REVIEW Metformin in cancer: translational challenges
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
R31
REVIEW
Metformin in cancer: translational challenges
Ryan J O Dowling1,2, Saroj Niraula2, Vuk Stambolic1,2 and Pamela J Goodwin3
1
Division of Signalling Biology, Ontario Cancer Institute, University Health Network, Toronto, Ontario, Canada M5G 2M9
2
Princess Margaret Hospital, 610 University Avenue, Toronto, Ontario, Canada M5G 2M9
3
Division of Clinical Epidemiology, Department of Medicine, Samuel Lunenfeld Research Institute, Mount Sinai Hospital,
University of Toronto, 1284-600 University Avenue, Toronto, Ontario, Canada M5G 1X5
(Correspondence should be addressed to P J Goodwin; Email: pgoodwin@mtsinai.on.ca)
Abstract
The anti-diabetic drug metformin is rapidly emerging as a potential anti-cancer agent. Metformin, effective in treating
type 2 diabetes and the insulin resistance syndromes, improves insulin resistance by reducing hepatic gluconeogenesis
and by enhancing glucose uptake by skeletal muscle. Epidemiological studies have consistently associated metformin
use with decreased cancer incidence and cancer-related mortality. Furthermore, numerous preclinical and clinical
studies have demonstrated anti-cancer effects of metformin, leading to an explosion of interest in evaluating this agent
in human cancer. The effects of metformin on circulating insulin levels indicate a potential efficacy towards cancers
associated with hyperinsulinaemia; however, metformin may also directly inhibit tumour growth. In this review, we
describe the mechanism of action of metformin and summarise the epidemiological, clinical and preclinical evidence
supporting a role for metformin in the treatment of cancer. In addition, the challenges associated with translating
preclinical results into therapeutic benefit in the clinical setting will be discussed.
Journal of Molecular Endocrinology (2012) 48, R31–R43
Introduction bypassed the traditional Phase I pharmacokinetic/
toxicity assessment and has moved directly into Phase II
Emerging evidence from several areas of research and Phase III testing, reflecting rapid accumulation of
suggests that metformin, a commonly used anti-diabetic preclinical, clinical and epidemiological evidence that
drug, may be useful in the prevention and treatment of it may have beneficial anti-cancer effects, despite the
cancer. Metformin, a biguanide derivative, has been fact that precise mechanisms of potential anti-cancer
used for half a century to treat non-insulin-requiring action remain unresolved (Goodwin et al. 2011).
diabetes. It is a relatively safe drug, with known Current understanding of potential anti-cancer
pharmacokinetics and manageable toxicities. Its most effects of metformin raises the intriguing possibility
common toxicity is mild-to-moderate gastrointestinal of a duality of action – metformin may act directly on
discomfort, usually self-limited and ameliorated by a the tumour or it may act indirectly on the host by
graduated ramp up in dose. Its most serious toxicity, lowering insulin levels. This, along with the fact that
lactic acidosis, is rare (Bodmer et al. 2008), occurring the key host-related mediator (insulin) is a critical
once per 100 000 years of use. Lactic acidosis is more component of culture medium used in in vitro experi-
common in elderly patients (over age 80 years) and in ments, leads to enhanced challenges in translating
those with impaired renal, cardiac and/or hepatic results of preclinical research into the clinical setting,
function. Although metformin has only recently been underscoring the importance of cross-disciplinary
directly tested in conjunction with anti-cancer agents in research approaches.
the clinical setting, its common use in the treatment of Here, we summarise emerging evidence from research
diabetes has resulted in its co-administration with on humans (epidemiological, clinical and metabolic)
virtually all anti-cancer agents in diabetic cancer and from the preclinical setting (mechanistic, in vitro
patients. No evidence of important interactions of and in vivo research) suggesting that metformin has anti-
metformin with standard cancer therapies has emerged cancer effects (Fig. 1). We then integrate this informa-
through this experience. Because of this, clinical tion to develop recommendations for translational
evaluation of metformin as an anti-cancer agent has evaluation of metformin in the clinical setting.
Journal of Molecular Endocrinology (2012) 48, R31–R43 DOI: 10.1530/JME-12-0007
0952–5041/12/048–R31 q 2012 Society for Endocrinology Printed in Great Britain Online version via http://www.endocrinology-journals.org
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessR32 R J O DOWLING and others . Metformin and cancer
Epidemiologic of metformin (Memmott et al. 2010), coupled with
Metformin/cancer
associations in diabetes
emerging clinical evidence that metformin may be
associated with improved lung cancer outcomes
(reviewed below Mazzone et al. (2010) and Tan et al.
Therapeutic
Metabolic
(2011)), suggest that other factors, such as nicotine,
Associations of obesity and Evidence of metformin
insulin with risk/prognosis activity in human cancer may lead to insulin resistance in individuals with
Metformin smoking associated cancers or that non-insulin-mediated
and
cancer
mechanisms of action are important.
Although epidemiological studies have fairly consist-
Preclinical
Preclinical ently reported reduced cancer incidence and/or
In vitro evidence of
In vivo evidence of
anti-cancer activity
anti-cancer activity mortality in diabetic patients who receive metformin
in standard clinical doses (1500–2250 mg/day in
adults), these studies have important methodological
Mechanistic
limitations. Most were conducted retrospectively and
many sampled their cases from hospital or clinical
Figure 1 Evidence supporting the use of metformin in the registries rather than population-based registries,
treatment of cancer. The potential use of metformin in the
prevention and treatment of cancer is based on emerging evidence
thereby limiting external validity and introducing
from a number of research fields. Metabolic factors such as obesity potential selection biases. Inclusion criteria varied.
and hyperinsulinaemia are associated with cancer risk while Some studies did not exclude individuals with prior
epidemiological studies have demonstrated a reduced incidence diagnosis of cancer, thus introducing a possible reverse
of cancer in diabetic patients receiving metformin. Moreover, causation bias. Other studies included both invasive
preclinical studies have provided evidence of the anti-cancer
effects of metformin and defined its mechanism of action. and non-invasive cancers in their analyses (Bodmer et al.
2010). Many studies included patients exposed to a
variety of treatments for diabetes complicating the
Research on humans analysis of metformin associations. Self-reporting of key
variables such as concomitant medication use and
Epidemiologic cancer risk factors such as obesity, tobacco use and
family history may have introduced exposure biases;
Evans et al. (2005) were the first to report a potential imbalances in these factors, as well as others such as age
association of metformin use with reduced cancer inci- and severity of diabetes, may have led to confounding of
dence. In diabetics receiving metformin (as opposed associations of metformin with cancer incidence or
to other therapies), overall cancer incidence was mortality. Nonetheless, it remains biologically plausible
lowered (odds ratio (OR) 0.86 and 95% confidence that metformin use may be causally associated with
interval (95% CI) 0.73–1.02) and there was evidence of lower cancer incidence and mortality. However, caution
a dose response in relation to total duration of should be exercised in translating these observations to
use or number of prescriptions dispensed. Since then, non-diabetic patients because their physiological milieu
at least 17 epidemiological studies examining the and the cancers they develop may differ in important
association of metformin treatment of diabetes with ways from the situation in diabetic patients. Notably,
cancer incidence and mortality have reported similar insulin resistance (characterised by high levels of
findings (see Table 1), and evidence has emerged that circulating insulin and, in later stages, by high glucose
metformin use may reverse the increased cancer risk levels with or without sustained high insulin levels) may
associated with administration of insulin or insulin have been present for many years before the clinical
secretagogues (Li et al. 2009). A recent meta-analysis diagnosis of diabetes (Kendall & Bergenstal 2001),
(Decensi et al. 2010) has identified a 31% reduction in leading to the development of insulin- and/or glucose-
overall cancer incidence or mortality when metformin dependent cancers that are more sensitive to insulin-
is used in the treatment of diabetes. There is and/or glucose-lowering effects of metformin. Because
emerging evidence that metformin use is associated of this, it is possible that similar physiological and/or
with reduced risk of several common cancers, including anti-cancer effects may not be present in non-diabetics.
colorectal, pancreas, hepatocellular, breast and lung,
although not all studies have identified significant
Clinical
effects. The reduced risk of obesity-associated cancers
such as breast and colorectal is not surprising, given Retrospective clinical data suggest that metformin use in
that metformin reduces insulin levels that appear to diabetics may be associated with the development of
be important mediators of associations of obesity with cancers that differ from those seen in the absence of
cancer. Preclinical reports suggesting reduced tobacco– metformin. Specifically, in breast cancer, metformin
carcinogen-induced lung cancer burden with the use use has been associated with tumours that are more
Journal of Molecular Endocrinology (2012) 48, R31–R43 www.endocrinology-journals.org
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessMetformin and cancer . R J O DOWLING and others R33
Table 1 Epidemiological studies examining the association of metformin use by diabetics with cancer incidence and mortality
Sample Results (HR/OR/RR
Study type Outcome size Comparison Site and 95% CI) Reference
Case–control Incidence 11 876 Any vs no metformin Multiple OR 0.86 (0.73–1.02) Evans et al. (2005)
Retrospective cohort Mortality 10 309 Metformin Multiple HR 1.0 Bowker et al. (2006)
Insulin HR 1.9 (1.5–2.4)
Sulphonylureas (SU) HR 1.3 (1.1–1.6)
Case–control Incidence 390 Any vs no metformin Multiple OR 0.28 (0.13–0.57) Monami et al. (2009)
Retrospective cohort Incidence 8170 Any vs no metformin Bowel HR 0.60 (0.38–0.94) Libby et al. (2009)
mortality
Lung HR 0.70 (0.43–1.15)
Breast HR 0.60 (0.32–1.10)
Overall HR 0.63 (0.49–0.81)
Retrospective cohort Incidence 62 809 SU Breast HR (relative to Currie et al. (2009)
metformin users)
B 0.98 (0.69–1.41)
Colorectal C 1.80 (1.29–2.53)
Pancreas P 4.95 (2.74–8.96)
Prostate R 1.07 (0.76–1.49)
MetforminCSU B 0.90 (0.67–1.21)
C 1.43 (1.05–1.94)
P 0.38 (0.13–1.12)
R 1.18 (0.89–1.57)
Insulin-based B 1.07 (0.79–1.44)
C 1.69 (1.23–2.33)
P 4.63 (2.64–8.10)
R 1.10 (0.79–1.52)
Prospective cohort Mortality 1353 Any vs no metformin Multiple HR 1.47 (1.22–1.76) Landman et al. (2010)
Case–control Incidence 973 Insulin Pancreas OR 5.04 (2.38–10.7) Li et al. (2009)
Insulin secretagogues OR 1.74 (0.80–3.77)
Thiazolidinediones OR 1.65 (0.71–3.87)
Metformin OR 0.41 (0.19–0.87)
Case–control Incidence 1001 Any vs no metformin Prostate OR 0.56 (0.32–1.00) Wright & Stanford
(2009)
Case–control Incidence 1573 Insulin or SU Liver OR 2.99 (1.34–6.65) Donadon et al. (2009)
Metformin OR 0.33 (0.1–0.7)
Case–control Incidence 1524 Biguanides Liver OR 0.3 (0.2–0.6) Hassan et al. (2010)
Thiazolidinediones OR 0.3 (0.1–0.7)
SU OR 7.1 (2.9–16.9)
Insulin OR 1.9 (0.8–4.6)
Case–control Incidence 305 Any vs no metformin Breast OR 0.44 (0.24–0.82) Bodmer et al. (2010)
Prospective cohort Incidence 480 984 Any vs no metformin Colorectal HR 0.36 (0.13–0.98) Lee et al. (2011)
Liver HR 0.06 (0.02–0.16)
Pancreas HR 0.15 (0.03–0.79)
Overall HR 0.12 (0.08–0.19)
Retrospective cohort Mortality 595 Any vs no metformin Colorectal HR 1.45 (1.08–1.93) Lee et al. (2012)
Retrospective cohort Mortality 3685 Metformin Multiple HR 0.56 (0.34–0.94) Bo et al. (2012)
Insulin HR 1.56 (1.22–1.99)
Case–control Incidence 10 781 Metformin Ovarian OR 0.61 (0.30–1.25) Bodmer et al. (2011)
SU OR 1.26 (0.65–2.44)
Insulin OR 2.29 (1.13–4.65)
Nested case–control Incidence 8098 Any vs no metformin Prostate RR 1.23 (0.99–1.52) Azoulay et al. (2011)
Case–control Incidence 4323 Any vs no metformin Breast OR 0.81 (0.63–0.96) Bosco et al. (2011)
Case–control Incidence 1340 Metformin Multiple OR 0.46 (0.25–0.85) Monami et al. (2011)
SU OR 0.75 (0.39–1.45)
B, Breast Cancer; C, Colorectal Cancer; P, Pancreatic Cancer; R, Prostate Cancer; HR, Hazard Ratio; RR, Risk Ratio; OR, Odds Ratio.
frequently progesterone receptor (PgR) positive (Berstein cancer if they are receiving metformin. Jiralerspong
et al. 2010a) and less frequently triple negative (Meiers et al. (2009) studied pathological complete response
et al. 2010), whereas in lung cancer, metformin use has been (pCR) rates in breast cancer patients receiving
associated with a higher frequency of adenocarcinomas neoadjuvant chemotherapy – pCR was significantly
(vs other histologies; Mazzone et al. 2010, Tan et al. 2011). higher in diabetics receiving metformin than in
Similar retrospective data suggest that cancer out- diabetics not receiving metformin (24 vs 8%), with
comes may be better in diabetics with breast or lung intermediate pCR in non-diabetics who were not
www.endocrinology-journals.org Journal of Molecular Endocrinology (2012) 48, R31–R43
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessR34 R J O DOWLING and others . Metformin and cancer
exposed to metformin (16%). Although imbalances in ongoing studies on the metastatic and adjuvant setting
covariates such as age, obesity, insulin and taxane use in breast, prostate, pancreatic and endometrial cancer
were present, differences in pCR were significant in (clinicaltrials.gov), will provide important additional
adjusted analyses; however, metformin use was not information on the anti-cancer effects of metformin
significantly associated with survival. Likewise, metfor- and help elucidate the clinically important mechanisms
min use by patients with triple-negative breast cancer of metformin action in diabetic and non-diabetic
was not associated with beneficial effects on distant cancer patients.
metastasis-free survival, recurrence-free survival or over-
all survival (Bayraktar et al. 2012). However, patients
receiving metformin had a slightly lower risk of distant Metabolic
metastases (compared with diabetics not receiving Obesity has been associated with increased overall
metformin and non-diabetics). In a retrospective review cancer risk and increased risk of most common solid
of lung cancers in diabetics, Mazzone et al. (2010) tumours and haematological malignancies (Calle et al.
reported more frequent occurrence of metastatic 2003); lung cancer is a notable exception to this
disease at diagnosis in those receiving insulin or association. Although many factors have been postu-
thiazolidinediones (which also lower insulin; 20 vs lated to mediate effects of obesity on cancer, including
42% in those not receiving these agents, PZ0.027) and sex hormones such as oestrogen, adipocytokines such
a reduced risk of death in those receiving metformin as leptin and adiponectin, and inflammatory cytokines
(hazard ratio (HR) 0.56, PZ0.056). Recent evidence such as interleukins and tumour necrosis factor a
also suggests that chemotherapy outcomes may be (TNFa), recent research has focused on insulin (or
improved by metformin in diabetic non-small cell lung insulin resistance as part of the metabolic/insulin
cancer patients (Tan et al. 2011). Because of the resistance syndrome) as a potentially important
retrospective design of these studies and the non- mediator. In a number of meta-analyses (Everhart &
random allocation of metformin (and thiazolidine- Wright 1995, Larsson et al. 2005, 2006, 2007, Mitri et al.
diones), these results should be considered as 2008, Larsson & Wolk 2011), type 2 diabetes (associated
hypothesis generating. Nonetheless, they suggest that with a period of hyperinsulinaemia) has been associ-
clinically important beneficial effects may result from ated with increased risk of common solid tumours
metformin use in cancer patients. including those of the breast, colon/rectum, pancreas
Prospective data regarding metformin use in non- and kidney but not the prostate (Kasper & Giovannucci
diabetic cancer patients are beginning to emerge. We 2006, Kasper et al. 2009). Furthermore, higher insulin
have reported a 22% reduction in insulin levels when or C-peptide (cleaved from proinsulin when insulin is
metformin is given to non-diabetic breast cancer released) levels have also been associated with risk of
survivors in a standard clinical dose of 1500 mg/day breast, colorectal and other cancers (Pisani 2008).
(Goodwin et al. 2008). Hadad et al. (2011) have recently These observations provide credence to an insulin-
completed a preoperative, randomised, ‘window of lowering mechanism of metformin action in cancer
opportunity’ trial examining the effects of metformin prevention.
on non-diabetic women with operable invasive breast In the setting of established cancer, higher levels of
cancer. Metformin (1000 mg twice daily) was well insulin or C-peptide have been independently associ-
tolerated and caused a significant reduction in Ki-67 ated with poor outcomes (increased risk of recurrence
staining in tumours and altered the expression of and death) in breast and prostate cancers (Goodwin
numerous genes including those involved in metab- et al. 2002, Pasanisi et al. 2006, Ma et al. 2008, Emaus et al.
olism, inflammation and AMPK (PRKAA) and mTOR 2010, Duggan et al. 2011, Erickson et al. 2011, Irwin et al.
signalling. Interim data from additional ongoing 2011, Pritchard et al. 2011). Our group has demon-
neoadjuvant studies on breast cancer have provided strated a more than doubled risk of distant recurrence
evidence that metformin administration (in standard and tripled risk of death in women with locoregional
clinical dose) to newly diagnosed breast cancer patients breast cancer whose insulin levels were in the highest
is safe and has favourable effects on tumour cell quartile, even though those levels were within the
proliferation and apoptosis in the absence of other normal range (Goodwin et al. 2002). In prostate cancer,
anti-cancer treatment (Bonanni et al. 2010, Niraula et al. this association may be limited to men with body mass
2010). Furthermore, Hosono et al. (2010) have index (BMI) O25 kg/m2 (Ma et al. 2008).
reported a randomised trial showing that a very low The presence of insulin receptors (IRs) on many
dose of metformin (250 mg daily) reduces proliferation cancers provides a biological rationale for the effects
and aberrant crypt foci formation in the rectal of insulin on cancer risk and prognosis – recent under-
epithelium of non-diabetic patients with previous standing of the nature of these receptors and the
colorectal polyps when compared with placebo. signalling pathways they activate when ligand binding
Completion of these studies, as well as planned and occurs is reviewed in the following section.
Journal of Molecular Endocrinology (2012) 48, R31–R43 www.endocrinology-journals.org
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessMetformin and cancer . R J O DOWLING and others R35
Preclinical evidence AMPK (Kahn et al. 2005). The resulting increase in AMP
activates AMPK by at least three separate mechanisms
Mechanism of action of metformin as an anti-cancer (Long & Zierath 2006): i) allosteric activation,
agent ii) promotion of activation-specific phosphorylation of
the a catalytic subunit on residue Thr172 by the upstream
The role of metformin in the inhibition of cancer is kinase LKB1 (STK11) and iii) interference with de-
postulated to be associated with both direct and posphorylation of AMPK Thr172 by protein phosphatases.
indirect effects of the drug, as shown in Fig. 2. The Upon activation, AMPK phosphorylates a number of
indirect effects are linked to the ability of metformin effectors leading to the activation of ATP-generating
to inhibit the transcription of key gluconeogenesis pathways, such as glycolysis and fatty acid oxidation,
genes in the liver and stimulate glucose uptake in and the inhibition of ATP-consuming pathways, such
muscle, thus increasing insulin sensitivity and reducing as fatty acid and protein synthesis (Kahn et al. 2005).
blood glucose and lowering insulin levels. The direct
effects of metformin are believed to be primarily
mediated by activation of AMPK, a serine/threonine Direct (insulin-independent) effects of metformin
protein kinase involved in regulating cellular energy Protein synthesis is one of the most energy-consuming
metabolism, leading to a reduction in mTOR signalling processes in the cell and, as such, is a major target of
and protein synthesis in cancer cells. Metformin AMPK signalling under conditions of cellular energy
activates AMPK by inhibiting complex I of the mito- stress. Upon activation by metformin, AMPK phosphor-
chondrial respiratory chain, which leads to impaired ylates TSC2, stimulating its GTPase-activating protein
mitochondrial function and conditions that effectively (GAP) activity towards the small GTPase RHEB, which
mimic cellular energy stress (El-Mir et al. 2000, Brunmair causes a reduction in mTOR signalling (Inoki et al.
et al. 2004). Examples of these stresses include glucose 2003). mTOR controls protein synthesis by regulating
deprivation, hypoxia, oxidative stress, ischaemia and the phosphorylation of key proteins involved in mRNA
muscle contraction or exercise, all of which lead to translation, such as the 4E-BPs, S6Ks and the initiation
an increase in the ratio of AMP:ATP and activation of factor eIF4G. Inhibition of mTOR signalling leads to a
reduction in phosphorylation of its major downstream
Insulin
effectors, the 4E-BPs and S6Ks, and a net inhibition of
global protein synthesis (Zakikhani et al. 2006, Dowling
et al. 2007; Fig. 2). Reduced protein synthesis is thought
to be an important mechanism of direct metformin
Circulating insulin levels
Metformin IGF1R IR action in the inhibition of cancer cell proliferation.
Indeed, the growth-suppressive effect of metformin
PI3K in breast cancer cell lines was associated with a
OCT LKB1
OCT suppression of mTOR signalling and a general
Gluconeogenesis AMPK AMPK
inhibition of protein synthesis (Zakikhani et al. 2006,
AKT
Dowling et al. 2007).
TSC2 Considering the complexity of the molecular cascade
Liver Metformin mediating the effect of metformin on protein synthesis,
mTORC1
Cancer the status of several factors can impact metformin
cell
sensitivity. For instance, in mouse embryonic fibroblasts
Protein synthesis,
cell growth, proliferation (MEFs), loss of TSC2 leads to resistance to the effects of
metformin on mTOR signalling, protein synthesis and
Indirect Direct
cell proliferation (Dowling et al. 2007). Nevertheless, a
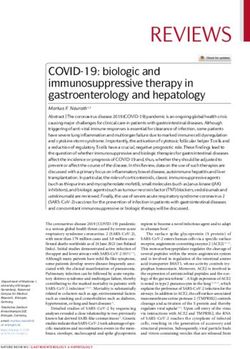
Figure 2 Mechanism of action of metformin in cancer. The anti- recent report demonstrates that in MEFs, AMPK can
cancer activity of metformin is associated with direct and indirect
effects of the drug. The direct insulin-independent effects of directly suppress mTOR in the absence of TSC2 by
metformin are mediated by activation of AMPK and a reduction in phosphorylating the mTOR-associated adaptor protein
mTOR signalling and protein synthesis in cancer cells. The raptor (Gwinn et al. 2008). The tumour suppressor
tumour suppressors LKB1 and TSC2 are important in mediating LKB1 is also an important determinant of metformin
the effects of metformin on AMPK and mTOR respectively;
however, metformin may also inhibit mTOR independently of sensitivity. As indicated earlier, LKB1 is the immediate
LKB1, AMPK and TSC2. The indirect insulin-dependent effects of AMPK activator in response to cellular energy stress and
metformin are mediated by its ability to activate AMPK and inhibit phosphorylates a key AMPK residue (Thr172) obligate
gluconeogenesis in the liver and stimulate glucose uptake in for catalytic activity. Cells lacking LKB1 exhibit
muscle. The resulting reduction in circulating insulin alleviates
activation of PI3K/AKT/mTOR signalling in cancer cells. The cell
decreased AMPK activation and elevated mTOR signal-
membrane transporter OCT1 is required for metformin uptake in ling even under conditions of cellular energy stress or
tissue and therefore may play a key role in efficacy. treatment with AMPK agonists (Shaw et al. 2004). LKB1
www.endocrinology-journals.org Journal of Molecular Endocrinology (2012) 48, R31–R43
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessR36 R J O DOWLING and others . Metformin and cancer
is also required for metformin-mediated AMPK acti- (SLC22A2), and -3 (SLC22A3)). OCT1 is primarily
vation. A variety of cells lacking LKB1, including those responsible for metformin transport into cells and
derived from breast and cervical cancers and mouse polymorphisms in the gene encoding OCT1 that affect
embryonic stem cells, are resistant to the growth hepatic uptake of metformin in vitro and have been
inhibitory effects of metformin in vitro (Zakikhani et al. associated with decreased efficacy in patients (Shu et al.
2006, Dowling et al. 2007, Huang et al. 2008). Moreover, 2007, Jin et al. 2009, Tzvetkov et al. 2009, Memmott et al.
LKB1 is required for liver AMPK activation and the 2010). OCT1 is highly expressed in liver tissue,
associated reduction in blood glucose in response to with lower levels present in the kidney and minimal
metformin treatment (Shaw et al. 2005). Thus, LKB1 levels present in the lung and small intestine (Jin et al.
and TSC2 represent key factors in determining tumour 2009, Tzvetkov et al. 2009, Memmott et al. 2010). Little is
sensitivity to the effects of metformin. known about the expression of OCT1 in human
Increased mTOR-dependent protein synthesis and tumours; however, an assessment of its expression
cell growth are hallmark features of tumorigenesis patterns in tumour tissue will be critical to elucidate
downstream of the activated PI3K/AKT signalling the mechanism of anti-tumour action of metformin
pathway, one of the most frequently deregulated and the identification of patients best suited for
molecular networks in human breast cancer. Activating metformin therapy.
mutations in the PI3K catalytic subunit (PIK3CA) have Recent reports have raised the possibility that
been found in 20–35% of primary breast specimens metformin exhibits additional inhibitory effects on
(Bachman et al. 2004, Lee et al. 2005), while mutations gluconeogensis and mTOR signalling independent of
or loss of the tumour suppressor PTEN, a negative AMPK and TSC2 (Gwinn et al. 2008, Foretz et al. 2010,
regulator of the PI3K/AKT cascade, has been found in Kalender et al. 2010). Metformin inhibited mTOR
up to 40% of breast tumours (Sansal & Sellers 2004, activity in cells lacking TSC2 and AMPK by suppressing
Perez-Tenorio et al. 2007). In addition, over-expression RAG GTPases, which are involved in mTOR activation
of HER2 (ERBB2), an upstream activator of PI3K, is (Kalender et al. 2010). Furthermore, metformin
observed in 30% of human breast cancers (Yu & Hung lowered hepatic gluconeogenesis in the absence of
2000). Notably, PI3K/AKT signalling correlates with AMPK, or its kinase, LKB1, by reducing hepatic energy
breast cancer progression and contributes to resistance levels (Foretz et al. 2010). These observations highlight
of breast cancer cells to chemotherapy, trastuzumab the need for additional research focusing on the
and tamoxifen (Zhou et al. 2004, Morgensztern & mechanism of action of metformin. Nevertheless, it
McLeod 2005). A number of physiological stimuli, appears likely that the ability of metformin to exert
including a variety of growth factors and hormones direct effects on mTOR signalling and indirect effects
such as insulin, also activate PI3K signalling in cancer on circulating insulin remain integral to its potential
cells. Considering the prevalence of genetic changes mechanism of action in the treatment of cancer.
leading to elevated mTOR signalling, targeting this
cascade using metformin represents a possibly viable
Indirect (insulin-dependent) effects of metformin
therapeutic option in breast cancer.
In addition to mTOR, other targets of AMPK may also As noted earlier, metformin may also exhibit indirect
be implicated in cancer cell proliferation and survival. effects on tumour growth by reducing circulating
For example, AMPK phosphorylates p53 (a tumour glucose and insulin levels via inhibition of hepatic
suppressor that is a downstream target of AMPK) upon gluconeogenesis and stimulation of glucose uptake in
energy stress in MEFs leading to activation of a cell cycle muscle (Fig. 2). High insulin levels associated with
checkpoint, allowing cells to survive periods of energy obesity, insulin resistance and type 2 diabetes may
deprivation (Jones et al. 2005). p53 may also impact promote tumourigenesis via activation of the foetal
sensitivity to metformin. Metformin inhibited the isoform of the IR-A, which is highly expressed in human
growth of p53-deficient human colon carcinoma cells breast cancer. The IR lies upstream of a number
in vitro and in tumour xenografts in mice but had no of growth-promoting pathways including the PI3K/
effect on p53 wild-type cells (Buzzai et al. 2007). This AKT/mTOR signalling network (Belfiore & Frasca
difference in sensitivity was attributed to the ability of 2008, Pollak 2008). The IGF1R, also proposed to be
p53 wild-type cells to undergo a metabolic adaptation, involved in breast cancer, is less highly expressed in
which maintained cell survival during periods of breast tumours but may hybridise with IR-A to bind
metformin-mediated AMPK activation. However, p53 insulin and stimulate proliferation of breast cancer cells
status did not impact metformin sensitivity in other at concentrations that do not activate IGF1R dimers
cancer cell lines (Zhuang & Miskimins 2008, Alimova (Papa & Belfiore 1996, Mulligan et al. 2007). Together,
et al. 2009). Sensitivity to the anti-tumoral effects of these observations suggest that, unlike normal adult
metformin may also be governed by expression levels of epithelial cells, breast cancer cells may acquire sensi-
the organic cation transporters (OCT1 (SLC22A1), -2 tivity to the growth and survival effects of insulin.
Journal of Molecular Endocrinology (2012) 48, R31–R43 www.endocrinology-journals.org
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessMetformin and cancer . R J O DOWLING and others R37
Reduction in insulin levels by metformin may counter human doses in the latter) reduced tumour growth
act this sensitivity by reducing ligand binding to when mice were fed a high-energy diet (which induces
IR-A/IGF1R, indirectly inhibiting tumour growth and weight gain and insulin resistance; Algire et al. 2008,
improving breast cancer outcomes. Phoenix et al. 2010). In these models, the high-energy
diet enhanced tumourigenesis, whereas metformin
significantly reduced the effect of this diet on tumour
In vivo models of anti-tumour activity of metformin growth. Metformin improved insulin sensitivity in
The effects of metformin on spontaneous breast tumour-bearing high-energy diet fed mice and resulted
tumour development have been examined in MMTV– in AMPK activation and reduced IR-mediated signalling
Her2/Neu transgenic mice that exhibit mammary- in tumours. Paradoxically, metformin failed to inhibit
specific expression of the HER2/NEU oncoprotein, the growth of tumours in mice on a control diet, despite
resulting in the almost universal development of focal activation of AMPK in tumour tissue (Algire et al. 2008).
mammary adenocarcinomas, which metastasise to the These observations are consistent with an indirect,
lungs. Metformin treatment, in a dose comparable to insulin-lowering mechanism of metformin action;
that used clinically in humans, significantly delayed the however, it must be recognised that the tumour cells
appearance of mammary adenocarcinomas, reduced were dependent on high insulin levels in culture
the size of tumours and prolonged the lifespan of medium before their injection into mice and
MMTV–Her2/Neu mice (Anisimov et al. 2005). These mechanisms may differ in the clinical setting in which
effects were accompanied by a significant reduction in this dependence is not present.
blood glucose and a statistically non-significant dimin-
ution in circulating insulin levels (Anisimov et al. 2005).
In vitro models of anti-cancer effects of metformin
In mice heterozygous for the tumour suppressor PTEN
(highly prone to tumours in various organs), metfor- In vitro work focusing on the effects of metformin on
min (administered at a dose of 300mg/kg body weight breast cancer cells demonstrated that metformin
per day, more than tenfold higher than the standard inhibited the growth of a variety of breast cancer cells
clinical dose) delayed tumour onset by 25% (Huang regardless of oestrogen receptor (ER), PR, HER2 or
et al. 2008), an effect that required LKB1-mediated p53 status (Zhuang & Miskimins 2008, Alimova et al.
AMPK activation. Metformin was also effective in 2009). Recently, it was reported that metformin
reducing the growth of intestinal polyps in mice deficient induced unique responses in the triple-negative (ER,
for the tumour suppressor APC (Tomimoto et al. 2008). PR and HER2 negative) breast cancer cell line MDAMB-
Orally administered metformin (at plasma levels 231, leading to an S phase cell cycle arrest, reduced cell
(2.7–10.3 mM) equivalent to those achieved in patients proliferation and colony formation, as well as increased
(2 . 8–15 mM)) also reduced tobacco carcinogen- apoptosis (Liu et al. 2009). In this system, metformin
induced lung tumourigenesis (4-(methylnitrosamino)- also induced AMPK activation, reduced the phosphoryl-
1-(3-pyrdyl)-1-butanone (NNK)) in mice (tumour ation of epidermal growth factor receptor (EGFR),
burden reduced by 53%; Memmott et al. 2010). MAPK and Src and lowered the levels of cyclins D1
Intraperitoneal administration, resulting in higher and E (Liu et al. 2009). Growth inhibitory effects were
plasma levels of metformin (24.2 mM), reduced tumour recapitulated in vivo where metformin significantly
burden by 72%. Although AMPK activation was reduced the growth of triple-negative breast cancer
observed in the liver and circulating insulin levels cell xenografts in nude mice. Some of the anti-
were reduced after i.p. injection, metformin failed to cancer effects of metformin on triple-negative breast
activate AMPK in lung tumour tissue. A concomitant cancer cells were also associated with STAT3 inhibition.
reduction in phosphorylation of IGF1R/IR, AKT and Treatment of triple-negative cells with metformin led to
ribosomal protein S6 in tumours suggests that the a reduction in STAT3 activation and downstream
indirect (insulin-mediated) effects of metformin were signalling and metformin acted synergistically with a
responsible for the reduction in lung tumour burden. STAT3 inhibitor to decrease cell growth and induce
In addition to spontaneous and carcinogen-induced apoptosis (Deng et al. 2012). Metformin may also be
tumours, metformin has been found to impact growth effective against ER-positive breast cancers by
in mouse xenograft and syngeneic tumour models – the inhibiting aromatase expression in tumour stroma.
tumour cells injected in these models were grown in In primary human breast adipose stromal cells,
culture media that contained high levels of glucose, metformin treatment led to an increase in the
insulin and other growth factors. In at least two phosphorylation of AMPK, which was associated with
syngeneic model systems (Lewis lung carcinoma LLC1 an inhibition of nuclear translocation of CRTC2, a
cells in C57BL/6J mice and triple negative 66c14 cells CREB co-activator known to increase aromatase
in Balb/c mice), metformin (at doses comparable to expression (Brown et al. 2010). Furthermore, metfor-
human doses in the former and w40 times higher than min interacted additively with tamoxifen to reduce
www.endocrinology-journals.org Journal of Molecular Endocrinology (2012) 48, R31–R43
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessR38 R J O DOWLING and others . Metformin and cancer
breast cancer cell proliferation (Berstein et al. 2010b). effective in preventing tumour growth and relapse in
These results indicate that metformin may represent a mice (Hirsch et al. 2009, Iliopoulos et al. 2011).
potentially effective therapy in women with ER-positive Significantly, no CD44C/CD24lo cells could be isolated
breast tumours. from mice after metformin treatment, raising the
Emerging evidence indicates that breast cancer cells possibility that metformin may specifically target
over-expressing Her2, either through gene amplifi- tumour-initiating cells. Metformin was also effective in
cation or ectopic expression, exhibit increased sensi- preventing tumour relapse in mice when combined
tivity to the growth inhibitory effects of metformin with the standard chemotherapeutic agents paclitaxel
(Vazquez-Martin et al. 2009). The effects of metformin and carboplatin, highlighting the potential application
were associated with translational suppression of HER2 of metformin as part of a combinatorial therapeutic
protein expression mediated by the inhibition of S6K1, strategy (Iliopoulos et al. 2011). However, in some
a downstream effector of mTOR (Vazquez-Martin et al. experiments the regimen of metformin administration
2009). Of interest, the mTOR inhibitor rapamycin complicates the interpretation of results (Hirsch et al.
caused similar translational suppression of erbB3 2009). Large volumes (up to 0.5 ml) of metformin
(an EGFR, also known as HER3 in humans) in breast solution were directly injected into tumour xenografts,
cancer cells and mammary tumours in mice (Liu et al. likely resulting in exposure of tumour cells to non-
2005). Taken together, these data indicate that physiological doses of the drug, as well as necrosis (due
metformin and other inhibitors of mRNA translation to direct tumoral injection). It is unclear how a
act by reducing translation of mRNAs encoding specific comparable drug delivery can be achieved in patients.
growth factor receptors. Metformin also exhibited Nonetheless, these data imply a possible benefit in
inhibitory effects on trastuzumab-resistant breast cancer combining metformin with standard chemotherapies
cells. In trastuzumab-resistant models, metformin in breast cancer treatment.
disrupted ERBB2/IGF1R complexes and significantly
reduced cell proliferation (Liu et al. 2011).
Metformin has also been reported to exert anti-
proliferative effects against a number of other cancer Limitations of preclinical models
cell types including those derived from prostate,
One of the major limitations in interpreting many
endometrial and brain tumours (Isakovic et al. 2007,
preclinical studies is the high concentration of
Ben Sahra et al. 2008, Cantrell et al. 2010). In prostate
metformin used in vitro in relation to the concentration
cancer cells, metformin treatment caused a G1 cell cycle
that can be safely obtained in the clinical setting
arrest (mediated by a reduction in cyclin D1 levels and
(Fig. 3). Most in vitro studies report using doses of
phosphorylation of Rb), as well as an increase in the
metformin between 1 and 40 mM (165–6600 mg/l),
levels of the cell cycle inhibitor p27kip, resulting in a
which is well above the feasible therapeutic plasma
strong anti-proliferative effect both in vitro and in
levels (0.465–2.5 mg/l or 2.8–15 mM) in humans
tumour xenografts in mice (Ben Sahra et al. 2008). In
(Stambolic et al. 2009). Thus, it is possible that
endometrial cancer cells, metformin induced a
metformin caused a degree of energy stress (and resul-
G1 arrest and at high doses caused apoptosis while
ting AMPK activation) in these studies that far exceeds
suppressing mTOR signalling (Cantrell et al. 2010).
effects that would be seen clinically. For example,
Finally, while causing cell cycle arrest in low-density
Phoenix et al. (2009); reported pro-angiogenic effects of
cultures of rat glioma cells, metformin induced
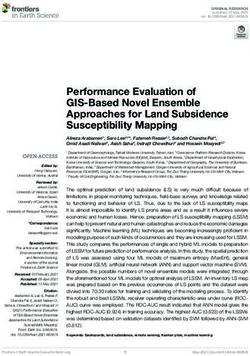
apoptosis in confluent cell cultures (Isakovic et al. 2007). Concentration of metformin
A major obstacle in the effective treatment of breast
and other cancers is the resistance of tumour cells to
drug therapy. The existence of tumour-initiating (stem)
cells, a specific subset of tumour cells that are believed
to be involved in tumour initiation, progression,
heterogeneity and recurrence, has been proposed as
one of the underlying causes of this resistance (Camp- Clinical/epidemiological In vivo In vitro
0·15–1·0 × therapeutic dose 2·0–45 × therapeutic dose 25–>1000 × therapeutic dose
bell & Polyak 2007, Polyak & Weinberg 2009). 250–2250 mg/day 750 mg/kg per day 2–50 mM
Metformin specifically inhibited the growth of
CD44C/CD24lo (a putative stem cell marker signature; Figure 3 Concentrations of metformin used in clinical and
Hirsch et al. 2009) cells in culture and reduced their preclinical studies. The anti-cancer effects of metformin have
ability to form tumours when injected into nude mice. been tested over a wide range of doses. Clinical and epidemio-
logical studies have utilised metformin at standard doses of up to
When metformin was combined with doxorubicin, a 2250 mg/day. Conversely, preclinical studies often involve extre-
striking reduction in both CD44C/CD24lo and other mely high, non-physiological concentrations of metformin that are
cancer cells was observed; this combination was also in excess of the therapeutic levels achieved in human patients.
Journal of Molecular Endocrinology (2012) 48, R31–R43 www.endocrinology-journals.org
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessMetformin and cancer . R J O DOWLING and others R39
metformin in a mouse xenograft model; however, glucose within culture media are required for
metformin concentrations were hundreds of times physiological modelling of metformin in vitro. It is
higher than those that are deemed safe clinically; it is anticipated that such models will be more likely to
possible that these extremely high concentrations led to inform clinical studies.
intracellular metabolic stresses (and responses to those
stresses) beyond those that would be seen clinically,
raising questions as to whether such pro-angiogenic
effects are clinically relevant. Translational challenges
Nonetheless, recent studies indicate that metformin
is effective at reducing cancer cell proliferation in vitro The anti-cancer effects of metformin are associated with
both direct (insulin-independent) and indirect
at concentrations as low as 10 mM, well within the
(insulin-dependent) actions of the drug. This duality
therapeutic range of the drug (Liu et al. 2009).
of action has increased the complexity of clinical
Moreover, metformin is capable of inhibiting
evaluation of metformin, including the translation of
tumour growth in mouse models at doses equivalent
preclinical observations. Existing preclinical, clinical
to those used in humans without causing toxicity
and epidemiological evidence has incorporated a broad
(Anisimov et al. 2005, Ben Sahra et al. 2008).
range of insulin, glucose and metformin concen-
Importantly, only slight levels of AMPK activation are
trations and has often focused on different potential
required to trigger downstream signalling events
mechanisms of metformin action (Fig. 3). Effects that
(Hawley et al. 2002).
have been identified in preclinical work, including
Another concern arises from the growth conditions
differential effects in different molecular subtypes of
of the cell culture models used to assess the inhibitory
breast cancer, although plausible, require confirmation
effects of metformin in vitro. The majority of cancer cell
in the clinical setting. Focused research in the
lines are grown in culture media that contains
neoadjuvant and metastatic settings, with biopsies pre-
extremely high amounts of growth factors and glucose.
and post-metformin administration, and concurrent
For example, average tissue culture media contains
evaluation of physiological effects will help to elucidate
glucose at concentrations between 10 and 25 mM, well
the clinical relevance of these effects.
above the fasting levels of glucose observed in non-
Differentiation of the relative importance of indirect
diabetic patients (!6 mM). Most media is also
(insulin-mediated) and direct (insulin-independent)
supplemented with 5–10% foetal bovine serum, which metformin effects is critical for optimal evaluation of
contains high concentrations of growth factors and this agent. The postulated mechanisms of action give
hormones, including insulin and EGF. Thus, cancer cell rise to a broad range of therapeutic targets, leading to a
lines are often maintained in non-physiological con- large number of potential clinical markers of metfor-
ditions that are optimised for maximum growth and min benefit (Table 2). Understanding the relative
proliferation. The excessive concentrations of insulin, importance of therapeutic targets and markers of
glucose and growth factors in culture media, combined benefit is required for appropriate selection of patients
with the presence of oncogenic mutations and variable who might benefit from metformin. For example, if
expression of the membrane transporter OCT1, may indirect insulin-mediated effects of metformin predo-
account for the elevated doses of metformin required minate, patient selection should target individuals with
to elicit cellular responses in vitro.
A host response is not present in vitro, and as a result, Table 2 Predictors of metformin benefit in human cancer
the direct (insulin-independent) mechanism(s) of
metformin action have been the focus of this research. Indirect Direct
Because many of the conditions evaluated in this in vitro effect effect
(insulin- (insulin-
work are outside the boundaries possible in the clinical Marker dependent) independent)
setting, it is conceivable that many of the direct effects
of metformin reported in in vitro work will not be
Host
relevant in the clinical situation. High BMI C
Thus, although a beneficial anti-cancer effect of Physical inactivity C
metformin at lower concentrations that are encoun- High fasting insulin C
tered clinically remains plausible, mechanistic effects Insulin resistance C
OCT1/2/3 expression (liver) C
identified in the preclinical studies may differ from Tumour
those that are most relevant in the clinical setting. IR/IGF1R expression C
It is therefore necessary to exercise caution in Increased PI3K/mTOR C C
further studies of the effects of metformin in vitro. OCT1/2/3 expression C
Careful dosing, equivalent to therapeutic levels in vivo, LKB1 expression C
TSC2 expression C
and strategies for varying the levels of insulin and
www.endocrinology-journals.org Journal of Molecular Endocrinology (2012) 48, R31–R43
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessR40 R J O DOWLING and others . Metformin and cancer
high insulin levels and/or obesity, germline expression Declaration of interest
of OCTs (particularly OCT1) and tumour characteristics
including IR/IGF1R expression and PI3K pathway P J G is the principal investigator and V S is the correlative science
chair of a Phase III adjuvant metformin trial (NCIC CTG MA.32).
activation. In contrast, if direct (insulin-independent) Apotex Canada, a generic drug company, supplies drug and placebo to
mechanisms of metformin action are key, tumour NCIC CTG for use in this trial.
characteristics such as LKB1 and TSC2 expression,
OCT1 positivity and PI3K/AKT/mTOR activation will
likely emerge. It is possible that the predominant
mechanism of metformin action (and key markers of Funding
activity) will differ across types of tumours. Once key
mechanisms of action (and their associated markers) The authors would like to acknowledge support from the Canadian
are understood, metformin can be used in a targeted Breast Cancer Foundation, the Ontario Institute for Cancer Research,
fashion, incorporating patient and tumour attributes the Canadian Cancer Society Research Institute, the Susan G Komen
for the Cure Foundation and the Breast Cancer Research Foundation.
consistent with known mechanisms of action. R J O D is supported by a Banting Postdoctoral Fellowship from the
Although evidence of direct (insulin-independent) Canadian Institutes of Health Research.
anti-cancer effects of metformin that has arisen from
preclinical research is strong, leading to a focus on
these direct effects by many researchers, emerging
clinical and in vivo data suggest that indirect insulin- References
mediated effects of metformin may be of key import-
ance in at least some common cancers, including breast Algire C, Zakikhani M, Blouin MJ, Shuai JH & Pollak M 2008
and lung. If this is borne out by ongoing and future Metformin attenuates the stimulatory effect of a high-energy diet on
research, the focus of preclinical research will need to in vivo LLC1 carcinoma growth. Endocrine-Related Cancer 15 833–839.
(doi:10.1677/ERC-08-0038)
shift to models that incorporate these indirect effects, Alimova IN, Liu B, Fan Z, Edgerton SM, Dillon T, Lind SE & Thor AD
requiring more complex designs than are currently 2009 Metformin inhibits breast cancer cell growth, colony
used in most in vitro research. Similarly, investigation formation and induces cell cycle arrest in vitro. Cell Cycle 8 909–915.
of markers of metformin benefit will need to include (doi:10.4161/cc.8.6.7933)
Anisimov VN, Berstein LM, Egormin PA, Piskunova TS, Popovich IG,
key host factors such as circulating insulin and glucose Zabezhinski MA, Kovalenko IG, Poroshina TE, Semenchenko AV,
levels, obesity and germline OCT1 expression, in Provinciali M et al. 2005 Effect of metformin on life span and
addition to attributes of tumour cells such as insulin/ on the development of spontaneous mammary tumors in
IGF1 receptor expression that can potentially mediate HER-2/neu transgenic mice. Experimental Gerontology 40 685–693.
(doi:10.1016/j.exger.2005.07.007)
these indirect, host-mediated effects and any direct
Azoulay L, Dell’Aniello S, Gagnon B, Pollak M & Suissa S 2011
effects that are relevant (Table 2). Metformin and the incidence of prostate cancer in patients with
Going forward, care is required to maximise the type 2 diabetes. Cancer Epidemiology, Biomarkers & Prevention 20
efficiency of evaluation of metformin as a potential 337–344. (doi:10.1158/1055-9965.EPI-10-0940)
anti-cancer agent. The known safety profile of the Bachman KE, Argani P, Samuels Y, Silliman N, Ptak J, Szabo S,
Konishi H, Karakas B, Blair BG, Lin C et al. 2004 The PIK3CA
agent allows rapid evaluation and has led to the gene is mutated with high frequency in human breast cancers.
initiation of at least one large-scale Phase III adjuvant Cancer Biology & Therapy 3 772–775. (doi:10.4161/cbt.3.8.994)
trial (NCIC CTG MA.32) in the breast cancer setting Bayraktar S, Hernadez-Aya LF, Lei X, Meric-Bernstam F, Litton JK,
(Goodwin et al. 2011). Several neoadjuvant studies are Hsu L, Hortobagyi GN & Gonzalez-Angulo AM 2012 Effect
of metformin on survival outcomes in diabetic patients with
ongoing, and studies on the metastatic and prevention triple receptor-negative breast cancer. Cancer 118 1202–1211.
settings are ongoing and planned in a number of (doi:10.1002/cncr.26439)
cancer types. It is essential that these studies include Belfiore A & Frasca F 2008 IGF and insulin receptor signaling in
strong embedded correlative research components, breast cancer. Journal of Mammary Gland Biology and Neoplasia 13
381–406. (doi:10.1007/s10911-008-9099-z)
with evaluation of host and tumour factors to identify
Ben Sahra I, Laurent K, Loubat A, Giorgetti-Peraldi S, Colosetti P,
potential predictors of metformin benefit and, more Auberger P, Tanti JF, Le Marchand-Brustel Y & Bost F 2008 The
importantly, to allow enhanced understanding of the antidiabetic drug metformin exerts an antitumoral effect in vitro
relative contributions of indirect insulin-mediated and in vivo through a decrease of cyclin D1 level. Oncogene 27
and direct insulin-independent metformin action. 3576–3586. (doi:10.1038/sj.onc.1211024)
Berstein LM, Boyarkina MP, Tsyrlina EV, Turkevich EA &
The absence of pharmaceutical industry interest in Semiglazov VF 2010a More favorable progesterone receptor
metformin (due to its generic status) has led to less phenotype of breast cancer in diabetics treated with metformin.
co-ordination of research activities than is commonly Medical Oncology 28 1260–1263. (doi:10.1007/s12032-010-9572-6)
seen in anti-cancer drug development – as a result, it is Berstein LM, Yue W, Wang JP & Santen RJ 2010b Isolated and
combined action of tamoxifen and metformin in wild-type,
essential that the research community ensures that this tamoxifen-resistant, and estrogen-deprived MCF-7 cells. Breast
function is fulfilled and that a major focus on clinical Cancer Research and Treatment 128 109–117. (doi:10.1007/s10549-
translation and relevance emerges in future research. 010-1072-z)
Journal of Molecular Endocrinology (2012) 48, R31–R43 www.endocrinology-journals.org
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessMetformin and cancer . R J O DOWLING and others R41
Bo S, Ciccone G, Rosato R, Villois P, Appendino G, Ghigo E & Grassi G et al. 2009 Antidiabetic therapy and increased risk of hepatocel-
2012 Cancer mortality reduction and metformin. A retrospective lular carcinoma in chronic liver disease. World Journal of
cohort study in type 2 diabetic patients. Diabetes, Obesity & Gastroenterology 15 2506–2511. (doi:10.3748/wjg.15.2506)
Metabolism 14 23–29. (doi:10.1111/j.1463-1326.2011.01480.x) Dowling RJ, Zakikhani M, Fantus IG, Pollak M & Sonenberg N 2007
Bodmer M, Meier C, Krahenbuhl S, Jick SS & Meier CR 2008 Metformin inhibits mammalian target of rapamycin-dependent
Metformin, sulfonylureas, or other antidiabetes drugs and the risk translation initiation in breast cancer cells. Cancer Research 67
of lactic acidosis or hypoglycemia: a nested case–control analysis. 10804–10812. (doi:10.1158/0008-5472.CAN-07-2310)
Diabetes Care 31 2086–2091. (doi:10.2337/dc08-1171) Duggan C, Irwin ML, Xiao L, Henderson KD, Smith AW,
Bodmer M, Meier C, Krahenbuhl S, Jick SS & Meier CR 2010 Long- Baumgartner RN, Baumgartner KB, Bernstein L, Ballard-Barbash R
term metformin use is associated with decreased risk of breast & McTiernan A 2011 Associations of insulin resistance and
cancer. Diabetes Care 33 1304–1308. (doi:10.2337/dc09-1791) adiponectin with mortality in women with breast cancer. Journal of
Bodmer M, Becker C, Meier C, Jick SS & Meier CR 2011 Use of Clinical Oncology 29 32–39. (doi:10.1200/JCO.2009.26.4473)
metformin and the risk of ovarian cancer: a case–control analysis. El-Mir MY, Nogueira V, Fontaine E, Averet N, Rigoulet M & Leverve X
Gynecological Oncology 123 200–204. (doi:10.1016/j.ygyno. 2000 Dimethylbiguanide inhibits cell respiration via an indirect
2011.06.038) effect targeted on the respiratory chain complex I. Journal of
Bonanni B, Cazzaniga M, Puntoni M, Pruneri G, Serrano D, Biological Chemistry 275 223–228. (doi:10.1074/jbc.275.1.223)
Lazzeroni M, Guerrieri-Gonzaga A, Macis D, Luini A, Veronesi A, Emaus A, Veierod MB, Tretli S, Finstad SE, Selmer R, Furberg AS,
et al. 2010 A randomized pre-surgical trial of metformin in breast Bernstein L, Schlichting E & Thune I 2010 Metabolic profile,
cancer. Preliminary feasibility and safety results. San Antonio Breast physical activity, and mortality in breast cancer patients. Breast
Cancer Symposium, (PD03-02). Cancer Research and Treatment 121 651–660. (doi:10.1007/s10549-
Bosco JL, Antonsen S, Sorensen HT, Pedersen L & Lash TL 2011 009-0603-y)
Metformin and incident breast cancer among diabetic women: Erickson K, Patterson RE, Flatt SW, Natarajan L, Parker BA, Heath DD,
a population-based case–control study in Denmark. Cancer Laughlin GA, Saquib N, Rock CL & Pierce JP 2011 Clinically
Epidemiology, Biomarkers & Prevention 20 101–111. (doi:10.1158/ defined type 2 diabetes mellitus and prognosis in early-stage breast
1055-9965.EPI-10-0817) cancer. Journal of Clinical Oncology 29 54–60. (doi:10.1200/JCO.
Bowker SL, Majumdar SR, Veugelers P & Johnson JA 2006 Increased 2010.29.3183)
cancer-related mortality for patients with type 2 diabetes who use Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR & Morris AD 2005
sulfonylureas or insulin. Diabetes Care 29 254–258. (doi:10.2337/ Metformin and reduced risk of cancer in diabetic patients. BMJ 330
diacare.29.02.06.dc05-1558) 1304–1305. (doi:10.1136/bmj.38415.708634.F7)
Brown KA, Hunger NI, Docanto M & Simpson ER 2010 Metformin Everhart J & Wright D 1995 Diabetes mellitus as a risk factor for
inhibits aromatase expression in human breast adipose stromal cells pancreatic cancer. A meta-analysis. Journal of the American Medical
via stimulation of AMP-activated protein kinase. Breast Cancer Research Association 273 1605–1609. (doi:10.1001/jama.1995.
and Treatment 123 591–596. (doi:10.1007/s10549-010-0834-y) 03520440059037)
Brunmair B, Staniek K, Gras F, Scharf N, Althaym A, Clara R, Roden M, Foretz M, Hebrard S, Leclerc J, Zarrinpashneh E, Soty M, Mithieux G,
Gnaiger E, Nohl H, Waldhausl W et al. 2004 Thiazolidinediones, like Sakamoto K, Andreelli F & Viollet B 2010 Metformin inhibits
metformin, inhibit respiratory complex I: a common mechanism hepatic gluconeogenesis in mice independently of the
contributing to their antidiabetic actions? Diabetes 53 1052–1059. LKB1/AMPK pathway via a decrease in hepatic energy state.
(doi:10.2337/diabetes.53.4.1052) Journal of Clinical Investigation 120 2355–2369. (doi:10.1172/
Buzzai M, Jones RG, Amaravadi RK, Lum JJ, DeBerardinis RJ, Zhao F, JCI40671)
Viollet B & Thompson CB 2007 Systemic treatment with the Goodwin PJ, Ennis M, Pritchard KI, Trudeau ME, Koo J, Madarnas Y,
antidiabetic drug metformin selectively impairs p53-deficient Hartwick W, Hoffman B & Hood N 2002 Fasting insulin and
tumor cell growth. Cancer Research 67 6745–6752. (doi:10.1158/ outcome in early-stage breast cancer: results of a prospective
0008-5472.CAN-06-4447) cohort study. Journal of Clinical Oncology 20 42–51. (doi:10.1200/
Calle EE, Rodriguez C, Walker-Thurmond K & Thun MJ 2003 JCO.20.1.42)
Overweight, obesity, and mortality from cancer in a prospectively Goodwin PJ, Pritchard KI, Ennis M, Clemons M, Graham M &
studied cohort of U.S. adults. New England Journal of Medicine 348 Fantus IG 2008 Insulin-lowering effects of metformin in women
1625–1638. (doi:10.1056/NEJMoa021423) with early breast cancer. Clinical Breast Cancer 8 501–505.
Campbell LL & Polyak K 2007 Breast tumor heterogeneity: cancer (doi:10.3816/CBC.2008.n.060)
stem cells or clonal evolution? Cell Cycle 6 2332–2338. (doi:10.4161/ Goodwin PJ, Stambolic V, Lemieux J, Chen BE, Parulekar WR,
cc.6.19.4914) Gelmon KA, Hershman DL, Hobday TJ, Ligibel JA, Mayer IA et al.
Cantrell LA, Zhou C, Mendivil A, Malloy KM, Gehrig PA & 2011 Evaluation of metformin in early breast cancer: a
Bae-Jump VL 2010 Metformin is a potent inhibitor of modification of the traditional paradigm for clinical testing
endometrial cancer cell proliferation – implications for a novel of anti-cancer agents. Breast Cancer Research and Treatment 126
treatment strategy. Gynecological Oncology 116 92–98. 215–220. (doi:10.1007/s10549-010-1224-1)
(doi:10.1016/j.ygyno.2009.09.024) Gwinn DM, Shackelford DB, Egan DF, Mihaylova MM, Mery A,
Currie CJ, Poole CD & Gale EA 2009 The influence of glucose- Vasquez DS, Turk BE & Shaw RJ 2008 AMPK phosphorylation
lowering therapies on cancer risk in type 2 diabetes. Diabetologia of raptor mediates a metabolic checkpoint. Molecular Cell 30
52 1766–1777. (doi:10.1007/s00125-009-1440-6) 214–226. (doi:10.1016/j.molcel.2008.03.003)
Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B Hadad S, Iwamoto T, Jordan L, Purdie C, Bray S, Baker L, Jellema G,
& Gandini S 2010 Metformin and cancer risk in diabetic patients: Deharo S, Hardie DG, Pusztai L et al. 2011 Evidence for biological
a systematic review and meta-analysis. Cancer Prevention Research 3 effects of metformin in operable breast cancer: a pre-operative,
1451–1461. (doi:10.1158/1940-6207.CAPR-10-0157) window-of-opportunity, randomized trial. Breast Cancer Research and
Deng XS, Wang S, Deng A, Liu B, Edgerton SM, Lind SE, Treatment 128 783–794. (doi:10.1007/s10549-011-1612-1)
Wahdan-Alaswad R & Thor AD 2012 Metformin targets Stat3 to Hassan MM, Curley SA, Li D, Kaseb A, Davila M, Abdalla EK, Javle M,
inhibit cell growth and induce apoptosis in triple-negative breast Moghazy DM, Lozano RD, Abbruzzese JL et al. 2010 Association of
cancers. Cell Cycle 11 367–376. (doi:10.4161/cc.11.2.18813) diabetes duration and diabetes treatment with the risk of
Donadon V, Balbi M, Ghersetti M, Grazioli S, Perciaccante A, hepatocellular carcinoma. Cancer 116 1938–1946. (doi:10.1002/
Della Valentina G, Gardenal R, Dal Mas M, Casarin P, Zanette G cncr.24982)
www.endocrinology-journals.org Journal of Molecular Endocrinology (2012) 48, R31–R43
Downloaded from Bioscientifica.com at 09/18/2021 12:05:23AM
via free accessYou can also read