrater reliability ex-
ceeded 98 percent for all items. Analysis
For each group of cases drawn monthly, we estab- Data were analyzed using SAS (SAS Institute, Inc.,
lished a "reference date" that was the midpoint of the Cary, North Carolina) and EGRET (SERC, Seattle,
range of dates on which positive urine cultures were Washington). Bivariate comparisons of characteristics
obtained. For example, during the first week of August by case status were tested for significance using the t
1993, we identified a group of potential cases who had test for continuous variables and the chi-square test for
positive urine cultures in the July laboratory file. categorical variables. Odds ratios and 95 percent con-
Working in reverse chronologic order from July 31st, fidence intervals were calculated using standard meth-
we selected cases on the basis of the date of their urine ods (19).
culture until we reached the 17th of the month. The To adjust for potential confounding factors, we con-
midpoint of this range, July 24th, was designated as structed several logistic models using case/control sta-
the reference date for that month. Each month, this tus as the dependent variable (19). In these models,
date was programmed into the interviewing software condom exposure was treated as either a dichotomous
and used as the point of reference for all questions variable (yes/no) or an ordinal or continuous variable
relating to events during the month prior to the UTI, representing frequency of use. To test for the presence
for example, "In the month prior to July 24th did you of a dose-response relation between frequency of con-
use a diaphragm?" Because we did not perform one- dom use and UTI, we created a set of dummy variables
to-one matching, this permitted us to assign a compa- representing different levels of condom use. Sexual
rable date to cases and controls and ask them identical activity was treated as a continuous variable, coded as
questions. Women in the case and control groups were the frequency per week during the previous month.
interviewed a median of 77 days (mean = 78 days)
and 75 days (mean = 77 days) after the reference date,
respectively. RESULTS
For the entire study, the monthly case samples were With computerized laboratory and administrative
selected from a period extending a mean of 8 days files, 1,394 women were selected as potential cases.
prior to the last day of the month. For the 50 percent Review of their medical records eliminated 405
of UTIs that occurred prior to the reference date, the women as ineligible, yielding 898 whom we attempted
interval averaged 5 days. to contact as cases (table 1). Of the 898, 148 were
During the interview, we asked subjects about their deemed ineligible on the basis of information gathered
general medical, obstetric, and gynecologic history; during the screening interview, leaving a total of 750
recent frequency of sexual activity; and number of eligible cases. We initially identified 1,543 potential
Am J Epidemiol Vol. 144, No. 5, 1996Condom Use and Urinary Tract Infection 515
TABLE 1. Reasons for exclusion of cases and controls, Seattle, Washington, 1990-1993
Cases Controls Total
No. % No. % No. %
Attempted contacts 898 1,543 2,441
Ineligible after interview 148 389 537
Pregnant 40 80 120
Comorbldlty 24 20 44
Virgin 5 46 51
Not sexually active during prior months 60 176 236
Miscellaneous 19 67 86
Unable to contact 48 5.3 184 11.9 232 9.5
Refusals 98 10.9 341 22.1 439 18.0
Total potentially eligible 750 1,154 1,904
Final no. of subjects 604 629 1,233
controls, of whom 389 were found to be ineligible Condoms were the most common method of con-
after interview, leaving 1,154 eligible controls. traception and/or protection from sexually transmitted
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
Eleven percent of the 898 potential cases we at- disease in the study population. They were used during
tempted to contact refused to be interviewed, and we the previous year and the previous month by 40 and 23
could not reach 5 percent (table 1). Twenty-two per- percent of the cases and 31 and 19 percent of controls,
cent of the 1,543 potential controls we tried to contact respectively. Of those who used condoms during the
refused the interview, and 12 percent could not be previous month, 35 percent of cases and 25 percent of
reached. Thus, 604 cases and 629 controls were in- controls reported that they definitely used condoms
cluded in the final analysis, for an overall response coated with N-9. Thirty-four percent of the total study
rate of 65 percent. sample used oral contraceptives during the previous
Cases and controls were similar with regard to age, year, while 39 percent of women or their partners had
ethnic background, education, and self-reported health undergone surgical sterilization, 7 percent used a dia-
(table 2). Cases were more likely than controls to be
phragm, 13 percent practiced the rhythm method, and
unmarried, were more sexually active, and had a more
7 percent used another method.
extensive history of previous UTIs.
TABLE 2. Characteristics of participants, Seattle, Washington, 1990-1993
Cases Controls
(n = 604) (n = 629) P
No. % No. % value
Age (years) ± SE* 32.8 ± 0.25 32.2 ± 0.25 0.07
No. married or living as married 378 62.6 473 75.2516 Fihn et al.
The unadjusted odds ratio for having an acute UTI UTI associated with condom use in the previous year was
among women who had used any type of condom during 1.47 (95 percent CI 1.16-1.85). The highestfrequencyof
the previous month was 1.24 (95 percent confidence condom use during the previous month or year was
interval (CI) 0.94-1.63) (table 3). The odds ratio for a associated with the highest risk of UTI.
TABLE 3. Unadjusted relative odds of urinary tract Infection according to frequency and type of
exposure to condoms coated with nonoxynol-9 or uncoated condoms, Seattle, Washington, 1990-1993
Exposure
No. of No. 0)
OR* 95%CI« P
cases controls value
Any condom use
No use of any condom during previous
year 362 432 Referent
Use of any condom during previous
year 242 197 1.47 1.16-1.85 0.001
No use during previous month 462 503 Referent
Use of any condom during previous
month 139 122 1.24 0.94-1.63 0.123
No use of any condom during previous
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
month 462 503 Referent
Use of any condom £1 time/week
during previous month 71 85 0.91 0.65-1.28 0.584
Use of any condom >1 time/week
during previous month 66 34 2.11 1.37-3.26Condom Use and Urinary Tract Infection 517
To determine whether misclassification due to those whose primary method was oral contraceptives
faulty recall regarding condom use could have biased reported exposure to any type of condom (table 4).
our results, we repeated this analysis using responses The relative risk of UTI related to the use of N-9-
from only the 132 cases and 153 controls for whom the coated condoms exceeded that associated with use of
interviewers felt high confidence in classifying expo- a diaphragm plus spermicide. The unadjusted odds
sure to condoms within the previous year. The odds ratio for acquiring a UTI among women who had used
ratio for UTI among women exposed to condoms a diaphragm during the previous month was 1.24 (95
within the previous year was 1.48 (95 percent CI percent CI 0.77-1.99). The proportion of women using
0.85-2.56). This result is nearly identical to the odds a diaphragm was small, however, and declined
ratio of 1.47 obtained when all women were included. steadily during the course of the study (figure 1).
The unadjusted risk of UTI was also significantly When we adjusted for potentially confounding vari-
elevated for women who specifically reported use of ables, including known risk factors for UTI (i.e., fre-
condoms coated with N-9 during the previous month, quency of sexual activity, history of UTI, and dia-
with an odds ratio of 1.72 (95 percent CI 1.08-2.75) phragm/spermicide use) and age (the matching factor),
(table 3). The highest risk of UTI was again seen with the risk of UTI associated with spermicide-coated
greater exposure to N-9-coated condoms over the pre- condoms was highly significant (OR = 2.42, 95 per-
vious month or year. The odds ratio for women who cent CI 1.45-4.04) (table 5, model 1). In fact, the risk
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
had used N-9-coated condoms one or more times per of UTI among condom users was mainly confined to
week during the previous month was 3.05 (1.47- women exposed to N-9-coated products (table 5).
6.35), higher than the odds ratio of 2.11 for an equiv- Moreover, with increasing use of spermicide-coated
alent level of exposure to uncoated condoms. For condoms during the previous month, the odds ratio for
those exposed to N-9-coated condoms more than twice experiencing a UTI rose significantly (table 5, model
weekly during the previous year, the odds ratio was 2). The odds ratio for use of an N-9-coated condom
2.39 (95 percent CI 1.10-5.16) compared with those two or more times per week during the previous month
unexposed to condoms. When women exposed during was 5.65 (95 percent CI 1.56-20.42).
the previous month to condoms not coated with N-9 hi none of the multivariate models we constructed
were treated as the reference group, the odds ratio of was there a significantly increased risk of UTI among
UTI among women who used N-9-coated condoms in women exposed to condoms not coated with spermi-
the previous month was 1.74 (95 percent CI 0.96- cides compared with controls not using any type of
3.14), while that for women who did not use any type condom. In the stratum of most frequent exposure, the
of condom was 1.01 (95 percent CI 0.68-1.51). This odds ratio associated with use of uncoated condoms
indicates that most of the risk of UTI related to con- more than twice a week was 2.36, but the confidence
dom use could be accounted for by exposure to N-9- intervals were wide and included 1.0. This again sug-
coated condoms. gests that most of the excess risk of UTI among
Most exposure to condoms, including to N-9-coated condom users is related to N-9 exposure. Among study
condoms, occurred among women not using another patients exposed to spermicide-coated condoms during
method of contraception. Less than 3 percent of the the previous month, 41.9 percent of UTIs among in-
women whose primary method of contraception was dividuals were due to coated condoms (attributable
vasectomy or tubal ligation and less than 14 percent of risk percent).
TABLE 4. Other methods of contraception used during previous month according to exposure to condoms coated with
nonoxynol-9 (N-9) and uncoated condoms, Seattle, Washington, 1990-1993
Cases Controls
Other methods
of NoN-9- N-9- NoN-9- N-9-
contraception condom
% coated % coated % Total
condom
% coated % coated % Total
condom condom condom condom
None or rhythm method 39 41 28 30 27 29 94 58 60 24 25 15 15 97
Diaphragm/spermlcide 34 85 3 8 3 8 40 26 90 2 7 1 3 29
Oral contraceptive 150 89 8 5 10 6 168 164 84 19 10 13 7 196
Vasectomy/tubal ligation 235 97 6 2 2 1 243 222 98 4 2 0 0 226
Other vaginal spermicide* 15 79 4 21 0 0 19 10 71 3 21 1 7 13
Other (including intrauterine
device) 5 83 1 17 0 0 6 5 71 2 29 0 0 7
1
Includes spermiddaJ foam, jelly, or contraceptive sponge.
Am J Epidemiol Vol. 144, No. 5, 1996518 Fihn et al.
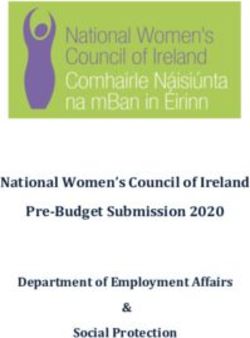
50 vated compared with no use of condoms (OR = 1.18,
• Diaphragm, controls Diaphragm,
• C o n d o m , controls Condom,
95 percent CI 0.89-1.56).
DISCUSSION
hi this large, population-based case-control study,
we observed a highly significant risk of UTT due to E.
coli, the most common cause of UTI, among women
exposed to condoms. The increase in risk of UTI was
restricted to women who used condoms coated with
N-9, the most commonly used spermicidal agent in the
United States. Of the women who participated in this
study, 36 percent had been exposed to a condom in the
previous year and, at a minimum, 29 percent of these
1991 1992 1993 exposures involved spermicide-coated condoms.
Year of Study After adjustment for these potentially confounding
FIGURE 1. Trends in proportion of study subjects using dia- variables, such as frequency of sexual activity, history
phragms/spermicldes and condoms during the course of the study,
of UTT, and use of other contraceptive methods, the
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
Seattle, WA, 1990-1993.
odds of UTI among women exposed to condoms
coated with N-9 were up to three times higher than
those among sexually active women who did not use
Other previously reported risk factors for UTI were coated condoms. The association between risk of UTI
also found to be significant in this study. In several and exposure to N-9-coated condoms was consistent in
multivariable models, the odds ratios of UTI associ- every analysis performed.
ated with the frequency of sexual intercourse per The size and consistency of the observed relation
week, coded as a continuous variable, ranged between between exposure to spermicide-coated condoms and
1.16 and 1.18 with a lower bound to the 95 percent CI risk of UTI and the strong dose-response relation
of 1.06 to 1.08 and an upper bound of 1.23 to 1.25. A suggest a causal relation. This is further supported by
history of a previous UTI was also significantly asso- biologic research showing that N-9 induces changes in
ciated with a heightened risk of UTI, with an odds the normal vaginal flora that facilitate colonization
ratio of approximately 2.65. with coliform bacteria, a circumstance known to pre-
We did not detect an elevated risk of UTI among cede the occurrence of UTI (12). In addition, the
married (vs. single) women, those who had multiple association between use of coated condoms and UTI
sexual partners, or those who had a new sexual part- resembles that already proven between diaphragm use
ner. We did not observe a significantly increased risk and UTI. Diaphragm use is suspected of causing UTI
of UTI among women who had used a cervical cap as a result of the effects of the spermicide used in
during the previous month (OR = 4.0O, 95 percent CI conjunction with the diaphragm (13, 14).
0.27-60.3) or the previous year (OR = 0.57, 95 per- We took a number of precautions to minimize bias.
cent CI 0.18-1.82) in comparison with sexually active Our case definition, acute urinary symptoms plus a
women who were not using condoms, although the culture yielding a l O 5 bacteria per milliliter, is over 95
number of women using a cervical cap was very small. percent specific for the presence of a UTI (20). We
Only a small number of women reported exposure confirmed that all cases met this criterion based on
to a vaginal spermicidal agent other than in association review of data obtained from computerized laboratory
with use of a diaphragm or a coated condom. The odds files, medical records, and subject interviews. To
ratios for UTI among women exposed to spermicidal avoid the biases introduced by using controls drawn
foams, films, creams, suppositories, or sponges during from patients visiting a clinic or hospital, we randomly
the previous month and the previous year were 1.31 selected controls from the entire GHC enrollment base
(95 percent CI 0.67-2.56) and 1.15 (95 percent CI in the four counties studied. Exclusion criteria applied
0.70-1.88), respectively, compared with women who identically to the case and control groups.
reported no spermicide exposure. We strove to minimize recall bias by interviewing
To assess whether the women in the study might cases as soon as possible after the occurrence of their
have confused N-9 coating with regular lubrication of UTI. The interval between the reference date and the
the condom, we inquired about use of lubricated con- study interview was similar for cases and controls.
doms. The odds ratio for use of one of these products Subjects were not informed about the study hypothesis
during the previous month was not significantly ele- and were told only that the investigators were inter-
Am J Epidemiol Vol. 144, No. 5, 1996Condom Use and Urinary Tract Infection 519
TABLE 5. Muttiwiate models of the effect of condom use adjusted for potential confounding factors,
Seattle, Washington, 1990-1993
OR* 95% Cl* P
value
Model 1
Use of condoms during previous month
Any use of N-S^-coated condom 2.42 1.45-^1.04 2 times/week 2.36 0.80-6.96 0.121
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
Use of uncoated condoms >1-2 times/week 0.91 0.38-2.19 0.835
Use of uncoated condoms i 1 time/week 0.91 0.53-1.56 0.739
No condom use Referent
Diaphragm use during previous month 1.43 0.86-2.40 0.170
Frequency of intercourse (timesAveek)t 1.14 1.06-1.23520 Fihn et al.
side pharmacies. Any errors in reporting exposure that The authors thank Dick Rayray for his programming
may have occurred would likely have been nonsys- assistance and Allison McMorris and Lair Showalter for
tematic and would have acted to diminish the observed helping to perform interviews.
association between the use of spermicide-coated con-
doms and UTT (20). Third, the control group contained
women who may have had a UTI more than 1 month
previously, i.e., not so recently as to have been iden- REFERENCES
tified as a subject in the study. Other women in the
control group may have had UTIs diagnosed outside 1. Fihn SD, Latham RH, Roberts P, et al. Association between
diaphragm use and urinary tract infection. JAMA 1985;254:
the GHC system. To the extent that this occurred, it 240-5.
would also have tended to reduce the magnitude of any 2. Foxman B, Frerichs RR. Epidemiology of urinary tract infec-
association between spermicide use and UTI. Fourth, tion. I. Diaphragm use and sexual intercourse. Am J Public
Health 1985;75:1308-13.
the study population was insured and mainly Cauca- 3. Peddie BA, Bishop VA, Blake EE, et al. Association between
sian. Our results may not generalize to other groups of diaphragm use and asymptomatic bacteriuria. Aust N Z J
women. Obstet Gynecol 1986;26:225-7.
4. Remis RS, Gurwith MJ, Gurwith D, et al. Risk factors for
Given the widespread and highly appropriate efforts urinary tract infection. Am J Epidemiol 1987; 126:685-94.
to enhance the use of condoms, the significance of our 5. Vessey MP, Metcalfe MA, McPherson K, et al. Urinary tract
Downloaded from http://aje.oxfordjournals.org/ by guest on July 14, 2015
findings should be placed in proper perspective. From infection in relation to diaphragm use and obesity. Int J
a clinical standpoint, health care providers should ask Epidemiol 1987;16:441-4.
6. Strom BL, Collins M, West SL, et al. Sexual activity, contra-
women with UTI about the use of spermicide-coated ceptive use, and other risk factors for symptomatic and asymp-
condoms or other routes of exposure to spermicidal tomatic bacteriuria. A case-control study. Ann Intern Med
agents. Women who have recurrent infections should 1987;107:816-23.
be advised about the role of spermicides so that they 7. Foxman B, Chi JW. Health behavior and urinary tract infec-
tion in college-aged women. J Clin Epidemiol 1990;43:
may consider using condoms without spermicidal 329-37.
coating, another form of contraception, and/or protec- 8. Fihn SD, Johnson C, Pinkstaff C, et al. Diaphragm use and
tion from sexually transmitted diseases. The risk of urinary tract infections: analysis of urodynamic and microbi-
ological factors. J Urol 1986;136:853-6.
UTT is but one factor among many that must be con- 9. Percival-Smith R, Bartlett KH, Chow AW. Vaginal coloniza-
sidered in the decision to use spermicides. For most tion of Escherichia coli and its relation to contraceptive meth-
individuals, other factors, such as prevention of human ods. Contraception 1983,27:497-504.
immunodeficiency virus infection and unwanted preg- 10. Peddie BA, Bishop V, Bailey RR, et al. Relationship between
contraceptive method and vaginal flora. Aust N Z J Obstet
nancy, should weigh more heavily. Gynaecol 1984;24:217-18.
It is possible, however, that other active spermicidal 11. Thumer J, Poitschek C, Kopp C. Der Einfluss von Spermiz-
agents might not exert the same deleterious effects on iden auf die physiologische und pathologene Genitalflora. (In
German). Wien Med Wochenschr 1983;133:265-8.
the vaginal flora as N-9, an anionic surfactant that 12. Stamey TA. The role of introital enterobacteria in recurrent
disrupts cell membranes. Research is warranted to find urinary infections. J Urol 1973;109:467-72.
compounds that are less toxic to lactobacilli and 13. Hooton TM, Hillier S, Johnson C, et al. Escherichia coli
demonstrate a greater inhibitory effect upon coliform bacteriuria and contraceptive method. JAMA 1991;265:64-9.
14. Hooton TM, Fennell CL, Clark AM, et al. Nonoxynol-9:
organisms but retain activity against Neisseria gonor- differential antibacterial activity and enhancement of bacterial
rhoeae, Herpes simplex virus, and human immunode- adherence to vaginal epithelial cells. J Infect Dis 1991;164:
ficiency virus. Even if such compounds are less effec- 1216-19.
tive spermicides, they might be desirable to many men 15. Stapleton A, Moseley S, Stamm WE. Urovirulence determi-
nants in Escherichia coli isolates causing first-episode and
and women who use spermicide-coated condoms recurrent cystitis in women. J Infect Dis 1991;163:773-9.
solely for protection against these sexually transmitted 16. Foxman B, Geiger AM, Palin K, et al. First-time urinary tract
organisms. infection and sexual behavior. Epidemiology 1995;6:162-8.
17. Coughlin SS. Recall bias in epidemiologic studies. J Clin
Epidemiol 199O;43:87-91.
18. Hatcher RA, Stewart F, Trussell J, et al. Contraceptive tech-
nology, 1990-1992. 15th revised ed. New York, NY: Irving-
ACKNOWLEDGMENTS ton Publishers, Inc., 1990.
Supported by grants RO1 DK431341-02 and RO1 19. Rothman KJ. Modern epidemiology. Boston, MA: Little,
Brown and Co., 1986.
DK431341-03 from the Epidemiology Program of the Kid- 20. Stamm WE, Counts GW, Running KR, et al. Diagnosis of
ney Branch of National Institute of Diabetes, Digestive, and coliform infection in acutely dysuric women. N Engl J Med
Kidney Diseases. 1982;307:463-8.
Am J Epidemiol Vol. 144, No. 5, 1996You can also read