The Role of Sleep Curtailment on Leptin Levels in Obesity and Diabetes Mellitus
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Review Article
Obes Facts 2021;14:214–221 Received: May 30, 2020
Accepted: December 23, 2020
DOI: 10.1159/000514095 Published online: March 23, 2021
The Role of Sleep Curtailment on Leptin
Levels in Obesity and Diabetes Mellitus
Maryam Mosavat a Mitra Mirsanjari b Diana Arabiat a, c Aisling Smyth a
Lisa Whitehead a
a School
of Nursing and Midwifery, Edith Cowan University, Joondalup, WA, Australia; b Mazandaran University
of Medical Sciences, Emam Khomeini Hospital, Mazandaran, Iran; c Maternal and Child Nursing Department,
The University of Jordan, Amman, Jordan
Keywords Introduction
Short sleep duration · Leptin · Obesity · Diabetes
Sleep is a biological and behavioral process that is fun-
damental for life and optimum health. Sleep is controlled
Abstract by diurnal, homeostatic, and neurohormonal mecha-
Emerging evidence has identified sleep as a significant, but nisms [1]. Existing research acknowledges that sleep is an
modifiable, risk factor for metabolic syndrome, diabetes, and essential modulator of cardiovascular function, glucose
obesity. Leptin, an adipocyte-derived peptide and a regula- regulation, and hormonal release [2]. Sleep duration has
tor of food intake and energy expenditure, has been shown also been shown to have a pivotal function in metabolic
to be associated with a short sleep duration in the patho- hormones and body weight and it has been linked to oth-
physiology of obesity and consequently type 2 diabetes. This er biological mechanisms including inflammation, the
review focuses on the current evidence indicating the effects autonomic nervous system, the coagulation system, en-
of a short sleep duration on the regulation of leptin concen- dothelial function, and metabolic regulation [3, 4]. Sleep
tration in association with obesity and diabetes mellitus. In quality varies in individuals according to factors such as
summary, the evidence suggests that sleep deprivation, by age, gender, occupation, educational level, socioeconom-
affecting leptin regulation, may lead to obesity and conse- ic status, race, family relationships, and pathological con-
quently development of type 2 diabetes through increased ditions including insomnia, depression level, and sleep-
appetite and food intake. However, findings on the role of disordered breathing [5–7]. According to the US Nation-
leptin in diabetes due to sleep deprivation are contradictory, al Sleep Foundation, adequate sleep duration requirements
and further studies with larger sample sizes are needed to vary across lifespans and from person to person, with 7–
confirm previous findings. © 2021 The Author(s) 9 h recommended for adults [8, 9]. In recent decades, the
Published by S. Karger AG, Basel average sleep duration has decreased worldwide, and this
is widely attributed to a modern lifestyle [10]. Based on
National Sleep Foundation criteria, 75% of preadoles-
karger@karger.com © 2021 The Author(s) Maryam Mosavat
www.karger.com/ofa Published by S. Karger AG, Basel School of Nursing and Midwifery, Edith Cowan University
This article is licensed under the Creative Commons Attribution-
270 Joondalup Dr.
NonCommercial-NoDerivatives 4.0 International License (CC BY- Joondalup, WA 6027 (Australia)
NC-ND) (http://www.karger.com/Services/OpenAccessLicense). m.mosavat @ ecu.edu.au
Usage and distribution for commercial purposes as well as any dis-
tribution of modified material requires written permission.cents and 45% of late adolescents experience sleep defi- cardiovascular disease, and downstream targets of leptin
ciency [11]. may have a therapeutic potential role in the management
Insufficient sleep is characterized by either a consider- of diabetes [29, 30]. Furthermore, the adiponectin-leptin
able reduction in sleep time during a certain period due ratio has been found to be significantly correlated with
to 24-h wakefulness or a reduction in sleep time less than the insulin resistance index in diabetes mellitus [31–33].
the optimal level for individual needs. Sleep loss, related Leptin stimulates cytokine activation and immune-cell
to a decreased total sleep time, can be a result of habitual proliferation, which predisposes to inflammatory condi-
behavior or the presence of a pathological condition in- tions [34].
cluding addiction (medications or alcohol), anxiety, de- The evidence suggests a bidirectional relationship be-
pression, idiopathic, somatic and painful diseases, and tween sleep duration and leptin. Leptin has central neural
subjective and psychophysiological insomnia [12]. specific effects beyond modulation of appetite alone [35].
The reports from recent epidemiological studies, me- Leptin concentrations display a circadian pattern, with its
ta-analyses, and systematic reviews have indicated that levels increasing during the first part of the night and then
sleep duration is significantly correlated with several ad- decreasing during the latter part of the night [36]. Fur-
verse health outcomes including diabetes mellitus, car- thermore, leptin has a function in preserving deep sleep
diovascular diseases, coronary heart diseases and stroke, by antagonizing the orexin neuron function in the hypo-
dyslipidemia, hypertension, metabolic disease, obesity, thalamus [37]. The findings of animal studies presented
and mortality [1, 13–20]. Recent evidence proposes that that the orexin (hypocretin) system monitors sleep and
that relationship between a short sleep duration, obesity, wakefulness through interactions with the system that
and diabetes risk may include at least 3 pathways, i.e., regulates energy homeostasis and facilitates adaptive in-
(1) an altered glucose metabolism, (2) up-regulation of tensification of arousal in response to fasting. The orexin
hunger and appetite or dysregulation of appetite/satiety neuron actions are inhibited by leptin, blood glucose, and
hormones, and (3) down-regulation of energy expendi- food intake [37–39]. An animal study in leptin-resistant
ture [21]. (db/db) genetically obese and diabetic mice showed that
Leptin, a metabolic hormone, has a pivotal function in impaired leptin signaling had deleterious impacts on the
balancing appetite and satiety via food intake regulation regulation of sleep duration [40]. This study proposed
and energy homeostasis [22]. Leptin works in synergy that leptin signaling plays an important role in coordina-
with another metabolic hormone, i.e., ghrelin. Whereas tion of sleep-wake states and metabolism. It appears that
leptin suppresses food intake and induces weight loss, sleep-related changes in leptin level promote progression
ghrelin increasing hunger and food intake [22]. Leptin is of metabolic and immune disorders. Leptin’s proinflam-
the product of the ob gene, which has an impact on matory role [24, 41, 42] proposes that increased serum
growth, metabolism, and reproduction [23, 24]. Leptin leptin levels in metabolic syndrome and obesity in a sleep
has several other biological roles in the body [24], includ- deprivation status may be associated with low-grade sys-
ing functions in glucose homeostasis via suppression of temic inflammatory diseases, characterized by increased
insulin production in pancreatic β cells [25]. The regula- proinflammatory cytokine levels including interleukin-6
tion of diurnal blood leptin is controlled by multiple fac- and tumor necrosis factor (TNF)-α. Leptin regulates the
tors such as gender, age, feeding, fasting, sleep, obesity, brain appetite-regulating center with information about
and endocrine disorders [26]. The concentration of se- energy balance [43]. It has been believed that there is an
rum leptin is directly related to fat mass, where increased interaction between leptin and insulin in peripheral tis-
circulating leptin, termed leptin resistance, is related to sues [44, 45]. Leptin inhibits energy storage mechanisms,
obesity [27]. The proposed mechanisms involved in whereas insulin enhances leptin production [46]. Evi-
leptin resistance are comprised of a reduction in the num- dence also indicates that leptin promotes insulin sensitiv-
ber of leptin receptors, impairment of receptor function, ity through enhancement of fatty acid oxidation and de-
a reduction in transport across the blood-brain barrier, clined fat accumulation in non-adipose tissues. Leptin
and a circulating suppressor of leptin function [28]. Since induces fatty acid oxidation in muscle via AMP-activated
a leptin deficit in lipodystrophy is accompanied by dys- protein kinase (AMPK) [47]. Moreover, leptin has a sig-
glycemia and insulin resistance, it is expected that glucose nificant role in increasing the glucose uptake in skeletal
metabolism is affected by leptin resistance [28]. Defects muscle through a β-adrenergic mechanism and the hypo-
or dysfunction in the leptin signaling pathway plays a role thalamic-sympathetic nervous system axis [47].
in the pathophysiology of obesity, diabetes mellitus, and
Sleep Curtailment and Leptin Circulation Obes Facts 2021;14:214–221 215
DOI: 10.1159/000514095As one of the factors affecting leptin level regulation, creased body mass. These researchers suggested that a the effect of sleep has been investigated in several experi- leptin deficiency increases appetite and consequently mental studies. Sleep loss with an effect on appetite hor- may cause obesity. The Child and Adolescent Metabolic mone (leptin) and energy expenditure has been linked to Syndrome cohort studies [55, 56] suggested that a short an increased risk of obesity and diabetes. This review aims sleep duration (
increased hunger [66]. Hayes et al. [65] have examined
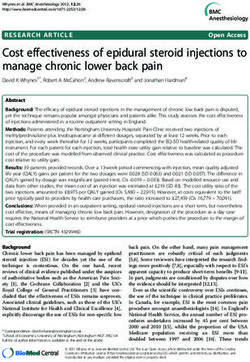
the level of leptin in association with a reduced sleep time Sleep curtailment
among adults. They reported that a 1-h decrease in total
sleep duration was associated with a 10% increase in
leptin levels [65]. A study on salivary cortisol and leptin Sympathetic Proinflammatory
↑ Ghrelin ↑ ↑
activity cytokines
in young healthy women showed that a single night of
restricted sleep (3 h) altered the diurnal pattern of cortisol
rhythms (the level of morning cortisol was reduced, and ↑ TSH
↑ cortisol
afternoon/evening cortisol levels were elevated) and in-
creased morning leptin levels in subjects but it did not
have an effect on hunger and craving scores [67]. Bosy- ↑
↓ Leptin Insulin resistance
Westphal et al. [73] found that consecutive nightly de- →
creases in sleep duration significantly increased body
weight, energy intake, glucose-induced thermogenesis, ↑
Appetite &
Obesity Diabetes
leptin/fat mass, free triiodothyronine, and free thyroxine hunger
[73]. Charles et al. [74] showed that both short (8 h) sleep durations were associated with increased
Fig. 1. Role of sleep restriction on leptin regulation in obesity and
leptin levels related to obesity. diabetes.
However, unaffected leptin levels have been reported
in patients with a sleep deficiency [61]. In a study in men
with and without insomnia, circulating levels of leptin
and ghrelin were measured across the night. Serial mea- sequently diabetes mellitus. It was shown by a systematic
surement of appetite hormones showed that ghrelin lev- and meta-analysis study that both short and long sleep
els were significantly lower in insomnia patients, whereas durations in type 2 diabetes patients is significantly associ-
leptin did not differ between the groups. Furthermore, ated with an increase in hemoglobin A1c (HbA1c) levels,
the findings of this study concluded that dysregulation in suggesting poorer glycemic control compared to that with
energy balance in patients with insomnia results in weight a normal sleep duration, with the relationship being U-
gain in this population [61]. A Circadian Locomotor Out- shaped [84]. In another study both a short sleep duration
put Cycles Kaput (CLOCK) gene study showed that a (>5.5 and 5.5–6.4 h) and a long sleep duration (7.5–8.4 h)
shorter sleep duration increased ghrelin levels with no ef- were associated with an increase in the risk of metabolic
fects on leptin values [60]. This study suggested that sleep syndrome, insulin resistance, and high-sensitivity C-reac-
reduction with alterations in ghrelin levels and changes tive protein in diabetic patients compared to those with
in eating behaviors may affect weight and weight loss. 6.5–7.4 h of sleep [85]. These findings also concluded that
Schmid et al. [62], in a study in healthy normal-weight sleep duration has a U-shaped relationship with metabol-
men, reported that feelings of hunger and ghrelin levels ic syndrome and insulin resistance. A recent meta-analy-
were elevated after 1 night of total sleep deprivation, sis confirmed that short sleep (> 6 compared to 7 h) may
whereas morning serum leptin concentrations was unaf- increase the risk of type 2 diabetes by approximately 30%
fected. A large multiethnic study also found no associa- [86]. It has been proposed that sleep deprivation impairs
tion between sleep duration and leptin levels [75]. insulin sensitivity and pancreatic β-cell function and glu-
cose uptake by target cells, increasing insulin resistance
and leading to type 2 diabetes [87–94]. Recent evidence
Sleep Duration, Leptin, and Diabetes suggests that the metabolic hormones leptin and ghrelin
are involved in the relationship between sleep and dys-
Sleep plays a critical role in glucose regulation, and regulation of insulin and glucose and increase the risk of
sleep duration has been shown to have an inverse effect on diabetes [63, 68, 94–97]. Given the effects of sleep defi-
endocrine function and carbohydrate metabolism [2, 76]. ciency on leptin levels and metabolism, a short sleep dura-
The link between sleep and glucose metabolism has been tion may mediate its effects on incident diabetes through
explored in several studies, where it has been proposed weight gain [98, 99] (Fig. 1).
that both short [13, 77–80] and long sleep durations [81– The reviews on the role of sleep restriction in the met-
83] may increase the risk of developing obesity and con- abolic and endocrine alterations propose that a decreased
Sleep Curtailment and Leptin Circulation Obes Facts 2021;14:214–221 217
DOI: 10.1159/000514095sleep duration impairs glucose tolerance and insulin sen- vestigated the role of a short sleep duration on leptin
sitivity, increases evening concentrations of cortisol and regulation; however, the findings regarding the role of
levels of ghrelin, decreases levels of leptin, and increases leptin in diabetes as a consequence of sleep curtailment
appetite and hunger [100, 101]. are conflicting and more studies with a larger sample size
In contrast, a multiethnic study in a population at high are required to confirm the previous findings.
risk for diabetes showed that a short sleep duration (≤5.5
h) was associated with an increase in leptin levels [75]. A
study in diabetic patients showed that an insufficient Strengths and Limitations
sleep duration increased the level of leptin and insulin re-
sistance compared to those with an appropriate sleep du- We reviewed and discussed the probable mechanism
ration [102]. A laboratory-based sleep study showed that underlying the effect of sleep duration on leptin regula-
sleep restriction (5 nights of 4 h in bed) impaired glucose tion as the potential physiological mechanism underlying
homeostasis and increased fasting and insulin levels [63]. obesity and type 2 diabetes. Potential limitations of this
Sleep restriction was associated with an increase in after- work include the conflation of sleep quality and sleep du-
noon cortisol and leptin levels compatible with an in- ration where these were not always reported separately in
creased insulin resistance [63]. It has been reported that the studies included in this review. Furthermore, this re-
a 1-h reduction in sleep duration was associated with a 7% view was conducted as a narrative review and as such a
elevation in leptin levels [65]. Furthermore, a study in ro- quality appraisal of the included papers was not under-
tating-shift-work women reported an inverse association taken. Further work is required to compare the findings
between leptin levels and the risk of type 2 diabetes. How- of both sleep quality and duration on leptin circulation
ever, there was no association between sleep duration, related to obesity and diabetes.
leptin levels, and diabetes [103].
Considering the role of leptin in regulation of energy
consumption, a decrease in the production of leptin due Conflict of Interest Statement
to a lack of sleep may explain the contribution of adjust-
ment of this hormone to obesity, decreased insulin sensi- The authors declare that there is no conflict of interest regard-
ing the publication of this article.
tivity, and increased insulin resistance. It is noteworthy
that elevation of serum leptin levels results in decreased
leptin transport across the blood-brain barrier [104]. It Funding Sources
has been indicated that when leptin reaches its threshold
the blood-brain barrier limits the leptin transport from There were no funding sources for this work.
peripheral blood to the central nervous system, inhibiting
its activity [105]. This condition may explain the eleva-
tion of leptin levels due to sleep restriction, where the ef- Author Contributions
fectiveness of it is attenuated. In this way, leptin resis-
tance, characterized by a decreased response to leptin due Maryam Mosavat drafted this paper. Mitra Mirsanjari, Diana
Arabiat, Aisling Smyth, and Lisa Whitehead reviewed and revised
to a reduced receptor expression, is another possible this work. All authors read and approved the final version of this
mechanism that explains elevated leptin levels in the article.
blood but decreased leptin effects [28]. Thus, in the case
of elevated plasma leptin levels it does not consistently
reflect increased leptin efficacy and function in glucose
homeostasis [28]. References 1 Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W,
et al. Sleep duration and risk of type 2 diabe-
In summary, recent evidence indicates that an insuf- tes: a meta-analysis of prospective studies. Di-
ficient sleep duration, with an effect on leptin metabo- abetes Care. 2015 Mar;38(3):529–37.
lism, may promote the development of type 2 diabetes 2 Van Cauter E, Spiegel K, Tasali E, Leproult R.
Metabolic consequences of sleep and sleep
through increased hunger/food intake and weight gain. loss. Sleep Med. 2008 Sep;9(1):S23–8.
Furthermore, leptin dysregulation contributes to de- 3 Tobaldini E, Fiorelli EM, Solbiati M, Costan-
creased insulin secretion and sensitivity, increased insu- tino G, Nobili L, Montano N. Short sleep du-
ration and cardiometabolic risk: from patho-
lin resistance and inflammation, and consequently an in- physiology to clinical evidence. Nat Rev Car-
creased risk of diabetes mellitus. Several studies have in- diol. 2019 Apr;16(4):213–24.
218 Obes Facts 2021;14:214–221 Mosavat/Mirsanjari/Arabiat/Smyth/
DOI: 10.1159/000514095 Whitehead4 Taheri S, Lin L, Austin D, Young T, Mignot E. 18 Shen X, Wu Y, Zhang D. Nighttime sleep du- 35 Olson CA, Hamilton NA, Somers VK. Per-
Short sleep duration is associated with re- ration, 24-hour sleep duration and risk of all- centage of REM sleep is associated with over-
duced leptin, elevated ghrelin, and increased cause mortality among adults: a meta-analysis night change in leptin. J Sleep Res. 2016 Aug;
body mass index. PLoS Med. 2004 Dec; of prospective cohort studies. Sci Rep. 2016 25(4):419–25.
1(3):e62. Feb;6(1):21480. 36 Licinio J, Mantzoros C, Negrão AB, Cizza G,
5 Heinzer R, Vat S, Marques-Vidal P, Marti- 19 Wu Y, Zhai L, Zhang D. Sleep duration and Wong ML, Bongiorno PB, et al. Human leptin
Soler H, Andries D, Tobback N, et al. Preva- obesity among adults: a meta-analysis of pro- levels are pulsatile and inversely related to pi-
lence of sleep-disordered breathing in the spective studies. Sleep Med. 2014 Dec;15(12): tuitary-adrenal function. Nat Med. 1997 May;
general population: the HypnoLaus study. 1456–62. 3(5):575–9.
Lancet Respir Med. 2015 Apr;3(4):310–8. 20 Leng Y, Cappuccio FP, Wainwright NW, 37 Hirota T, Morioka T, Yoda K, Toi N, Hayashi
6 Park C, Sim CS, Sung JH, Lee J, Ahn JH, Choe Surtees PG, Luben R, Brayne C, et al. Sleep N, Maruo S, et al. Positive association of plas-
YM, et al. Low Income as a Vulnerable Factor duration and risk of fatal and nonfatal stroke: ma leptin with sleep quality in obese type 2
to the Effect of Noise on Insomnia. Psychiatry a prospective study and meta-analysis. Neu- diabetes patients. J Diabetes Investig. 2018
Investig. 2018 Jun;15(6):602–12. rology. 2015 Mar;84(11):1072–9. Sep;9(5):1100–5.
7 Ruggiero AR, Peach HD, Gaultney JF. Asso- 21 Knutson KL, Spiegel K, Penev P, Van Cauter 38 Yamanaka A, Beuckmann CT, Willie JT, Hara
ciation of sleep attitudes with sleep hygiene, E. The metabolic consequences of sleep depri- J, Tsujino N, Mieda M, et al. Hypothalamic
duration, and quality: a survey exploration of vation. Sleep Med Rev. 2007 Jun; 11(3): 163– orexin neurons regulate arousal according to
the moderating effect of age, gender, race, and 78. energy balance in mice. Neuron. 2003 Jun;
perceived socioeconomic status. Health Psy- 22 Klok MD, Jakobsdottir S, Drent ML. The role 38(5):701–13.
chol Behav Med. 2019 Jan;7(1):19–44. of leptin and ghrelin in the regulation of food 39 Sakurai T. The neural circuit of orexin (hypo-
8 Hirshkowitz M, Whiton K, Albert SM, Alessi intake and body weight in humans: a review. cretin): maintaining sleep and wakefulness.
C, Bruni O, DonCarlos L, et al. National Sleep Obes Rev. 2007 Jan;8(1):21–34. Nat Rev Neurosci. 2007 Mar;8(3):171–81.
Foundation’s updated sleep duration recom- 23 Denver RJ, Bonett RM, Boorse GC. Evolution 40 Laposky AD, Bradley MA, Williams DL, Bass
mendations: final report. Sleep Health. 2015 of leptin structure and function. Neuroendo- J, Turek FW. Sleep-wake regulation is altered
Dec;1(4):233–43. crinology. 2011;94(1):21–38. in leptin-resistant (db/db) genetically obese
9 Hirshkowitz M, Whiton K, Albert SM, Alessi 24 Fantuzzi G, Faggioni R. Leptin in the regula- and diabetic mice. Am J Physiol Regul Integr
C, Bruni O, DonCarlos L, et al. National Sleep tion of immunity, inflammation, and hema- Comp Physiol. 2008 Dec;295(6):R2059–66.
Foundation’s sleep time duration recommen- topoiesis. J Leukoc Biol. 2000 Oct;68(4):437– 41 Jahromi AS, Zareian P, Madani A. Associa-
dations: methodology and results summary. 46. tion of insulin resistance with serum interleu-
Sleep Health. 2015 Mar;1(1):40–3. 25 Wang C, Guan Y, Yang J. Cytokines in the kin-6 and TNF-α levels during normal preg-
10 Van Cauter E, Knutson KL. Sleep and the ep- progression of pancreatic β-cell dysfunction. nancy. Biomark Insights. 2011;6:BMI–S6150.
idemic of obesity in children and adults. Eur Int J Endocrinol. 2010;2010:515136. 42 Xu LL, Shi CM, Xu GF, Chen L, Zhu LL, Zhu
J Endocrinol. 2008 Dec;159 Suppl 1:S59–66. 26 Pan W, Kastin AJ. Leptin: a biomarker for L, et al. TNF-α, IL-6, and leptin increase the
11 Miguez MJ, Bueno D, Perez C. Disparities in sleep disorders? Sleep Med Rev. 2014 Jun; expression of miR-378, an adipogenesis-relat-
sleep health among adolescents: the role of 18(3):283–90. ed microRNA in human adipocytes. Cell Bio-
sex, age, and migration. Sleep Disord. 2020 27 Zhou Y, Rui L. Leptin signaling and leptin re- chem Biophys. 2014 Nov;70(2):771–6.
Jan;2020:5316364. sistance. Front Med. 2013 Jun;7(2):207–22. 43 Timper K, Brüning JC. Hypothalamic circuits
12 Medic G, Wille M, Hemels ME. Short- and 28 Gruzdeva O, Borodkina D, Uchasova E, Dyl- regulating appetite and energy homeostasis:
long-term health consequences of sleep dis- eva Y, Barbarash O. Leptin resistance: under- pathways to obesity. Dis Model Mech. 2017
ruption. Nat Sci Sleep. 2017 May;9:151–61. lying mechanisms and diagnosis. Diabetes Jun;10(6):679–89.
13 Itani O, Jike M, Watanabe N, Kaneita Y. Short Metab Syndr Obes. 2019 Jan;12:191–8. 44 Amitani M, Asakawa A, Amitani H, Inui A.
sleep duration and health outcomes: a system- 29 Meek TH, Morton GJ. Leptin, diabetes, and The role of leptin in the control of insulin-
atic review, meta-analysis, and meta-regres- the brain. Indian J Endocrinol Metab. 2012 glucose axis. Front Neurosci. 2013 Apr;7:51.
sion. Sleep Med. 2017 Apr;32:246–56. Dec;16(9 Suppl 3):S534–42. 45 D’souza AM, Neumann UH, Glavas MM,
14 Cappuccio FP, Cooper D, D’Elia L, Strazzullo 30 Meek TH, Morton GJ. The role of leptin in Kieffer TJ. The glucoregulatory actions of
P, Miller MA. Sleep duration predicts cardio- diabetes: metabolic effects. Diabetologia. leptin. Mol Metab. 2017 May;6(9):1052–65.
vascular outcomes: a systematic review and 2016 May;59(5):928–32. 46 Rosenbaum M, Leibel RL. 20 years of leptin:
meta-analysis of prospective studies. Eur 31 Oda N, Imamura S, Fujita T, Uchida Y, In- role of leptin in energy homeostasis in hu-
Heart J. 2011 Jun;32(12):1484–92. agaki K, Kakizawa H, et al. The ratio of leptin mans. J Endocrinol. 2014 Oct;223(1):T83–96.
15 Cappuccio FP, D’Elia L, Strazzullo P, Miller to adiponectin can be used as an index of in- 47 Minokoshi Y, Toda C, Okamoto S. Regulatory
MA. Quantity and quality of sleep and inci- sulin resistance. Metabolism. 2008 Feb;57(2): role of leptin in glucose and lipid metabolism
dence of type 2 diabetes: a systematic review 268–73. in skeletal muscle. Indian J Endocrinol Metab.
and meta-analysis. Diabetes Care. 2010 Feb; 32 Zaletel J, Barlovic DP, Prezelj J. Adiponectin- 2012 Dec;16(9 Suppl 3):S562–8.
33(2):414–20. leptin ratio: a useful estimate of insulin resis- 48 Beccuti G, Pannain S. Sleep and obesity. Curr
16 Wang Y, Mei H, Jiang YR, Sun WQ, Song YJ, tance in patients with Type 2 diabetes. J En- Opin Clin Nutr Metab Care. 2011 Jul; 14(4):
Liu SJ, et al. Relationship between duration of docrinol Invest. 2010 Sep;33(8):514–8. 402–12.
sleep and hypertension in adults: a meta-anal- 33 Mosavat M, Omar SZ, Tan PC, Razif MF, 49 Hakim F, Wang Y, Carreras A, Hirotsu C,
ysis. J Clin Sleep Med. 2015 Sep; 11(9): 1047– Sthaneshwar P. Leptin and soluble leptin re- Zhang J, Peris E, et al. Chronic sleep fragmen-
56. ceptor in association with gestational diabe- tation during the sleep period induces hypo-
17 Chaput JP, McNeil J, Després JP, Bouchard C, tes: a prospective case-control study. Arch thalamic endoplasmic reticulum stress and
Tremblay A. Short sleep duration as a risk fac- Gynecol Obstet. 2018 Mar;297(3):797–803. PTP1b-mediated leptin resistance in male
tor for the development of the metabolic syn- 34 Peelman F, Waelput W, Iserentant H, Lavens mice. Sleep (Basel). 2015 Jan;38(1):31–40.
drome in adults. Prev Med. 2013 Dec; 57(6): D, Eyckerman S, Zabeau L, et al. Leptin: link- 50 Seetho IW, Wilding JP. Screening for obstruc-
872–7. ing adipocyte metabolism with cardiovascu- tive sleep apnoea in obesity and diabetes—po-
lar and autoimmune diseases. Prog Lipid Res. tential for future approaches. Eur J Clin In-
2004 Jul;43(4):283–301. vest. 2013 Jun;43(6):640–55.
Sleep Curtailment and Leptin Circulation Obes Facts 2021;14:214–221 219
DOI: 10.1159/00051409551 van der Lely AJ, Tschöp M, Heiman ML, 64 Simpson NS, Banks S, Dinges DF. Sleep re- 78 Schultes B, Schmid S, Peters A, Born J, Fehm
Ghigo E. Biological, physiological, patho- striction is associated with increased morning HL. Sleep loss and the development of diabe-
physiological, and pharmacological aspects of plasma leptin concentrations, especially in tes: a review of current evidence. Exp Clin En-
ghrelin. Endocr Rev. 2004 Jun;25(3):426–57. women. Biol Res Nurs. 2010 Jul;12(1):47–53. docrinol Diabetes. 2005 Dec;113(10):563–7.
52 Zigman JM, Elmquist JK. Minireview: from 65 Hayes AL, Xu F, Babineau D, Patel SR. Sleep 79 Lou P, Zhang P, Zhang L, Chen P, Chang G,
anorexia to obesity—the yin and yang of body duration and circulating adipokine levels. Zhang N, et al. Effects of sleep duration and
weight control. Endocrinology. 2003 Sep; Sleep (Basel). 2011 Feb;34(2):147–52. sleep quality on prevalence of type 2 diabetes
144(9):3749–56. 66 Pejovic S, Vgontzas AN, Basta M, Tsaousso- mellitus: A 5-year follow-up study in China.
53 Cummings DE, Purnell JQ, Frayo RS, Schmi- glou M, Zoumakis E, Vgontzas A, et al. Leptin Diabetes Res Clin Pract. 2015 Jul;109(1):178–
dova K, Wisse BE, Weigle DS. A preprandial and hunger levels in young healthy adults af- 84.
rise in plasma ghrelin levels suggests a role in ter one night of sleep loss. J Sleep Res. 2010 80 Jackson CL, Redline S, Kawachi I, Hu FB. As-
meal initiation in humans. Diabetes. 2001 Dec;19(4):552–8. sociation between sleep duration and diabetes
Aug;50(8):1714–9. 67 Omisade A, Buxton OM, Rusak B. Impact of in black and white adults. Diabetes Care. 2013
54 Spiegel K, Tasali E, Penev P, Van Cauter E. acute sleep restriction on cortisol and leptin Nov;36(11):3557–65.
Brief communication: sleep curtailment in levels in young women. Physiol Behav. 2010 81 Tan X, Chapman CD, Cedernaes J, Benedict
healthy young men is associated with de- Apr;99(5):651–6. C. Association between long sleep duration
creased leptin levels, elevated ghrelin levels, 68 Spiegel K, Leproult R, L’hermite-Balériaux M, and increased risk of obesity and type 2 diabe-
and increased hunger and appetite. Ann In- Copinschi G, Penev PD, Van Cauter E. Leptin tes: A review of possible mechanisms. Sleep
tern Med. 2004 Dec;141(11):846–50. levels are dependent on sleep duration: rela- Med Rev. 2018 Aug;40:127–34.
55 Fu J, Wang Y, Li G, Han L, Li Y, Li L, et al. tionships with sympathovagal balance, carbo- 82 Jike M, Itani O, Watanabe N, Buysse DJ,
Childhood sleep duration modifies the poly- hydrate regulation, cortisol, and thyrotropin. Kaneita Y. Long sleep duration and health
genic risk for obesity in youth through leptin J Clin Endocrinol Metab. 2004 Nov; 89(11): outcomes: A systematic review, meta-analysis
pathway: the Beijing Child and Adolescent 5762–71. and meta-regression. Sleep Med Rev. 2018
Metabolic Syndrome cohort study. Int J Obes. 69 Fontenelle LC, Feitosa MM, Severo JS, Freitas Jun;39:25–36.
2019 Aug;43(8):1556–67. TE, Morais JB, Torres-Leal FL, et al. Thyroid 83 Azharuddin M, Kapur P, Adil M, Ghosh P,
56 Li M, Fu J, Han L, Li G, Gao S, Grant SF, et al. Function in Human Obesity: underlying Sharma M. The impact of sleep duration and
Childhood habitual sleep duration modifies Mechanisms. Horm Metab Res. 2016 Dec; sleep quality on glycaemic control in Asian
the polygenic risk for obesity through leptin 48(12):787–94. population with type 2 diabetes mellitus: A
pathway: a longitudinal study. Diabetes. 2018 70 Xu R, Huang F, Zhang S, Lv Y, Liu Q. Thyroid systematic literature review and meta-analy-
Jul;67. function, body mass index, and metabolic risk sis of observational studies. Clin Epidemiol
57 Chaput JP, Després JP, Bouchard C, Trem- markers in euthyroid adults: a cohort study. Glob Health. 2020 Mar;8(3):967–75.
blay A. Short sleep duration is associated with BMC Endocr Disord. 2019 Jun;19(1):58. 84 Lee SW, Ng KY, Chin WK. The impact of
reduced leptin levels and increased adiposity: 71 Solanki A, Bansal S, Jindal S, Saxena V, Shuk- sleep amount and sleep quality on glycemic
results from the Quebec family study. Obesity la US. Relationship of serum thyroid stimulat- control in type 2 diabetes: A systematic review
(Silver Spring). 2007 Jan;15(1):253–61. ing hormone with body mass index in healthy and meta-analysis. Sleep Med Rev. 2017 Feb;
58 Mullington JM, Chan JL, Van Dongen HP, adults. Indian J Endocrinol Metab. 2013 Oct; 31:91–101.
Szuba MP, Samaras J, Price NJ, et al. Sleep loss 17(7 Suppl 1):S167–9. 85 Ohkuma T, Fujii H, Iwase M, Ogata-Kaizu S,
reduces diurnal rhythm amplitude of leptin in 72 Sanyal D, Raychaudhuri M. Hypothyroidism Ide H, Kikuchi Y, et al. U-shaped association
healthy men. J Neuroendocrinol. 2003 Sep; and obesity: an intriguing link. Indian J Endo- of sleep duration with metabolic syndrome
15(9):851–4. crinol Metab. 2016 Jul-Aug;20(4):554–7. and insulin resistance in patients with type 2
59 Stern JH, Grant AS, Thomson CA, Tinker L, 73 Bosy-Westphal A, Hinrichs S, Jauch-Chara K, diabetes: the Fukuoka Diabetes Registry. Me-
Hale L, Brennan KM, et al. Short sleep dura- Hitze B, Later W, Wilms B, et al. Influence of tabolism. 2014 Apr;63(4):484–91.
tion is associated with decreased serum leptin, partial sleep deprivation on energy balance 86 Holliday EG, Magee CA, Kritharides L, Banks
increased energy intake and decreased diet and insulin sensitivity in healthy women. E, Attia J. Short sleep duration is associated
quality in postmenopausal women. Obesity Obes Facts. 2008;1(5):266–73. with risk of future diabetes but not cardiovas-
(Silver Spring). 2014 May;22(5):E55–61. 74 Charles LE, Gu JK, Andrew ME, Violanti JM, cular disease: a prospective study and meta-
60 Garaulet M, Sánchez-Moreno C, Smith CE, Fekedulegn D, Burchfiel CM. Sleep duration analysis. PLoS One. 2013 Nov;8(11):e82305.
Lee YC, Nicolás F, Ordovás JM. Ghrelin, sleep and biomarkers of metabolic function among 87 Wong PM, Manuck SB, DiNardo MM, Koryt-
reduction and evening preference: relation- police officers. J Occup Environ Med. 2011 kowski M, Muldoon MF. Shorter sleep dura-
ships to CLOCK 3111 T/C SNP and weight Aug;53(8):831–7. tion is associated with decreased insulin sen-
loss. PLoS One. 2011 Feb;6(2):e17435. 75 Brady EM, Bodicoat DH, Hall AP, Khunti K, sitivity in healthy white men. Sleep (Basel).
61 Motivala SJ, Tomiyama AJ, Ziegler M, Khan- Yates T, Edwardson C, et al. Sleep duration, 2015 Feb;38(2):223–31.
drika S, Irwin MR. Nocturnal levels of ghrelin obesity and insulin resistance in a multi-eth- 88 Wang X, Greer J, Porter RR, Kaur K, Youngst-
and leptin and sleep in chronic insomnia. Psy- nic UK population at high risk of diabetes. edt SD. Short-term moderate sleep restriction
choneuroendocrinology. 2009 May; 34(4): Diabetes Res Clin Pract. 2018 May; 139: 195– decreases insulin sensitivity in young healthy
540–5. 202. adults. Sleep Health. 2016 Mar;2(1):63–8.
62 Schmid SM, Hallschmid M, Jauch-Chara K, 76 Van Cauter E, Holmbäck U, Knutson K, Le 89 Rao MN, Neylan TC, Grunfeld C, Mulligan K,
Born J, Schultes B. A single night of sleep de- proult R, Miller A, Nedeltcheva A, et al. Im- Schambelan M, Schwarz JM. Subchronic
privation increases ghrelin levels and feelings pact of sleep and sleep loss on neuroendocrine sleep restriction causes tissue-specific insulin
of hunger in normal-weight healthy men. J and metabolic function. Horm Res. 2007; 67 resistance. J Clin Endocrinol Metab. 2015
Sleep Res. 2008 Sep;17(3):331–4. Suppl 1:2–9. Apr;100(4):1664–71.
63 Reynolds AC, Dorrian J, Liu PY, Van Dongen 77 Gutiérrez-Repiso C, Soriguer F, Rubio-Mar- 90 Donga E, van Dijk M, van Dijk JG, Biermasz
HP, Wittert GA, Harmer LJ, et al. Impact of tín E, Esteva de Antonio I, Ruiz de Adana MS, NR, Lammers GJ, van Kralingen KW, et al. A
five nights of sleep restriction on glucose me- Almaraz MC, et al. Night-time sleep duration single night of partial sleep deprivation induc-
tabolism, leptin and testosterone in young and the incidence of obesity and type 2 diabe- es insulin resistance in multiple metabolic
adult men. PLoS One. 2012;7(7):e41218. tes. Findings from the prospective Pizarra pathways in healthy subjects. J Clin Endocri-
study. Sleep Med. 2014 Nov;15(11):1398–404. nol Metab. 2010 Jun;95(6):2963–8.
220 Obes Facts 2021;14:214–221 Mosavat/Mirsanjari/Arabiat/Smyth/
DOI: 10.1159/000514095 Whitehead91 Pyykkönen AJ, Isomaa B, Pesonen AK, Eriks- 96 Broussard JL, Ehrmann DA, Van Cauter E, 100 Zimberg IZ, Dâmaso A, Del Re M, Carneiro
son JG, Groop L, Tuomi T, et al. Subjective Tasali E, Brady MJ. Impaired insulin signaling AM, de Sá Souza H, de Lira FS, et al. Short
sleep complaints are associated with insulin in human adipocytes after experimental sleep sleep duration and obesity: mechanisms and
resistance in individuals without diabetes: the restriction: a randomized, crossover study. future perspectives. Cell Biochem Funct.
PPP-Botnia Study. Diabetes Care. 2012 Nov; Ann Intern Med. 2012 Oct;157(8):549–57. 2012 Aug;30(6):524–9.
35(11):2271–8. 97 Knutson KL, Van Cauter E. Associations be- 101 Gangwisch JE. Epidemiological evidence for
92 Damanti S, Bourron O, Doulazmi M, Man- tween sleep loss and increased risk of obesity the links between sleep, circadian rhythms
dengue Sosso AL, Nguyen-Michel VH, Mari- and diabetes. Ann N Y Acad Sci. 2008;1129(1): and metabolism. Obes Rev. 2009 Nov; 10
ani J, et al. Relationship between sleep param- 287–304. Suppl 2:37–45.
eters, insulin resistance and age-adjusted in- 98 Ayas NT, White DP, Al-Delaimy WK, Man- 102 Jain SK, Kahlon G, Morehead L, Lieblong B,
sulin like growth factor-1 score in non son JE, Stampfer MJ, Speizer FE, et al. A pro- Stapleton T, Hoeldtke R, et al. The effect of
diabetic older patients. PLoS One. 2017 Apr; spective study of self-reported sleep duration sleep apnea and insomnia on blood levels of
12(4):e0174876. and incident diabetes in women. Diabetes leptin, insulin resistance, IP-10, and hydro-
93 Chang JK, Koo M, Kao VY, Chiang JK. Asso- Care. 2003 Feb;26(2):380–4. gen sulfide in type 2 diabetic patients. Metab
ciation of sleep duration and insulin resis- 99 Yaggi HK, Araujo AB, McKinlay JB. Sleep du- Syndr Relat Disord. 2012 Oct;10(5):331–6.
tance in Taiwanese vegetarians. BMC Public ration as a risk factor for the development of 103 Wang S, Fu W, Jiang Y, Deng L, Zhou S,
Health. 2012 Aug;12(1):666. type 2 diabetes. Diabetes Care. 2006 Mar; Yang L. Association of plasma leptin levels
94 Buxton OM, Pavlova M, Reid EW, Wang W, 29(3):657–61. with type 2 diabetes in rotating shift work
Simonson DC, Adler GK. Sleep restriction for women. Biomed Res (Aligarh). 2017 Jan;
1 week reduces insulin sensitivity in healthy 28(1).
men. Diabetes. 2010 Sep;59(9):2126–33. 104 Banks WA. Role of the blood-brain barrier
95 Grandner MA, Seixas A, Shetty S, Shenoy S. in the evolution of feeding and cognition.
Sleep duration and diabetes risk: population Ann N Y Acad Sci. 2012 Aug;1264(1):13–9.
trends and potential mechanisms. Curr Diab 105 Imayama I, Prasad B. Role of Leptin in Ob-
Rep. 2016 Nov;16(11):106. structive Sleep Apnea. Ann Am Thorac Soc.
2017 Nov;14(11):1607–21.
Sleep Curtailment and Leptin Circulation Obes Facts 2021;14:214–221 221
DOI: 10.1159/000514095You can also read