An Analysis of the United States and United Kingdom Smallpox Epidemics (1901-5) - The Special Relationship that Tested Public Health Strategies ...
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Med. Hist. (2020), vol. 64(1), pp. 1–31. c The Author 2019. Published by Cambridge University Press 2019 This
is an Open Access article, distributed under the terms of the Creative Commons Attribution licence
(http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in
any medium, provided the original work is properly cited.
doi:10.1017/mdh.2019.74
An Analysis of the United States and United Kingdom
Smallpox Epidemics (1901–5) – The Special
Relationship that Tested Public Health Strategies for
Disease Control
BERNARD BRABIN 1,2,3 *
1
Clinical Division, Liverpool School of Tropical Medicine, Pembroke Place,
Liverpool, L3 5QA, UK
2
Institute of Infection and Global Health, University of Liverpool, UK
3
Global Child Health Group, Academic Medical Centre, University of Amsterdam,
The Netherlands
Abstract: At the end of the nineteenth century, the northern port of
Liverpool had become the second largest in the United Kingdom. Fast
transatlantic steamers to Boston and other American ports exploited
this route, increasing the risk of maritime disease epidemics. The
1901–3 epidemic in Liverpool was the last serious smallpox outbreak in
Liverpool and was probably seeded from these maritime contacts, which
introduced a milder form of the disease that was more difficult to trace
because of its long incubation period and occurrence of undiagnosed
cases. The characteristics of these epidemics in Boston and Liverpool
are described and compared with outbreaks in New York, Glasgow and
London between 1900 and 1903. Public health control strategies, notably
medical inspection, quarantine and vaccination, differed between the
two countries and in both settings were inconsistently applied, often for
commercial reasons or due to public unpopularity. As a result, smaller
smallpox epidemics spread out from Liverpool until 1905. This paper
analyses factors that contributed to this last serious epidemic using the
historical epidemiological data available at that time. Though imperfect,
these early public health strategies paved the way for better prevention
of imported maritime diseases.
Keywords: Smallpox, Maritime, Epidemic, Public health, Boston,
Liverpool
* Email address for correspondence: b.j.brabin@liverpool.ac.uk
The author wishes to acknowledge Dr Loretta Brabin and the three anonymous reviewers for critical appraisal
of the manuscript; Mr David McGuirk for assistance with medical illustration; the University of Liverpool Inter-
Library Loan Team; and staff at the Wirral Archives, Liverpool and Birkenhead Central Reference Libraries, and
Wellcome Trust Reference Library, London.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.742 Bernard Brabin
Introduction
A constellation of factors contributed to the pattern of smallpox outbreaks in the United
States and United Kingdom at the onset of the twentieth century. This dreadful disease had
occurred in sequential epidemics throughout the nineteenth century in British cities,1 and
was largely imported from Europe.2 In contrast in the United States, with the exception
of mild smallpox in the southern states and a few severe cases in New York City, the
disease had, by 1897, entirely disappeared from the country.3 This changed in late 1896,
following an outbreak of a very mild type of smallpox which originated in the southern
states and spread over four years to northeastern cities and ports. Historical epidemiology
suggests importation of smallpox from these ports to the United Kingdom, and particularly
to Liverpool from Boston in 1901. The barrier of the Atlantic Ocean was now bridged by
fast transatlantic steamers, shortening crossing times to fewer than six days,4 heightening
commercial shipping interests while allowing rapid dissemination from infected sailors.
The Liverpool Dock System between 1890 and 1906 was radically reconstructed, allowing
intake of a greater number of larger ships from America.5 Liverpool expanded to become
the second largest port in the United Kingdom at the turn of the century.
This paper describes the factors that contributed to the pattern of national smallpox
outbreaks in the United States and United Kingdom, and specifically in the cities of New
York, Boston and Liverpool, between 1901 and 1903. Reconstructing these historical
epidemics using imperfect sources is challenging, and methodological limitations are
considered. The primary aim is to describe public health approaches to control smallpox
during epidemics in major transit ports for Atlantic shipping, and factors which influenced
these efforts. Experience with different responses helped develop a more evidence-based
approach to disease control and to anticipate the general public’s response to such
measures. A knowledge base for disease control was growing, given experience with other
maritime imported epidemic diseases, such as cholera and plague, but smallpox differed
due to the availability of an effective preventive vaccine, the efficacy of which had not
been fully assessed. In analysing these data, a secondary aim is to examine the evidence
that smallpox cases occurring in Liverpool in 1901 and 1902 may have originated from
American imported cases. Peak smallpox incidence in the United States spanned the period
1901 and 1902 and a high infection risk was channelled via ships travelling from Boston
to Liverpool, where the outbreak peaked in April 1903. Outbreaks across northern and
central England were temporally related to the Liverpool epidemic.
The response to the epidemics was influenced by new epidemiological approaches
and public health practices in both countries, although public health recommendations
differed. In the United States, national and state vaccination strategies varied, as did
exemption regulations for children and adults. In both countries, local factors influenced
commercial interests, variable clinical disease patterns, delayed diagnosis and quarantine
practices. An improved understanding of smallpox disease epidemiology slowly emerged
1 Charles Creighton, A History of Epidemics in Britain, Volume Two 1666–1893 First edition 1894 (London:
Frank Kass and Co. Ltd., 1965), 582–601 and 604–19.
2 Donald R. Hopkins, Princes and Peasants, Smallpox in History (Chicago, IL: University of Chicago Press,
1983), 87–96.
3 Charles Value Chapin, ‘Variation in Type of Infectious Disease as Shown by the History of Smallpox in the
United States 1895–1912’, Journal of Infectious Diseases, 13 (1913), 171–96.
4 P.J. Hugill, World Trade since 1431 (Baltimore, MD: Johns Hopkins University Press, 1993), 128.
5 William Farrer and J. Brownbill (eds), A History of the County of Lancaster, Volume 4 (London, 1911), 41–3.
British History Online http://www.british-history.ac.uk/vch/lancs.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 3
and contributed to eventual control and elimination through broadened international
efforts.
Methodological Approaches to Reconstructing Historical Epidemiological
Evidence
Extracting and interpreting late nineteenth-century information from historical medical
records on smallpox in order to quantify risk factors, a standard method in modern disease
epidemiology, is subject to several pitfalls. Instead of meticulous tracing and recording of
known cases and their contacts, the basic assumption at that time attributed the social and
domestic habits of the poor to be the principal factors spreading smallpox.6 Emphasis on
environmental and aggregate models of health and disease suggested that microorganisms
causing a specific disease were subordinate to the person’s total environment.7 It is true
that environmental conditions are important, but by the late nineteenth century it was also
realised that epidemics were caused by a specific agent. Although the organism responsible
for smallpox had not been isolated, it caused a recognised disease, which evoked
introduction of tighter measures to prevent its importation. This included inspecting ships,
monitoring smallpox outbreaks at home and abroad, and some level of contact tracing.8
Europe-wide pandemics from 1870 to 1875 had led to improved vaccination strategies,
with legal provisions for enforcement. These developments, the basis of modern preventive
epidemiology, occurred despite inadequate understanding of the causal agent, its modes of
transmission, or the relative impact of behavioural changes and social determinants.9
Despite such progress, the present reconstruction of historical outbreaks and
examination of their risk factors is affected by several criteria which are difficult to
quantify. These included: variable definitions of reported events; misdiagnoses; lack of
detailed household transmission data; spatial heterogeneities; inadequate information on
vaccine effectiveness – partly because of lack of reliable estimation methods; difficulties
in early recognition of smallpox cases and confusion with chicken pox or measles;
notification delayed until the afflicted person had been suffering for many days and the
absence of explicit statistical analyses.10,11 Since the length of the incubation period
can only be known for individuals exposed early, late reporting compromised quarantine
regulations which specified a period of fourteen to sixteen days. In practice, it was based
on clinical experience and limited epidemiological data. Similarly, vaccine coverage of
the general population, or subgroups, was critical in order to reach a target capable of
interrupting an epidemic. In the modern era, estimates of critical vaccine coverage are
6 Anne Hardy, The Epidemic Streets. Infectious Disease and the Rise of Preventive Medicine 1856–1900 (Oxford:
Clarendon Press, 1993), 134 and 145.
7 Charles E. Rosenberg, Explaining Epidemics and Other Studies in the History of Medicine (Cambridge:
Cambridge University Press, 1992), 299–301.
8 Alexander Mercer, Infections, Chronic Disease, and the Epidemiological Transition: A New Perspective
(Rochester, NY: University of Rochester Press, 2014), 69.
9 S. Del Valle, H. Hethcote, J.M. Hyman and C. Castillo-Chavez, ‘Effects of Behavioural Changes in a Smallpox
Attack Model’, Mathematical Biosciences, 195, 2 (2005), 228–51.
10 Hiroshi Nishiura, Stefan O. Brockmann and Martin Eichner, ‘Extracting Key Information from Historical Data
to Quantify the Transmission Dynamics of Smallpox’, Theoretical Biology and Medical Modelling, 5 (2008), 20
doi:10.1186/1742-4682-5-20.
11 Karen Wallach, The Antivaccine Heresy: Jacobson v. Massachusetts and the Troubled History of Compulsory
Vaccination in the United States (Rochester Studies in Medical History), (Rochester, NY: University of Rochester
Press/Boydell and Brewer, 2015), 70–73, 253. Provides an extensive list of references covering the period 1900
to 1902 on difficulties of smallpox diagnosis in the United States.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.744 Bernard Brabin
obtained by estimating the ’reproduction number’, which is based on the average number
of secondary cases which arise from a single index case in a susceptible population in
the absence of interventions. During the early twentieth century, lack of reliable statistical
methods precluded measurement of vaccine effectiveness and, as a consequence, use of
smallpox vaccine remained controversial. In this paper, vaccine efficacy is calculated from
the data available, both in the United States and the United Kingdom. In 1903, Boston
Health Department physician Dr Frank Morse pointed out that accurate smallpox records
had been kept only since 1888, and were reported in the Annual Reports of the City Health
Department Surgeon, as well as the Annual Reports of the Surgeon General of the Public
Health, and Marine-Hospital Service of the United States. Nevertheless, this information
provided no data on how many people were vaccinated or re-vaccinated out of the total
population.12 In the United Kingdom, case numbers and locations were listed in the
Annual Reports of City Medical Officers of Health, and the Metropolitan Asylums Board,
and these provided crude estimates of vaccinated and allegedly vaccinated individuals,
although criteria for identifying vaccine scars were unclear. Part of the analysis in this
paper uses information based on these reports for the years 1901 to 1905. Monthly case
notifications are available in both the United States and United Kingdom, but seasonal
analysis of case fatality is limited, as available reports provide mostly annual data on
deaths. The availability of these data also enables evaluation of the hypothesis that the
Liverpool outbreaks originated in the United States, where disease control measures
differed and may have been less efficient.
Maritime Relationships between Britain and the United States
Early Twentieth-Century Maritime Quarantine Regulations at British and United States
Seaports
In the late nineteenth century, quarantine stations and regulations for the sanitary
inspection of ships were present at many British seaports, and general sanitary
arrangements were satisfactory in two-thirds of the sixty port sanitary districts.13 Similar
arrangements were present on the Atlantic seaboard of the United States.14 Several
diseases were cause for concern, including cholera, plague, yellow fever and smallpox.15
Sanitary inspection of all vessels entering British or United States ports was the main
strategy available. The UK Public Health (Shipping) Act of 1885 extended the ordinary
powers of local authorities granted in the 1872 Public Health Act to the Port Sanitary
Authorities with respect to infectious disease.16 These initiatives allowed efficient
intervention when vessels with infected crew or passengers entered ports.17 To this end,
smallpox figures for countries from which other ships originated were included in reports
12 Ibid., 16.
13 Anne Hardy, ‘Smallpox in London: Factors in the Decline of the Disease in the Nineteenth Century’, Medical
History, 27 (1983), 128.
14 Howard Markel, ‘A Gate to the City: The Baltimore Quarantine Station, 1918–28’, Public Health Reports,
110, 2 (1995), 218–9.
15 D.S. Barnes, ‘Cargo,”Infection,” and the Logic of Quarantine in the Nineteenth Century’, Bulletin of the
History of Medicine, 88 (2014), 75–101.
16 Public Health (Shipping) Act (1885), 48 & 49, and Public Health Act (1872), 75 & 76 Vict. c. 79, sec. 3, 20.
17 J.C. Burne, ‘The Long Reach Hospital Ships and Miss Willis’, Proceedings of the Royal Society of Medicine,
66 (1973), 1017–21.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 5
in both countries,18,19 and could be used to enhance surveillance.
There was some collaboration between the two countries. The United States Assistant
Surgeon, Dr Carroll Fox (b.1874), stayed in the Liverpool United States Consulate for
three months in 1902 to review infection control policy and practice and the numbers
of smallpox and typhus cases.20 He reported on six Liverpool municipal hospitals as
well as on containment, refuse disposal and disinfection procedures, noting that steam
disinfectors used in Liverpool were newer than those used by the Public Health Service at
the quarantine station in Port Townsend, Washington. This exchange signalled some of the
first international efforts to harmonise infection control practice across major sea routes for
maritime transport. Yet, in September 1902, as Dr Fox completed his mission, eleven ships
with infected seamen from Boston had already arrived in Liverpool, and Dr Fox failed to
mention the Boston epidemic in his report.
In the last decade of the nineteenth century, the twin systems of medical inspection
and quarantine were in use, but with greater emphasis on medical inspection and case
isolation. The risk posed by foreigners had become more evident to the general public
in the United States as migration sensitised opinions, and foreigners became a focus for
quarantine policies.21, 22 In the United Kingdom, the Merchant Shipping Act of 1894
required medical inspection of all outward bound steerage passengers and crew, when
services of a medical practitioner could be obtained, on board ship or preferably before
embarkation.23 In the Port of London, Gravesend, the Medical Officer for the Board of
Trade commonly examined all persons as they proceeded along the gangway and refused
them permission to proceed, if considered ill.24 This screening had low sensitivity, but
should have identified obviously sick travellers with facial rashes, which might be a sign of
active infection. As an alternative to inspection, the argument for quarantine of ships was
contentious. A Lancet editorial commented in 1880 that it only survived because it was
plausible, seductive and fitted the unreasonable demands of certain Continental powers,
and that ’it was derogatory to England that she should submit to these hideously farcical
detrimental proceedings’.25 Quarantine avoided the trouble of disinfecting and removing
the sick, but was costly for trading sea ports. Moreover, unless cholera, plague or yellow
fever was existent on board a vessel, there was no legal authority for detaining her on
sanitary grounds. Some had advocated the inclusion of smallpox in the cholera, plague
and yellow fever order, but a smallpox reservoir in the United Kingdom was assumed so
its inclusion was considered inadvisable, as it would deter international trade.
18 Annual Report of the Surgeon General of the Public Health and Marine-Hospital Service of the United States,
Fiscal Year 1902 (Washington, DC: Government Printing Office, 1903), 303–3.
19 Annual Report of the Surgeon General of the Public Health and Marine-Hospital Service of the United States,
Fiscal Year 1904 (Washington, DC: Government Printing Office, 1905), 100.
20 Annual Report of the Surgeon General of the Public Health and Marine-Hospital Service of the United States,
Fiscal Year 1903 (Washington, DC: Government Printing Office, 1904), 192–3. He later won recognition for the
identification of a quirk in the flea population of San Francisco, California, and helped prevent a wider outbreak
of plague which had been infecting the city population since 1900. Public Health Reports, 25 September 1908,
quoted in David K. Randall, Black Death at the Golden Gate: The race to save America from the bubonic plague
(New York: W.W. Norton and Company, 2019), 210–11.
21 Barnes, op. cit. (note 15).
22 Alan M. Kraut, Silent Travelers: Germs, Genes, and the ’Immigrant Menace’ (Baltimore, MA: Johns Hopkins
University Press, 1995), 50–77.
23 Port of London Sanitary Committee. Annual Report of the Medical Officer of Health to 31 December 1902.
May 1903, 23–5.
24 Ibid., Appendix H, 77–91.
25 The Lancet, editorial, 1 (1880), 687–9.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.746 Bernard Brabin
Quarantine Stations
In Britain, quarantine stations, including some more isolated offshore establishments,
had existed in the early nineteenth century. This remained the only effective measure
until later in the century when contact tracing and surveillance were introduced. Port
Sanitary Authorities established hospital ships in a number of locations around Britain to
isolate suspected smallpox cases. In 1884, the Metropolitan Asylums Board moored three
converted ships in the Thames to serve as a floating hospital,26 primarily for indigenous
cases arising during the 1884–5 London smallpox epidemic.27 By 1899, the Infectious
Diseases Notification Act required compulsory notification of infections, by which time
smallpox was the focus of attention.28 In Liverpool in 1874, the Local Government Board,
under the Public Health Act, permanently constituted the Liverpool Council with powers
to inspect vessels on arrival and to appoint a quarantine station in the River Mersey where
vessels could anchor. A quarantine station already existed at Hoyle Lake, an offshore area
enclosed by sandbanks on the outer Mersey Estuary, which provided accommodation
for infected patients, particularly cholera cases.29 As the estuary began silting up and
Liverpool port expanded, a land-based Port Sanitary isolation hospital was built in 1875 at
New Ferry, isolated from the public, and with ship access via a long wooden jetty.30
Procedures were in place for ship fumigation, cleaning and painting of vessels,
disinfection of clothing, and vaccination of passengers and seamen, although often seamen
refused vaccination.31,32 This task was immense, given the number of ships passing
through the Port of Liverpool. More than 1200 cases of tropical diseases were admitted
to the Port Sanitary Hospital in the period 1875–1963, including cholera, leprosy and
smallpox. Some infectious disease patients were still treated as ordinary patients in
other Liverpool hospitals, including smallpox cases, which were later transferred to New
Ferry.33 As early as 1891, New Ferry was declared unnecessary. Instead, long-haul ships
proceeded directly to the Pier Head entrance of each Liverpool dock to answer questions
on quarantine, a concession much appreciated by ship owners.34 In 1896, quarantine
was discontinued and officially replaced by medical inspection,35 although in practice
quarantine remained, but at the discretion of the Local Government Board rather than
as a national policy.36 New Ferry simply acted as an isolation hospital for eighty-eight
26 Burne, op. cit. (note 17).
27 London Metropolitan Asylums Board Annual Report 1900 (London: M. Corquadale and Co. Ltd., 1901).
28 Infectious Diseases Notification Act (1899), 62 & 63 Vict. c. 8.
29 Thomas Herbert Bickerton, Medical History of Liverpool from the Earliest Days to the Year 1920 (London:
John Murray, 1936), 188.
30 Port Sanitary Hospital, New Ferry, City of Liverpool Smallpox Register, Wirral Archives, Cheshire Lines
Building Centre, Birkenhead, Wirral.
31 Hardy, op. cit. (note 13), 122–3, 129.
32 William Hanna, Report on Marine Hygiene: Being Suggestions for Improvements in the Sanitary
Arrangements and Appliances on Shipboard. Liverpool Port Sanitary Authority (Liverpool: C. Tinling and Co.
Ltd., 1917).
33 Liverpool and Emigration in the Nineteenth and Twentieth Centuries. National Museums Liverpool, Maritime
Archives and Library, Information Sheet 64.
34 John Booker, Maritime Quarantine. The British Expansion, 1650–1900 (Hampshire, UK: Ashgate Publishing
Ltd, 2007), 547.
35 The Public Health Act 1896 (Statute 59 and 60, c19) made provisions with respect to epidemic, endemic
and infectious diseases and repealed the 1825 Quarantine Act (Statute 6 Geo iv, c78), and sections in other acts
in which quarantine was mentioned. The Act united for the first time the sanitary arrangements of the United
Kingdom.
36 Booker, op. cit. (note 34), 549–50.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 7
Figure 1: Liverpool Port Sanitary Hospital Commemorative plaque.
years and was officially razed to the ground in 1963. A commemorative plaque records
its historic role and location and is the last physical reminder of a Port Sanitary hospital
in the United Kingdom (Figure 1). Even today, quarantine is exerted only in exceptional
circumstances.
In the United States, maritime quarantine was initially a state service but was transferred
to a national Public Health Service between the 1880s and the 1920s. The Marine Hospital,
dedicated to the care of ill and disabled seamen in the United States Merchant Marines, the
US Coast Guard and other federal beneficiaries, eventually evolved into the Public Health
Service Commissioned Corps.37 Quarantine stations were established,38 and a prescribed
protocol followed, based on the vessel’s sanitary history and presence of infected or
deceased crew or passengers. Disease detection led to active disinfection and fumigation of
ships and isolation of passengers. When a case of smallpox was diagnosed on board, crew
and passengers were expected to spend fourteen days in quarantine, although breaches
of recommended policies were often made, especially for travellers in first and second
class.39
Factors Leading up to the Boston 1901–2 Smallpox Epidemic in the United
States
Smallpox, when diagnosed, was reported and case fatalities were recorded across the
country. Dr Charles Value Chapin (1856–1941), an American pioneer in public health
research and practice, and Health Superintendent (1884–1932) for Providence, Rhode
Island, compiled a detailed outline of smallpox in the United States between 1895 and
1912.40 By 1897, with the exception of mild smallpox in the South and a few severe cases
in New York City, the disease had disappeared from the country. During 1896, cases of
mild smallpox in Florida began to spread and within a period of about four years cases
37 United States Public Health and Marine-Hospital Service Annual Report, 1905, 221.
38 Markel, op. cit. (note 14).
39 Michael Willrich, Pox. An American History (New York: The Penguin Press, 2011), 219.
40 Chapin, op. cit. (note 3), 186.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.748 Bernard Brabin
were detected all over the country.41 The rate of dispersion was exponential because the
infection was mild, which meant that patients remained active, and contagious, in their
communities and cases were under-reported.42 By 1900 this wave of infection had reached
northeastern cities, and by 1901 had carried smallpox to every state and territory in the
Union. There had been an epidemic in New York City in late 1899, preceding that in
Boston in 1901.43,44 The main culprit was the milder strain (Variola minor), with had a
death rate of 2 to 6% among unvaccinated individuals, which was considerably lower than
with the Variola Major strain.45 Variola major nonetheless remained present in several
American cities, particularly in the northeast.
Disease notification was incomplete in some cities and rural areas, and some states
omitted returns.46 Incidence for individual states returning notifications can be estimated
using 1900 National Population Census data and the 1901 Annual Report of state smallpox
notifications of the Surgeon General of the Public Health and Marine-Hospital Service. 47,
48
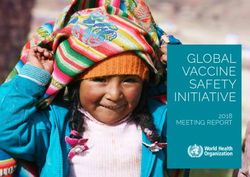
Figure 2 shows these estimates by state between 28 June 1901 and 27 July 1902 per
100 000 population. By 1901, as the epidemic spread to northern states, incidence rapidly
declined in southern states, ranging from less than one per 105 population in Texas, to
more than 300 cases per 105 population in North Dakota, Minnesota and Wisconsin.
Annual smallpox notifications peaked nationally in 1901 at 56 857 cases (Figure 2). In
Massachusetts, where the 1901 Boston epidemic occurred, annual incidence for that year
was sixty per 105 population. In New York City, between 1901 and 1902, 3480 smallpox
cases were reported, with 720 deaths (incidence approximately 100 cases per 100 000
population).49
The Boston epidemic commenced in May 1901 in a large factory.50 Cases were initially
mild but by May 1901 severe cases began to appear. Their source was not known. The
Health Department thought a letter received by a family from infected relatives living
through the New York epidemic was the cause.51 In the outbreak, twelve cases within
forty-eight hours were admitted to hospital, and despite control measures, cases increased
to thirty in September, forty-nine in October, 195 in November, and 201 in December
1901.52 By the end of October 1902, new cases of smallpox had appeared in nearly
every section of the city with the epidemic continuing into 1903. In total, there were
1596 cases (period incidence 284 per 100 000 population) with 270 deaths (17%).53
41 Hopkins, op. cit. (note 2), 288.
42 Gareth Williams, Angel of Death. The Story of Smallpox (Hampshire, UK: Palgrave Macmillan, 2010), 331–2.
43 Chapin, op. cit. (note 3), 186.
44 Willrich, op. cit. (note 39), 41–74, 167.
45 Thirty-First Annual Report of the Health Department of the City of Boston for the Year 1902 (Boston: City of
Boston Printing Department, 1903), 36.
46 Ibid., 172.
47 United States National Census 1900. 12th Census Population. United States Federal Census Records,
www.Censusrecords.com.
48 Annual Report of the Surgeon General of the Public Health and Marine-Hospital Service of the United States,
Fiscal Year 1901 (Washington DC: Government Printing Office, 1902), 319–44, 579–82.
49 John Christie McVail, Half a Century of Smallpox and Vaccination (Milroy Lectures), (Edinburgh: Edinburgh,
E. & S. Livingstone, 1919), 10.
50 Thirtieth Annual Report of the Health Department of the City of Boston for the Year 1901 (Boston: City of
Boston Printing Department, 1902), 43.
51 Chapin, op. cit. (note 3), 186.
52 Thirtieth Boston Annual Health Department Report, op. cit. (note 50), 44.
53 Michael Albert, Kristen Ostheimer and Joel Breman, ‘The Last Smallpox Epidemic in Boston and the
Vaccination Controversy, 1901–1903’, New England Journal of Medicine, 344, 5 (2001), 375–8.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 9
Figure 2: United States smallpox incidence per 100 000 population per annum, 28 June 1901–27 July 1902.
Sources: National Population Census data of 1900 [note 47]; Annual Report of State Smallpox Notifications of
the Surgeon General of the Public Health and Marine-Hospital Service for 1901 [note 48].
A smaller concurrent smallpox epidemic occurred in the adjoining city of Cambridge,
Boston’s close neighbour across the Charles River.54 The nationally prominent senior
public health officer in Boston, and Health Department Chairman, Dr Samuel Holmes
Durgin (1839–1931), initially played down the epidemic, referring to it as only ’a flurry
of cases’ and a minor storm that would pass.55 Durgin advised that schools should remain
open and insisted that immediate vaccination rather than quarantine was the most effective
control strategy. Many leading physicians in Boston preferred vaccination to sanitation and
quarantine, and were somewhat indifferent to public anxiety over contagion.56 Durgin was
blamed for the continued spread of smallpox, not least because he had allowed the Health
Department physicians who treated smallpox patients to mingle with and expose the public
without taking precautions.57 The cost of quarantine weighed heavily on officials and the
controversy received front-page press coverage.58
The difference in severity of cases between epidemics warrants further examination.
Characteristics of this epidemic can be gleaned from the clinical records of 243 patients
consecutively admitted to the Southampton Street smallpox hospital in Boston.59 Some
hospital cases were caused by the Variola major form of smallpox, but these were not
necessarily representative, as many attacks were mild.60 Smallpox has an incubation period
of approximately seven to seventeen days, clinical onset leading to headache and backache,
fever and malaise during a three-day pre-eruptive period before appearance of a skin rash.
54 Wallach, op. cit. (note 11), chapter three, ’The 1901–2 smallpox epidemic in Boston and Cambridge’, 75–8.
55 Ibid., 59.
56 Ibid., 68–9.
57 Ibid., 152–3.
58 ‘Three Strong Letters against Quarantine, The Board of Health’s Opinion. Dr Brough’s Opinion’, Cambridge
Chronicle, 19 July (1896).
59 Michael R. Albert, Kristen G. Ostheimer, David J. Liewehr, Seth M. Steinberg and Joel G. Breman, ‘Smallpox
Manifestations during the Boston Epidemic of 1901–3’, Annals of Internal Medicine, 137, 12 (2002), 993–1000.
60 Wallach, op. cit. (note 11), 69.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.7410 Bernard Brabin
Hospital cases presented with varying severity, but 47% were the milder form of the
disease, and most occurred in previously vaccinated persons. Full recovery took weeks,
with most deaths occurring as a result of unrecognised cases of smallpox in the city and
suburban districts going about from place to place, with many unvaccinated people being
exposed to infection.61 In the initial febrile phase (two to four days), individuals would
be infective, but infected seafarers, or their contacts, may not have developed symptoms
until nearly three weeks later. Individuals incubating the disease could readily depart on
transatlantic ships and act as disease vectors.62
The Boston epidemic coincided with a smaller smallpox epidemic (after accounting
for the difference in population size) in London, commencing in June 1901 and lasting
until January 1903, with 9484 notified cases.63 There is no evidence that the London
and Boston outbreaks were connected, despite their similar timing of onset. The daily
surveillance returns to the Metropolitan Health Board for the 1901–3 London epidemic
indicated upwards of twenty different centres of infection. The origin of the disease for the
first two patients could not be traced and, so far as was known, no cases arose from contact
with them. Two foci at the end of June identified a Parisian male who infected four people,
including a laundry worker who infected nine other contacts.64 In August, several other
cases, whose contact source could be traced, seemed unconnected. Preceding both these
epidemics was an outbreak in Glasgow, which began in April 1900 and lasted until July
1901 (1786 notified cases), with a recrudescent period between January and May 1902
(469 notified cases).65 The Glasgow epidemic terminated prior to the onset of the Boston
epidemic and the two are unlikely to have been directly related. A small epidemic occurred
in Dublin in 1903 with fewer than 250 cases and fewer than forty deaths,66 which resulted
from indigenous transmission with an index case from Glasgow. Vessels from Boston did
not sail via Dublin (see Figure 4 in next section).
Transatlantic Sailings Transmitting Smallpox from the Eastern United States
to Liverpool
In the nineteenth century, thousands of emigrants from the British Isles left from Liverpool
Port. Packet lines sailed regularly from 1818, and in 1822 smallpox was transmitted
from Liverpool to Baltimore on board the ship Pallas.67 Demand for North American
timber and cotton to meet British industrial expansion led to well-established transatlantic
links. British manufactured products provided a useful return cargo. Steamships started
to replace sail after the 1860s and the average voyage time was reduced to as few as
six days.68 The city of Liverpool was largely dependent upon the sea for its commercial
61 Thirty-first Boston Annual Health Department Report, op. cit. (note 45), 36.
62 Albert, op. cit. (note 59), 375.
63 Metropolitan Asylums Board Annual Report 1901, Sixteenth Report of the Statistical Committee (London:
McCorquadale & Co. Ltd., 1902).
64 Ibid., 108.
65 Archibald Kerr Chalmers, ‘Smallpox, 1900–2’, Corporation of Glasgow Report (West Nile Street, Glasgow:
Robert Anderson, Printer, 1902), 8–10.
66 Detailed Annual Reports of the Registrar-General (Ireland), for 1902 (39th), 1903 (40th), 1904 (41st)
containing numbers and causes of deaths registered in Ireland for that year (Dublin: His Majesty’s Stationery
Office, Cahill and Co., 1903, 1904, 1905).
67 Cyril William Dixon, Smallpox (London: Churchill Press, 1962), 198.
68 ‘The American Mails. Performances Outward and Homeward, Cunarders at the Front’, The Liverpool Post, 11
April (1900).
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 11
prosperity. Several steamship lines at the turn of the century were competing for
transatlantic passengers to Boston from Liverpool, and American cattle ships departing
from Boston traded regularly with the City.69 Schedules of ships arriving in Liverpool
from Boston for different steamship companies resulted in multiple arrivals each week,
and round trip transits took less than a month. In 1902, tonnage entering and leaving the
River Mersey amounted to the colossal total of 29 000 000 tons, with 214 000 emigrants.70
Prior to the 1901–3 epidemic, smallpox was imported on eight known occasions to
Liverpool in 1900, the most important being that of the SS New England, which arrived
with nineteen cases on board. This ship left Boston on 1 February, arriving in Liverpool
on 30 March. On leaving Boston with 525 passengers and 268 crew, including fifty-five
clergymen and many elderly people, it travelled to the Mediterranean.71 On 11 March,
prior to arriving in Constantinople, a male death occurred after presenting with petechial
skin haemorrhages, which were attributed to liver atrophy. The body was buried at sea.
By 21 March, twelve other people were sick, including eight crew, two of whom were
employed in the laundry, and two who had been assigned to seal the dead man’s body
in a casket. By 23 March, other passengers were sick with presumed malarial fever and
biliousness, and passenger deaths were reported following visits to Jaffa and Naples. The
Captain’s log only records smallpox after 22 March, and it is unclear why he sought
smallpox vaccination for himself on the 11 March while docked in Constantinople. The
ship’s doctor had no previous experience of smallpox. At Naples, all remaining 500
passengers were peremptorily disembarked and given tourist tickets, while the vessel left
port and sailed for Liverpool without communicating with the port on the nature of this
disease outbreak. The United States Marine Hospital Fortnightly Gazette reported that a
number of these passengers fell ill with smallpox at Naples and in other places in Italy
and France.72 Three persons subsequently developed the disease in Liverpool on dates
which indicated it was contracted prior to disinfection of the ship, which occurred later at
Liverpool. On 8 July 1900, the SS Ivernia from Boston also landed a single smallpox case
at Queenstown while en route to Liverpool.
Competitive, fast transatlantic passenger and mail steamers were efficient disease
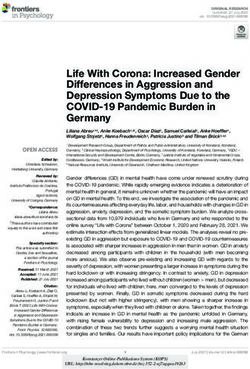
vectors. Figure 3 illustrates three examples of transit involving two ships arriving during
the initial phase of the Liverpool epidemic.73 These ships left Boston during the period of
peak prevalence during the epidemic of 1901–3.
Dates in Figure 3 indicate when notified and not when the illness began. The SS Kansas
arrived in Boston on 15 January 1902 following one smallpox death at sea. The ship was
quarantined but the vessel was allowed to leave for its return trip to Liverpool after only
six days. When it arrived back in Liverpool, nine clinical cases were identified on arrival
and transferred to the Port Sanitary Hospital at New Ferry, one of whom died.74 The crew
had been vaccinated before leaving Boston but some were already incubating the disease.
69 Edward William Hope, Annual Report on the Health of the City of Liverpool during 1901 (Liverpool: C.
Tinling and Co., Printing Contractors, 1902), 39.
70 Thomas Clarke, ‘Introductory Address to the Section on Port Sanitary Administration, Royal Institute of Public
Health Congress, Liverpool, July 1903’, Journal of State Medicine, 11, 8 (1903): 454–61.
71 Port of Liverpool, Annual Report of the Medical Officer of Health to the Port Sanitary Authority for the Year
1900 (Liverpool: C. Tinling and Co., Printing Contractors, 1901), 16–17.
72 Ibid., 17.
73 Edward William Hope, Annual Report on the Health of the City of Liverpool during 1902 (Liverpool: C.
Tinling and Co., Printing Contractors, 1903), 26–51.
74 Port Sanitary Hospital, op. cit. (note 30). These men had different occupations, including baker, engineers,
firemen, carpenter, sailor and boatswain.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.7412 Bernard Brabin
Figure 3: Neighbourhood smallpox transmission linked to imported maritime cases from Boston. Sources: Port
Sanitary Hospital Archives [note 30]; Annual Report on Health of the City of Liverpool during 1902 [note 73].
The Boston Health Department Chairman, Dr Samuel Durgin, received criticism in the
press for allowing the ship to depart after so few days of quarantine.75 At a legislative
hearing on an anti-vaccine bill, Durgin responded as follows to a critical heckler: ’I hold
the public health of Boston in one hand and its commerce in the other’.76 Commercial
interests in Boston were influential factors affecting public health regulations, at least
in this instance. The Health Department deliberately gave the outbreak a low profile to
prevent an unwanted scare. Press releases stated that alarm was needless and claimed
smallpox has never been epidemic in the city.77
The SS Devonian carried infected seamen on separate occasions in early December,
January and February. With the mild type illness, diagnosis was unclear until medical
advice on skin spots was sought.78 A further maritime case was identified on the SS
Campania arriving from New York on 5 April, on a ship holding the fastest transatlantic
crossing time.79 Multiple secondary Liverpool cases arose from these infected seamen,
especially through local lodging houses and contact with workhouse inmates. Seven
different ships were carrying infected passengers, and the SS Kansas imported nineteen
cases from Boston that were admitted to the New Ferry hospital. When the ship sailed
from Liverpool on 4 January 1902, two crew were treated at sea, one of whom died.
Late acquisition of smallpox explained these cases. Upon reaching Boston, as many as
twenty men were put ashore and all cattlemen were taken to the quarantine station and
75 ‘Eight Cases on Board’, The Boston Globe, 7 February (1902), 4.
76 Wallach, op. cit. (note 11), chapter three, ‘The 1901–2 smallpox epidemic in Boston and Cambridge’, 61.
77 ‘Alarm Was Needless. Smallpox Has Never Been Epidemic Here. Less than Two Cases in Every 3000 of the
Population of Boston’, The Boston Globe, 15 December (1901).
78 ‘Smallpox in Liverpool, a Fresh Case Reported Today. Forty-two Cases in the City’, The Liverpool Echo, 17
February (1902), 5.
79 ‘The American Mails, Performances Outward and Homeward. Cunarders to the Front’, The Liverpool Daily
Post, 11 April (1900), 3.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 13
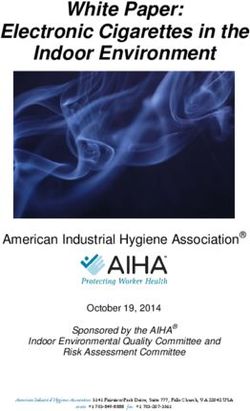
Figure 4: Commercial map showing the transatlantic trade connections of the Port of Liverpool in 1903. Source:
Appendix, City of Liverpool. Handbook Compiled for the Congress of the Royal Institute of Public Health, edited
by E.W. Hope (Liverpool: Lee and Nightingale, Printers, 1903). Map production Spottiswoode and Co., Ltd.,
Liverpool. Commercially developed: red, British Empire; grey, other countries. Detail of transatlantic section
from a world map.
revaccinated.80 Returning to Liverpool after leaving Boston, the SS Kansas put back to
New York and landed several further crew suffering from smallpox. Later arriving at
Liverpool on 6 February, nine convalescents and two contacts were identified and removed
to the Port Sanitary Hospital.81 Most of the crew were revaccinated and some were kept
under close observation.
Figure 4 shows the commercial trade connections of the Port of Liverpool and the
multiple potential routes for inward transmission of smallpox in 1903.82 Vessels from
Liverpool travelling west to Boston discharged first at St Johns, Newfoundland, and
Halifax, Nova Scotia. On the return journey, these vessels often travelled directly to
Liverpool. Between 1901 and 1902, only a single case of smallpox was reported in
Halifax, affecting a seaman on a schooner leaving Gloucester, north of Boston.83 No deaths
from smallpox were reported in St Johns during this period,84 which suggests westward
transmission of smallpox from Liverpool was negligible. The number of maritime cases of
80 Hope, 1903, op. cit. (note 73).
81 ‘The Smallpox, Liverpool, no Fresh Cases, Infected Cattlemen Removed to Hospital’, The Liverpool Daily
Post, 8 February (1902), 6.
82 City of Liverpool, in E.W. Hope (ed.) Handbook Compiled for the Royal Institute of Public Health, Liverpool
Congress, 15–21 July 1903 (Liverpool: Lee and Nightingale, Printers).
83 Alvey A. Adee, ‘A Case of Smallpox on Schooner Thalia at Halifax’, Public Health Reports, 16 (1901), 2176.
84 St Johns, Newfoundland. Register of Deaths St Johns City District, Book 3 (1901–2), 333–9.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.7414 Bernard Brabin
Figure 5: Periodicity of Boston and Liverpool epidemics and dates of transatlantic ship sailings. Sources:
[reference notes, 43, 50, 53, 68, 69].
smallpox landed from vessels in the Port of Liverpool between 1900 and 1904 is shown in
Table 1 in relation to port origin and case fatality. The total number of identified cases
arriving from Boston represents 27% of all maritime cases. The months involved are
shown in detail in Figure 5, to illustrate occurrence in Liverpool and steamship arrivals
from Boston with diagnosed smallpox infected crew or passengers. Another 27% of
importations arrived from New York and Baltimore in 1903 and 1904. Other incoming
vessels from outside the United States were also responsible for importations of cases or
suspected cases of smallpox (Table 1), but the majority of single-country origin was from
the United States.
Maritime and Non-Maritime Spread of Smallpox in the United Kingdom
1901–5
The connexion between seaports and smallpox had been initially observed in England
in the epidemic of 1870–2, when Liverpool and London were the first places to feel the
effects of the continental outbreaks associated with the Franco-Prussian war. In Liverpool,
smallpox had been introduced by Spanish sailors.85 Liverpool experienced almost 2000
deaths in the 1871 epidemic, but these numbers decreased with 685 deaths during the
1876–7 epidemic and 34 deaths in the smaller 1881 epidemic.86
85 Hardy, op. cit. (note 13), 128 and 132.
86 Ibid., 128.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 15
Year Cases from ships Cases from ships arriving Annual Annual
arriving from Boston from other locations case totalb case fatality
n (%)a n (%) n (%) n (%)
1900 1 (3.7)c 26d 156 23 (14.7)
1901 5 (21.7)e 18 37 6 (16.2)
1902 20 (44.4)f 25 560 20 (3.6)
1903 4 (16.6)g 20 1720 141 (8.2)
1904 4 (66.6)h 2 27 2 (7.4)
Total 34 (27.2) 91 2500 192 (7.7)
a Percentage of Boston and East Coast United States transits of all Liverpool maritime cases for that year.
b Annual number of cases for the city of Liverpool.
c Single case landed at Queenstown, Ireland.
d Includes nineteen cases on ship from Boston via the Mediterranean; one case on ship from New York.
e Transported on two different ships.
f Transported on seven different ships.
g Four cases from New York. Sixteen different ships brought cases, or suspected cases, of smallpox.
h Four cases from Baltimore.
Table 1: Number of maritime cases of smallpox landed from vessels in Port of Liverpool 1900–4 in relation to
United States origin and case fatality. Sources: Annual Reports on the Health of the City of Liverpool during
1900–4; Liverpool Smallpox Register, Wirral Archives [reference notes 30, 93].
The 1901 Liverpool outbreak was the last major smallpox epidemic in this city. Its
magnitude was comparable to earlier 1876–8 outbreaks, as shown in Figure 6. Four
Liverpool epidemics had occurred between 1875 and 1896, which exactly corresponded
temporally with the London epidemics, spanning both the same years and having identical
epidemic periods. This suggests indigenous transmission between these cities. In contrast,
the Liverpool epidemic of 1901 commenced twelve months after onset of the London
epidemic and was characterised by milder infections and close association with imported
maritime cases. Yet in London during 1902, of ninety-three smallpox cases treated in their
Port Sanitary Hospital, only one was an imported infection from New York, admitted on
12 April from the SS Minnehaha.87 Other cases were internally transferred to London,
mostly from British Ports – particularly Newcastle, with additional single importations
from Spanish, German and Dutch ports, as well as India and South Africa.88
John Christie McVail (1849–1926), Medical Officer of Health for Stirling and
Dumbarton in Scotland, and a leading advocate of smallpox vaccination in the early
twentieth century, suggested that smallpox was no longer indigenous in the United
Kingdom and insisted that epidemic outbreaks were imported.89 He tabulated provincial
smallpox outbreaks in English and Welsh cities and towns between 1902 and 1905.90
Incidence estimates per capita can be derived from these case numbers using the 1901
United Kingdom National Census. These are listed in Table 2, and their spatial dispersion
mapped in Figure 7. Case fatality estimates are also tabulated for the same locations.
The Liverpool focus is distinct from those in Glasgow, London, Edinburgh, Tynemouth,
Hull and South Wales, which are all ports, but which did not have regular scheduled
87 Port of London Sanitary Committee, Annual Report of the Medical Officer of Health to 31 December 1902,
May 1903, appendix H, 83.
88 Ibid., appendix H, pp. 77–91.
89 McVail, op. cit. (note 49), 8, 26.
90 Ibid., p. 6 (Table II).
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.7416 Bernard Brabin
Location Period in Cases 1901 Census Period incidence Deaths Case fatality
yearsa population per 105 (%)
Lancashire & North-West England
Liverpool 1901–3 2280 684,958 333 160 7.0
Stockport 1902–4 159 78,897 201 15 9.4
Oldham 1902–3 413 137,246 301 32 7.7
Chadderton 1902–5 144 24,000 600 5 3.5
Wigan 1902–3 70 60764 115 1 1.4
Blackburn 1902–3 141 127,626 110 5 3.5
Salford 1902–4 262 220,957 119 12 4.6
Manchester 1902–4 563 543,872 103 33 5.9
Warrington 1903 86 64,242 134 4 4.7
Macclesfield 1903–4 69 37,500 184 5 7.2
Preston 1904–5 172 112,989 152 8 4.7
Bradford 1901 28 279,767 10 0 0.0
St Helens 1902–5 66 84,410 78 3 4.5
ALL 1901–5 4453 2,457,228 181 283 6.3
Yorkshire & Pennines
Ossett Union 1902–3 519 12,903 4022 61 11.8
Heckmondwike 1904 91 9500 958 5 5.5
Dewsbury 1904 552 28,060 1967 57 10.3
Leeds 1902–5 690 428,968 161 35 5.1
Halifax 1903 141 104,936 134 6 4.3
York 1902–4 39 77,914 50 7 17.9
Batley 1904 103 128,712 80 6 5.8
ALL 1902–5 2135 790,993 270 172 8.0
Central England
Leicester 1902–4 731 211,579 345 30 4.1
Derby 1903–4 255 105,912 241 5 2.0
Nottingham 1903–5 479 239,743 200 17 3.5
Sheffield 1902–4 141 380,793 37 5 3.5
Northampton 1902–3 44 87,021 51 9 20.5
Birmingham 1902–5 364 522,204 70 17 4.7
ALL 1902–5 2014 1,547,252 130 83 4.1
North-East England
Tynemouth 1902–5 328 51,366 639 17 5.2
South Shields 1902–5 272 97,263 280 14 5.1
Chester-le-Street 1903–4 106 34,000 312 6 5.7
Newcastle 1903–5 628 215,328 294 28 4.5
Durham 1902 35 419,782 8 1 2.9
Sunderland 1902–3 66 146,077 45 4 6.1
Hull 1903–4 141 240,259 77 8 5.4
ALL 1902–5 1576 1,204,075 131 78 4.9
South Wales and South-West England
Swansea 1902 187 94,537 198 187 17.1
Cardiff 1901–5 96 164,333 58 5 5.2
Portsmouth 1902–5 20 188,133 11 1 5.0
Bristol 1903–5 125 328,945 38 1 3.2
ALL 1902–5 428 479,948 89 39 9.1
Table 2: Continued on next page.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74United States and United Kingdom Smallpox Epidemics (1901–5) 17
Figure 6: Periodicity of London and Liverpool smallpox epidemics between 1875 and 1905. Sources: [reference
notes, 27, 63, 93].
Location Period in Cases 1901 Census Period incidence Deaths Case fatality
yearsa population per 105 (%)
London
Greater London 1901–2 9484 6,226,494 152 (203)b 1540 16.2
Scotland and Ireland
Glasgow 1900–4 3413c 762,000 448 371 10.9
Edinburgh 1900–4 191 303,638 63 16 8.4
Dundee 1903–4 175 154,734 113 12 6.9
Rest of Scotland 1900–4 2844 3,251,731 87 235 8.3
Dublin (hospital) 1903–4 243 448,000 54 33 13.6
a Annual periods may not include all months of the year dependent on month outbreak commenced or resolved.
b Brackets is incidence estimate based on inner city London population alone.
c Includes some cases from beyond city boundaries.
Table 2 (Continued): United Kingdom smallpox period incidence and case fatality 1900–5. Sources: McVail,
Table II, 6 [note 49]; Martin, Table II, 19 [Journal of Hygiene, 34, 1(1934)]; UK Census, 1901 [note 39].
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.7418 Bernard Brabin
Figure 7: United Kingdom spatial smallpox period incidence per 105 population 1900–5. Sources: McVail, Table
II, 6 [note 49]; United Kingdom National Census, 1901 [note 99].
transatlantic links with eastern United States seaports. In Southampton, only two cases
of smallpox were reported on vessels bound for the port in 1902.91 Smallpox outbreak
distribution shows temporal dispersion across northwest and central England between the
years 1902 and 1904. The dispersion pattern implicates Liverpool as the primary focus,
possibly with discrete sequential transmission across the northwest during these years.
In these outbreaks, case fatality was low or very low (Table 2) and in the northwest
averaged 6.3%. This mortality was much lower than in the 1901 London epidemic (21.6%),
suggesting that infection was mostly due to a different milder strain, consistent with
transmission mainly from the Liverpool focus where a mild strain of Variola minor was
dominant. Chapin had considered it highly probable that the mild type of smallpox was
carried to England from Boston in 1902 and during the following years.92 Case fatality
during the epidemic decreased from around 16% in 1901 to 8% in 1903.93 As all cases
were hospitalised, this may have caused a bias towards observing severe or fatal cases.94
91 Southampton 1902 Public Health Report, 26.
92 Chapin, op. cit. (note 3).
93 Annual Reports on the Health of the City of Liverpool during 1900 to 1904 (Liverpool: C. Tinling and Co.,
Printing Contractors, 1901). Estimates compiled from figures available from Annual Health Reports produced by
Dr E.W. Hope, Medical Officer of Health for Liverpool, for the years 1900 to 1904, and published in the years
1901, 1902, 1903, 1904 and 1905.
94 Martin Eichner, ‘Analysis of Historical Data Suggests Long-lasting Protective Effects of Smallpox
Vaccination’, American Journal of Epidemiology, 158 (2003), 717–23.
Downloaded from https://www.cambridge.org/core. IP address: 46.4.80.155, on 21 Dec 2020 at 20:26:58, subject to the Cambridge Core terms of use, available at
https://www.cambridge.org/core/terms. https://doi.org/10.1017/mdh.2019.74You can also read