REVIEW Autoimmune Encephalitis and Autoantibodies: A Review of Clinical Implications
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
REVIEW
Autoimmune Encephalitis and Autoantibodies: A
Review of Clinical Implications
Julien Hébert,a Alexandra Muccilli,a,b Richard A. Wennberg,a,c and David F. Tang-Waia,d,*
Background: Autoimmune encephalitis (AE) is a common cause of encephalitis. We review the most recent evi-
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
dence on this neuroimmune condition and autoantibody testing currently available.
Content: Clinical criteria, neuroimaging and electroencephalography can facilitate the diagnosis of AE prior to
obtaining autoantibody testing results, and lead to a diagnosis of AE even in the absence of a recognized antibody.
Early treatment of AE has been found to correlate with improved long-term functional and cognitive outcomes.
We suggest a clinical approach to diagnosis based on the predominant area of nervous system involvement and
the results of ancillary testing that are widely available. We also propose a 2-tiered approach to the acute manage-
ment of probable or definite AE. We, finally, provide guidance on the long-term management of AE—a challenging
and understudied area.
Summary: Much work remains to be done to improve the care of patients with AE. As understanding of the
pathophysiology and predisposing factors underlying this condition steadily increases, a more evidence-based,
targeted approach to the treatment of AE is still desired. Nonetheless, looking at the progress made over the past
2 decades, since the discovery of the first autoantibodies associated with AE, one cannot help but feel optimistic
about the road ahead.
INTRODUCTION AE, Oppenheim described the case of a young
woman who presented with agnosia, mood
Our understanding of autoimmune encephalitis changes, and aphasia in association with a gastric
(AE) has steadily progressed over the past 2 deca- cancer. Not finding any pathological evidence of
des, following a 2-way avenue connecting the pa- neoplasm within the brain at autopsy, Oppenheim
tient and the laboratory. Careful clinical hypothesized that such neurological symptoms
observation informs the search for autoantibod- might be caused by “toxic products” secreted in
ies, and autoantibody identification, in turn, leads response to the presence of cancer (1). The term
to accurate classification, targeted treatment, and “paraneoplastic neurologic syndrome” (PNS) was
better understanding of the pathophysiology of eventually coined and, in the 1980s, the “toxic
this condition. In 1888, a century before the iden- products” were identified as autoantibodies tar-
tification of the first autoantibody associated with geting the cytoplasm of neurons (2). After the
a
Department of Medicine, Division of Neurology, Division of Neurology, University of Toronto, Toronto, ON, Canada; bDepartment of Medicine,
Division of Neurology, Multiple Sclerosis Clinic, St. Michael’s Hospital, Toronto, ON, Canada; cDepartment of Medicine, Division of Neurology,
Epilepsy Clinic and Neurophysiology Lab, Toronto Western Hospital, University Health Network, Toronto, ON, Canada; dDepartment of Medicine,
Division of Neurology, Memory Clinic, Toronto Western Hospital, University Health Network, Toronto, ON, Canada.
*Address correspondence to this author at: 399 Bathurst St 5WW-441, Toronto, Ontario, M5T 2S8 Canada. E-mail david.tang-wai@uhn.ca.
Received June 20, 2021; accepted July 29, 2021.
DOI: 10.1093/jalm/jfab102
C American Association for Clinical Chemistry 2021. All rights reserved.
V
For permissions, please email: journals.permissions@oup.com.
...............................................................................................
January 2022 | 07:01 | 81–98 | JALM 81REVIEW Autoimmune Encephalitis and Autoantibodies: A Clinical Review
IMPACT STATEMENT
The care of patients with autoimmune encephalitis, including paraneoplastic autoimmune encephalitis, is
discussed in this review. We present evidence for a standardized framework of definitions for autoimmune
encephalitis, summarize the current conceptualization of autoimmune encephalitis pathophysiology, review
published literature that highlight the most high-yield diagnostic testing approach to AE, and emphasize
the need for early treatment initiation. We also synthesize the body of data emerging on epidemiology, pre-
dictors of clinical outcomes, and prognosis of this condition. The reader will have an appreciation of the
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
current body of knowledge on autoimmune encephalitis, including its application to clinical care, and its
limitations.
discovery of anti-Hu, Yo, and Ri (often referred to association, and a penchant for targeting the lim-
as “classical PNS”), the 1990s witnessed the identi- bic system (5–7).
fication of several other such neurological syn-
dromes associated with the production of DEFINITIONS: ORDER OUT OF CHAOS
intracellular antibodies (2). Together, these PNS
were characterized by not only a strong associa- The nomenclature employed in the AE literature
tion with cancer, as the name suggests, but also can be confusing, and it is not always clear what
refractoriness to immunosuppressive treatment. the term “AE” encompasses and, equally impor-
Far from restricting themselves to the brain, PNS tant, what it does not (Fig. 1). AE can be further
appeared capable of targeting the entire neuro- classified according to a combination of the fol-
axis (3). For the subset of patients with evidence lowing: degree of diagnostic certainty (i.e., possi-
of predominant limbic system involvement (e.g., ble, probable, definite), predominant region of
cognitive impairment, seizures, psychiatric symp- brain involvement (e.g., limbic, cerebellar), cancer
toms, imaging evidence of mesial temporal lobe association (paraneoplastic AE), pathophysiologic
involvement), the term “paraneoplastic limbic mechanisms (e.g., cell-surface or intracellular
encephalitis” was employed (4). autoantibodies), or specific antibody (e.g., anti-
In the mid-2000s, Dalmau et al. described a NMDAr encephalitis). Acknowledging the arbitrary
large case series of young, predominantly female and ever-evolving nature of definitions, we sug-
patients with encephalitis associated with the pro- gest the following lexicon:
duction of antibodies targeting a glutamate recep- Encephalitis: A clinical syndrome of neurological
tor localized on the neuronal cell-surface: the N- dysfunction caused by inflammation of the brain
methyl-D-aspartate receptor (NMDAr) (5). This dis- parenchyma, independent of etiology. Known
covery paved the way for the subsequent identifi- causes of encephalitis include infectious and auto-
cation of a myriad of other such syndromes, immune etiologies (8).
which collectively came to be described as AE. Autoimmune encephalitis (9, 10): Encephalitis
These syndromes share a high rate of response to caused by an autoimmune process characterized
immunosuppression, significantly lower cancer by autoantibody production. Of note, such
....................................................................................................
82 JALM | 81–98 | 07:01 | January 2022Autoimmune Encephalitis and Autoantibodies: A Clinical Review REVIEW
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
Fig. 1. Conceptual representation of the neuro-immunology disease spectrum. The greyed areas corre-
spond to syndromes affecting the brain. The dotted area corresponds to predominantly autoimmune
processes, while the checkered areas correspond to paraneoplastic processes. Syndromes with mixed
etiologies are denoted with oblique bars. NB: The surface area does not necessarily correlate with
incidence.
associated antibodies may not necessarily be in- Autoantibody-positive definite autoimmune limbic
volved in the pathophysiology of this condition encephalitis (9): (a) Detection of autoantibodies
(see following section on pathophysiology). against cell-surface, synaptic, or intracellular onco-
Autoimmune limbic encephalitis (ALE) (9): AE pre- neural antigens; (b) 2 of the following 3: (i) sub-
dominantly involving the limbic system. acute onset (progression over 5 cells/ Autoantibody-negative definite autoimmune limbic
mm3), hyperintensities on brain MRI T2 fluid- encephalitis (9): Patients can meet the highest de-
attenuated inversion recovery sequences that are gree of certainty in the diagnosis of AE despite
highly restricted to 1 or both medial temporal testing negative for autoantibodies by meeting all
lobes, or in multifocal areas involving grey matter, 3 criteria: (a) subacute onset (progression overREVIEW Autoimmune Encephalitis and Autoantibodies: A Clinical Review
brain abnormalities on T2 fluid-attenuated inver- immunosuppression and have a tendency to target
sion recovery MRI or fluorodeoxyglucose F 18 a wider breadth of the nervous system (12).
positron emission tomography imaging, and (c) ei- A growing body of knowledge is emerging on
ther CSF pleocytosis (white blood cell count >5 the putative mechanisms triggering the neuroim-
cells/mm3) or electroencephalogram (EEG) show- mune response seen in AE. Molecular mimicry is
ing epileptiform or slow-wave activity involving the thought to play a role in paraneoplastic AE, nota-
temporal lobes of autoantibody-positive definite bly in teratoma-associated NMDAr encephalitis.
autoimmune limbic encephalitis. Neoplasms can trigger AE by producing antigens
Paraneoplastic neurologic syndromes (PNS) (11): A that are normally found only in the central ner-
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
neurological syndrome that can affect any part of vous system, such as a teratoma producing neural
the nervous system, occurs in association with tissue containing the NMDAr, which is then pre-
cancer, and has an immune-mediated pathogene- sented to CD4þ T-cells and leads to the produc-
sis that is supported by the presence of specific tion of autoantibodies (10). Other mechanisms of
neuronal antibodies. action need to be invoked for the many patients
High-risk neurologic phenotypes (11): These are clini- with NMDAr encephalitis who do not have a tera-
cal neurological syndromes that are frequently asso- toma, not to mention the overwhelming majority
ciated with cancer and should therefore prompt a of patients with AE for whom no associated neo-
search for an underlying neoplasm. They include en- plasm is found (10, 13). Infectious agents repre-
cephalomyelitis, limbic encephalitis, rapidly progress- sent another possible culpable source in the
ing cerebellar syndrome, opsoclonus-myoclonus, triggering of AE. This has been particularly well-
sensory neuronopathy, enteric neuropathy, and characterized for herpes simplex virus (HSV) en-
Lambert–Eaton myasthenic syndrome. cephalitis, with up to 25% of patients, in 1 large co-
hort, developing NMDAr encephalitis after the
initial viral encephalitis. This phenomenon has also
PATHOPHYSIOLOGY OF AUTOIMMUNE been described with a number of other infections
ENCEPHALITIS AND ITS CLINICAL (10).
IMPLICATIONS Despite the compelling evidence that cancer
and infection can trigger AE, such triggers alone
We will not perform an in-depth review of the do not appear to be sufficient. It has been hy-
pathophysiology of AE [there are several excellent pothesized that other factors leading to loss of
articles already published on the topic (10)]; instead, tolerance to self are required for AE to occur.
we will focus our attention on the relation between This is supported by 2 key observations: (a) can-
the current understanding of the mechanisms un- cer patients on immune-checkpoint inhibitors,
derlying AE and its implications on clinical presenta- which allow the immune system to produce anti-
tion. One paradigm that has proven useful is a bodies targeting antigens that would otherwise
dichotomization of AE syndromes based on associ- be identified as self, have a higher incidence of
ated autoantibodies and antigen targets into two AE than those receiving different chemothera-
groups: intracellular and cell surface (see Table 1). peutic agents, and (b) patients with certain hu-
AE syndromes associated with cell-surface antibod- man leukocyte antigen haplotypes that
ies are characterized by a responsiveness to immu- predispose to other autoimmune disorder, such
nosuppression and a predilection for the limbic as type 1 diabetes or thyroid disease, appear
system; AE associated with intracellular antibodies, more likely to develop autoimmune disorders,
on the other hand, are typically poorly responsive to including AE (10).
....................................................................................................
84 JALM | 81–98 | 07:01 | January 2022Autoimmune Encephalitis and Autoantibodies: A Clinical Review REVIEW
EPIDEMIOLOGY OF AUTOIMMUNE typically affect 1 area of the nervous system be-
ENCEPHALITIS fore spreading. For instance, anti-Ri and anti-Yo
appear to have a particular penchant for the
Until the early 2010s, HSV encephalitis was the brainstem and the cerebellum, respectively (18,
most commonly identified cause of encephalitis 19). We will now turn our attention to AE syn-
(14). Recent evidence now suggests that AE is a dromes that affect the nervous system in a more
more common cause of encephalitis than all infec- selective manner.
tious causes combined (15, 16) and at least as com-
mon as the PNS identified in the 1980 and 1990s Limbic Encephalitis
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
(13). Its incidence has been estimated at between 4
A limbic encephalitis clinical presentation is
to 9 per million person-years, with substantial year-
commonly observed in patients with cell-surface
to-year increases in the incidence of diagnoses be-
autoantibodies (e.g., NMDAr, LGI1) (5, 6) and tend
tween 2016 and 2019 (13, 16, 17). NMDAr, leucine-
to respond well to early treatment with immuno-
rich, glioma inactivated 1 (LGI1), and anti-Hu are the
suppression. The classic presentation consists of
most commonly diagnosed antibodies in AE (13).
focal cognitive impairment, often associated with
The age distribution of AE follows a bimodal dis-
psychiatric symptoms, with progression, typically
tribution: a first peak consists predominantly of
over weeks, to seizures, dysautonomia, and al-
younger women (median age 20) with NMDAr en-
tered level of consciousness (7).
cephalitis, and a second peak (median age 65) is
In addition to this classical neuropsychiatric pre-
composed primarily of patients with LGI1 enceph-
sentation, more autoantibody-specific clinical pre-
alitis and paraneoplastic AE, who are predomi-
sentations can be identified within autoimmune
nantly male (13).
limbic encephalitis syndromes. For instance, while
orofacial dyskinesias are highly suggestive of ad-
CLINICAL SYNDROMES OF vanced NMDAr encephalitis (5), unusual lateral-
AUTOIMMUNE ENCEPHALITIS ized motor spasms, which have come to be
known as faciobrachial dystonic or tonic–dystonic
As previously outlined, the diagnosis of AE seizures, are pathognomonic for LGI1 encephalitis
should be made on clinical grounds. In this sec- (20–23). AE associated with contactin-associated
tion, we provide a survey of the various ways in protein-like 2 (CASPR2) autoantibodies frequently
which AE may present. For a summary of clinical presents with peripheral nerve hyperexcitability
presentation by autoantibody, see Table 2 and 3. and autonomic dysfunction (i.e., Morvan syn-
drome) (6), and AE associated with autoantibodies
Encephalomyeloneuropathy against the glycine receptor (GlyR) can develop
progressive encephalomyelitis with rigidity and
Certain AE syndromes—especially those associ-
myoclonus syndrome (24).
ated with autoantibodies targeting intraneural
antigens—can affect the entire neuroaxis seem-
ingly indiscriminately, causing a combination of Movement Disorders
peripheral neuropathies, cerebellar ataxia, move- AE associated with autoantibodies against Ig-like
ment disorders, rhombencephalitis, and limbic en- cell adhesion molecule 5 (IgLON5) commonly
cephalitis. Anti-Hu antibodies appear especially presents with parkinsonism and sleep disorders
prone to such widespread attacks on the nervous and can sometimes mimic progressive supranuclear
system (2). More commonly, AE syndromes will palsy, especially when associated with axial rigidity
.................................................................................................
January 2022 | 07:01 | 81–98 | JALM 85REVIEW Autoimmune Encephalitis and Autoantibodies: A Clinical Review
and supranuclear gaze palsy (25). Autoantibodies for AE must therefore often be made before the
against CRMP5 have been associated with chorea, results of autoantibody testing are available.
often with concurrent ageusia and anosmia (26).
Finally, stiff-person syndrome—a disorder character-
ized by continuous muscle activation leading to Neuroimaging
hyperlordosis and diffuse rigidity—has been associ- For a large proportion of patients with AE—up
ated with autoantibodies targeting glutamic acid de- to 80% in the case of NMDAr encephalitis—neuro-
carboxylase 65-kilodalton (GAD65), GlyR, dipeptidyl- imaging can be normal (34, 35). As previously
peptidase-like protein-6 (DPPX), and amphiphysin mentioned, most AE syndromes with cell-surface
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
(24, 27, 28). DPPX has also been associated with a autoantibodies have a limbic encephalitis presen-
clinical picture of tremor, myoclonus, and diarrhea tation, and, unsurprisingly, can be associated with
(28). hyperintensities of the mesial temporal lobes visi-
ble on MRI, as highlighted in the clinical criteria for
ALE. This finding, common with certain types of
Rhombencephalitis
autoantibodies, such as LGI1 encephalitis, is often
AE not uncommonly targets the brainstem, most absent in other cases of ALE (9, 35). Of note,
notably when associated with autoantibodies target- patients with disorders that areon the differential
ing the c-aminobutyric acid aminotransferase A re- diagnosis of ALE, such as infectious causes of en-
ceptor (GABAAR) (29), anti-Ri (19), and Ma1/2 (30, cephalitis or status epilepticus from nonautoim-
31). Frequently, such brainstem involvement will mune causes, may also have mesial temporal lobe
lead to ophthalmoplegia or opsoclonus-myoclonus. hyperintensities (34, 35). Hyperintensities of the
claustrum—a vastly connected structure integrat-
Cerebellum ing cortical, subcortical and limbic system activ-
ity—is another neuroimaging finding highly
Certain AE syndromes appear to predominantly
suggestive of ALE, often in the context of presen-
involve the cerebellum [e.g., AE associated with
tation with an explosive onset of seizures (36, 37).
Delta/notch-like epidermal growth factor-related
AE associated with Ma2 (31) and Ri (38) antibodies
receptor antibodies (32), mGlur1 (33), anti-Yo (18),
can present with MRI changes in the brainstem,
and anti-Ri (19)] and commonly manifest as ataxia.
reflecting the symptomatology of the syndromes as-
sociated with these autoantibodies. In addition, Ma2
DIAGNOSING AUTOIMMUNE encephalitis, which can present with movement dis-
ENCEPHALITIS: AUTOANTIBODIES AND orders, can also develop MRI hyperintensities within
COMPANY the basal ganglia (31). In the majority of cases, how-
ever, AE with movement disorders are accompanied
When the diagnosis of AE is suspected clinically, by either a normal MRI or the same limbic hyperin-
4 ancillary investigations constitute crucial compo- tensities that are noted with the more classic ALE
nents of the clinician’s diagnostic toolbox: neuro- presentation (31, 38, 39).
imaging, EEG, CSF studies, and autoantibody The use of neuroimaging in the diagnosis of AE is
testing—with the latter typically being the last re- a rapidly evolving area, and recent studies have sug-
sult available (9). Decisions regarding treatment gested that other imaging techniques, such as
....................................................................................................
86 JALM | 81–98 | 07:01 | January 2022Autoimmune Encephalitis and Autoantibodies: A Clinical Review REVIEW
fluorodeoxyglucose-positron emission tomography different and unique pattern marked by a lateral-
scans (40) and diffusion tensor imaging (41), may ized frontal lobe “DC shift” or infraslow activity and
have a role in the evaluation of AE. an associated electrodecremental response, the
lateralized infraslow activity serving as a readily
Electroencephalography identifiable EEG marker of contralateral motor
spasms (faciobrachial dystonic seizures) in LGI1
Several studies have suggested that EEG can be
encephalitis (20, 21, 46). A remarkable propensity
an extremely useful tool in the evaluation of AE,
for hyperventilation to evoke focal temporal lobe
with a normal background nearly excluding the di-
seizures has also been recognized as a diagnostic
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
agnosis (42). Some AE syndromes, moreover, ap-
feature of LGI1 encephalitis, with potential treat-
pear to have specific EEG signatures. For instance,
ment implications (45, 47).
some patients with NMDAr encephalitis show a
unique, diagnostic EEG pattern described as
“extreme delta brush” (43, 44). In addition, 2 differ- Cerebrospinal Fluid Analysis
ent EEG patterns can be diagnostic of LGI1 en- When evaluating for possible AE, CSF pleocytosis
cephalitis (Fig. 2), the first comprised of and elevated protein concentration are often inter-
extraordinarily frequent subclinical temporal lobe preted as an indicator of neuroinflammation (9, 48).
seizures in the absence of interictal epileptiform In a retrospective study of 95 patients with early ac-
discharges (20, 21, 45) and the second, an entirely tive AE, however, a fourth (25%) of patients with
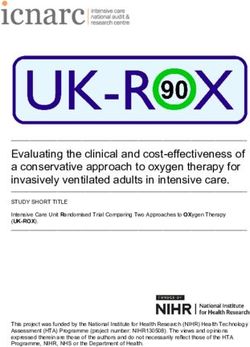
Fig. 2. EEG in LGI1 encephalitis. (A–D) Hyperventilation-induced focal temporal lobe seizures during rou-
tine EEG recording in 4 different patients (3 men, 1 woman) with LGI1 encephalitis. Arrows indicate
rhythmic electrical activity marking seizure onsets in left (A) or right (B, C, D) temporal lobes.
Hyperventilation does not normally trigger seizures in temporal lobe epilepsy—the finding is highly
suggestive of LGI1 encephalitis. Common average reference. (E) Different male patient with LGI1 en-
cephalitis and faciobrachial dystonic seizures (FBDS). A low frequency “DC-shift,” or infraslow activity,
is apparent over the right side of the brain (red EEG channels) preceding the onset of left-sided FBDS.
Arrow indicates onset of the left-sided motor spasms (average of 24 FBDS). Linked ears reference. HV,
hyperventilation; LFF, low-frequency filter; HFF, high-frequency filter.
.................................................................................................
January 2022 | 07:01 | 81–98 | JALM 87REVIEW Autoimmune Encephalitis and Autoantibodies: A Clinical Review
probable or definite AE had neither elevated CSF conversely, 22% of patients with LGI1 encephalitis
protein concentration nor pleocytosis (49). Such are autoantibody-positive in serum only (53).
noninflammatory findings on CSF studies can occur
and are particularly common in LGI1 encephalitis Special Cases
(48, 49). It is recommended that adding testing for
For certain conditions, the need to order auto-
CSF oligoclonal banding is a useful adjunct in the
antibodies is unclear, typically when a patient
evaluation of early active AE (49).
presents with a common symptom or sign occur-
ring in isolation (e.g., psychosis) without other fea-
Autoantibody Testing
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
tures of AE. This topic is covered in more detail in
Two important principles of autoantibody testing the article by Budhram et al. on common pitfalls in
in the clinical setting are: (a) treatment should ideally the diagnosis of AE (54). We will briefly discuss 3
be initiated promptly, prior to receiving the results such common presentations that may occur in
of autoantibody testing, and (b) comprehensive test- isolation (i.e., without other signs or symptoms of
ing for all autoantibodies, as opposed to testing for AE): new-onset psychosis, new-onset focal seiz-
specific autoantibodies, is usually warranted, in both ures, and dementia. We discourage routine auto-
serum and CSF. Rare exceptions to the latter princi- antibody testing for these conditions unless
ple would currently be limited to cases with the few certain conditions raising suspicion for an autoim-
identified pathognomonic clinical features (e.g., se- mune cause are met.
rum LGI1 testing for faciobrachial dystonic seizures) In a large retrospective study of 571 patients di-
or EEG findings (e.g., CSF NMDAr testing for extreme agnosed with NMDAr encephalitis, only 5 cases
delta brush on EEG in the appropriate clinical con- were reported as having had a pure psychiatric
text). Although a clinical diagnosis of AE can be presentation: of these, 2 were retrospectively
reached without the results of autoantibody testing found to have had orofacial dyskinesia, and all had
being available, or indeed even without autoanti- abnormalities on brain MRI (55). Similarly, in a re-
bodies being found (9), identifying the specific auto- view of 165 patients with an electroclinical diagno-
antibody associated with a patient’s clinical sis of temporal lobe epilepsy of more than 1-year
presentation is helpful for several reasons: it pro- duration, only 5% were found to have neural auto-
vides diagnostic closure to the patient and clinician antibodies (56), and of 50 patients diagnosed with
alike, it allows more targeted cancer screening (if in- a primary dementia, only 1 patient (2%), who had
dicated), facilitates prognostication, and may inform developed symptoms similar to progressive
treatment decisions (7). For an undifferentiated pre- supranuclear palsy over 4 months, was found to
sentation of AE, we recommend obtaining samples have AE (57).
from both serum and CSF for autoantibody testing, In addition to following the clinical criteria for
with a combination of at least 2 laboratory techni- AE, which emphasize the need for a combination
ques being employed (e.g., immunofixation assay of symptoms (e.g., psychiatric symptoms with cog-
and cell-based assay) (50). Indeed, while autoanti- nitive impairment rather than psychiatric symp-
body testing results are usually concordant between toms alone) and highlight the role of ancillary
serum and CSF samples (51), studies have shown testing (i.e., EEG, MRI, and CSF white blood cell
that 15% of patients with NMDAr encephalitis have count) (9), some additional diagnostic criteria can
autoantibody production in CSF only (52), and, aid the clinician in identifying psychosis (58), new
....................................................................................................
88 JALM | 81–98 | 07:01 | January 2022Autoimmune Encephalitis and Autoantibodies: A Clinical Review REVIEW
focal seizures (59), or dementia caused by AE (57). with improvements in long-term outcomes (61,
Generally, the rapidly progressing nature of symp- 63).
toms and refractoriness to usual treatment is In a recent survey by the Autoimmune
emphasized. Encephalitis Alliance Clinicians Network, 84% of
self-identified experts in AE reported high-dose
SERONEGATIVE BUT PROBABLE corticosteroids (1 g/day for 3–7 days) as their first-
AUTOIMMUNE ENCEPHALITIS line agent of choice: 65% said they would use this
agent alone while 19% said they would use it in
In a large national epidemiological study of AE combination with intravenous immunoglobulin
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
performed between 2016 and 2019 in France, (IvIG) or plasmapheresis (64). In the clinical prac-
23% of patients with AE were found to have nega- tice of the authors of this review, a combination of
tive autoantibody testing while meeting criteria for high-dose steroids with IvIG is favored. Of note,
probable AE (13). Much work remains to be done corticosteroids may initially lead to transient wors-
on better characterizing this subtype of patients, ening of neurocognitive symptoms, especially
who, in any case, likely represent a heterogenous symptoms of agitation and hallucinations.
group of several as-yet unidentified syndromes. In a small randomized placebo-controlled trial
Some studies have suggested that patients with from the Mayo Clinic (Rochester, MN), Dubey et al.
autoantibody-negative but probable AE are less found that patients with LGI1/CASPR2–associated
likely to develop seizures but equally likely to re- epilepsy treated with IvIG as a first-line agent had
spond to immunosuppression, thus emphasizing higher odds of seizure reduction (65). In a pro-
the importance of using clinical criteria early on to spective cohort study of 57 patients with refrac-
improve long-term outcomes in this patient popu- tory AE (Beijing, China), Zhang et al. found that
lation (60, 61). patients who receive plasmapheresis were more
likely to experience clinical improvement than
those who received other forms of immunosup-
TREATMENT OF AUTOIMMUNE pression. Forty-eight percent of patients who re-
ENCEPHALITIS ceived plasmapheresis had adverse effects,
although none were reported as being major (66).
Acute Management
Ultimately, the selection of plasmapheresis or IvIG
Studies have demonstrated that early treat- is often based on center-specific experience or
ment of AE is essential as it is associated with im- contraindications prohibiting 1 of the 2 (64).
proved long-term functional and cognitive When symptoms do not improve or continue to
outcomes (61, 62). Treatment can be divided into deteriorate, second-line immunosuppressive ther-
2 categories: tumor resection (if applicable) and apies must be considered. In a meta-analysis of
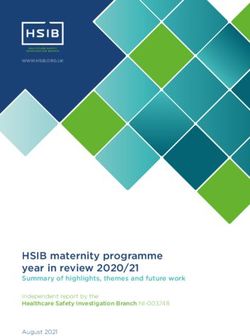
immunosuppression (Fig. 3). Only these 2 strate- 14 nonrandomized studies of patients with AE,
gies have been consistently associated with im- Nepal et al. found that administration of rituxi-
proved outcomes and can thus be thought of as mab, a CD20-cell depleting agent, was correlated
disease-modifying therapies. Although no ran- with a significant reduction in functional impair-
domized trials on tumor resection have been per- ment at follow-up. Reported complications in-
formed to date, clinical experience and cluded infusion-related reactions (16%),
retrospective studies strongly suggest that tumor pneumonia (6%), and severe sepsis (1%) (67).
removal correlates with a concurrent improve- Cyclophosphamide is considered a more afford-
ment in the patient’s symptoms of AE, as well as able second-line treatment alternative to
.................................................................................................
January 2022 | 07:01 | 81–98 | JALM 89REVIEW Autoimmune Encephalitis and Autoantibodies: A Clinical Review
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
Fig. 3. Suggested approach to the management of possible autoimmune encephalitis.
Abbreviations: AE, autoimmune encephalitis; ASM, antiseizure medications; IvIG, intravenous immunoglobulin; PLEX, plasma
exchange transfusion.
a
Based on Graus et al. (9).
b
May include workup for central nervous system infections, metabolic encephalopathy, drug toxicity, cerebrovascular dis-
ease, neoplastic disorders, Creutzfeld-Jakob disease, epileptic disorders, rheumatologic disorders, Kleine-Levin syndrome,
mitochondrial disease, or inborn errors of metabolism (9).
c
May be substituted by whole-body positron emission tomography scan.
d
May be substituted by pelvic and abdominal ultrasound.
e
This might vary based on institution and geographic localization.
f
Consult with the surgical team regarding risks of surgery on immunosuppression.
....................................................................................................
90 JALM | 81–98 | 07:01 | January 2022Autoimmune Encephalitis and Autoantibodies: A Clinical Review REVIEW
rituximab (64). Its usage is, however, limited by the The decision regarding the need for ongoing im-
potential for significant toxicities (infertility, myelo- munosuppression is one of the most difficult that
suppression, and increased risk of malignancy) must be made by clinicians caring for patients
(68). Given their respective mechanisms of with AE. In the absence of clear prospective stud-
actions, it has been suggested that rituximab be ies or guidelines on this matter (69), the impor-
favored for antibody-mediated AE (i.e., AE associ- tance of informed consent and having a dialogue
ated with antibodies targeting cell-surface anti- with the patient and the caregiver must be em-
gens) and that cyclophosphamide be reserved for phasized. Such discussions should weigh the risk
cell-mediated AE syndromes (i.e., AE with intracel- of AE relapse against the potential side effects of
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
lular antigen-targeting antibodies) (64). Of note, long-standing immunosuppression. The risk of AE
bridging immunotherapy, typically consisting of a relapse has been estimated at 12% over 2 years
tapering course of corticosteroids, is often ad- for patients with NMDAr encephalitis (52),
vised upon discharge from the hospital, with pos- although this is likely higher for other AE
sible addition of a steroid-sparing agent (see syndromes, such as LGI1 encephalitis (71).
following discussion on long-term management)
(64). Symptomatic Management
Symptomatic management of AE, especially in
Long-Term Management the acute phase, includes the use of antiseizure
Long-term management of AE is one of the medication, albeit with the understanding that
most challenging aspects of caring for patients this rarely leads to clinical improvement without
with this condition, in large part due to a paucity the concurrent use of immunosuppression or tu-
of clear evidence and guidelines. There are 2 ma- mour resection (72, 73). Of note, sodium-channel
jor aspects to long-term management of AE: (a) blockers have been found to be more effective
cancer screening and (b) decisions surrounding than other antiseizure medications at controlling
ongoing immunosuppression. undifferentiated seizures in LGI1-associated AE
Performing appropriate cancer screening, often (72). Alone or in combination with sodium-channel
guided by the results of autoantibody testing, con- blockers, a cycling regimen of acetazolamide—for
stitutes an important element of managing the reasons yet to be fully elucidated—can lead to a
long-term phase of AE. Although there is currently remarkable improvement in hyperventilation-
no consensus regarding the frequency of cancer sensitive temporal lobe pilomotor seizures, a phe-
screening after the initial presentation of AE (69), nomenon the authors have now observed in 4 pa-
we follow the recommendation of the European tient with LGI1 encephalitis (47). Benzodiazepines,
Federation of the Neurological Societies and per- antipsychotics, and mood stabilizers have all been
form cancer screening every 6 to 12 months for suggested as possible adjuncts to immunosup-
4 years after diagnosis, especially for syndromes pression in the treatment of the psychiatric symp-
with a known higher association with cancers (69, toms of AE. Movement disorders can generally be
70). Our preferred method of screening is a treated in the same fashion as similar movement
whole-body fluorodeoxyglucose-positron emis- disorders of a nonimmune etiology. The dysauto-
sion tomography, with additional directed screen- nomia that can be seen in advanced cases of AE is
ing based on the results of antibody testing and usually best addressed in intensive care unit
the age of the patient (69). settings (69).
.................................................................................................
January 2022 | 07:01 | 81–98 | JALM 91REVIEW Autoimmune Encephalitis and Autoantibodies: A Clinical Review
Table 1. Pathophysiology of autoimmune encephalitis and clinical correlates.
Antibody target Intracellular Cell surface/synaptic receptor
Examples of antibodies Hu, Yo, Ri, CRMP5, Ma2 NMDAR, LGI1, CASPR2,a AMPAR,b
GABA-Bc
Predominant areas of involvement Entire nervous system, including the Limbic system predominantly affected,
limbic system, basal ganglia, but can also affect basal ganglia, and
cerebellum, brainstem, spinal cord, peripheral nervous system.
dorsal root ganglia, and nerves.
Clinical syndromes Encephalomyelitis, paraneoplastic limbic Limbic encephalitis, movement
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
encephalitis, chorea, parkinsonism, disorders, peripheral nerve
cerebellar degeneration, hyperexcitability syndromes
opsoclonus-myoclonus, stiff person
syndrome
Association with cancer þþþ Uncommon (610%) (13), except for
teratoma
Immune cells predominantly involved T-cell mediated B-cell mediated
Response to immunosuppression Often poor Often excellent response
a
Contactin-associated protein-like 2.
b
Alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor.
c
c-aminobutyric acid aminotransferase.
OUTCOMES OF AUTOIMMUNE outcomes in NMDAr encephalitis, delay to immu-
ENCEPHALITIS nosuppression appears to be the most consistent,
highlighting the importance of early treatment ini-
The sense among the neuroscientific commu- tiation for suspected cases of AE (61, 74).
nity that the initial identification of cell-surface Interestingly, the specific autoantibody types have
autoantibodies marked a watershed moment can been inconsistently found to correlate with out-
hardly be exaggerated: a diagnosis and treatment comes (74).
path was now clearly recognizable for (often
young) patients who would have otherwise been
previously diagnosed with "encephalitis of un- CONCLUSIONS
known etiology". The seminal case series of
patients with NMDAr encephalitis by Dalmau et al. Much work remains to be done to improve the
reported that 47% of patients had full functional care of patients with AE: we are just starting to un-
recovery, 28% had mild stable deficits, 18% had derstand the pathophysiology and predisposing
severe deficits, and 7% died (5). Such relatively fa- factors underlying this condition; we have only a
vorable functional outcomes were subsequently rough estimate of the incidence of the condition,
replicated in studies of other AE syndromes asso- and there is a dire need for a more evidence-
ciated with cell-surface antibodies (74). Behind based targeted approach to the treatment of AE.
these overall optimistic figures on functional out- Nonetheless, looking at the progress made over
comes lies, however, high rates of persistent cog- the past 2 decades since the discovery of the first
nitive impairment (61). Amid the plethora of autoantibodies associated with AE, one cannot
variables that have been suggested to predict help but feel optimistic about the road ahead.
....................................................................................................
92 JALM | 81–98 | 07:01 | January 2022Table 2. Clinical syndromes of AE associated with cell-surface autoantibodies.
Demographics Limbic systema Basal ganglia Cancer association
Median Sex
age ratio Movement Brain Cere Cancer
Antibody (years) (F:M) Cognition Psychiatric Seizures disorders SPS Description stem bellum ANS PNS Others % types
AK5 (75) 66 1:4 þþþ þþþ þ 0
AMPAR (76) 53 5:1 þþ þþþ þþ þ þ þ 67 Thymus, lung,
breast, ovarian
CASPR2 (6) 66 1:4 þ þ þ þþþ þþþ Morvan syndrome, 20 Thymus,
Isaac Syndrome melanoma
DNER (32) 28 1:4 þ þ þ þþþ þ 90 Hodgkin’s
Lymphoma
DPPX (28) 57 1:4 þþþ þþþ þþþ þþ þþ Tremor, þþþ Diarrhea, Weight loss, 30 Lymphoma
myoclonus hyperekplexia
GABAAR (29) 22 1:2 þþ þ þþþ þ þ þ þ OMSTable 3. Clinical syndromes of AE associated with synaptic intracellular autoantibodies.
Demographics Limbic systema Basal ganglia Cancer association
Median Sex
age ratio Movement Brain- Cere Cancer
Antibody (years) (F:M) Cognition Psychiatric Seizures disorders SPS Description stem bellum ANS PNS Others % types
Amphiphy-sin (80) 64 1:3 þþ þþ þ þ þþ þ Encephalomyelitis, 85 Breast,
OMS Ovarian
ANNA-1 (anti-Hu) (2) 63 1:4 þþ þþ þþ þþ Myoclonus þþ þþ þþ Encephalomyelitis, OMS, 90 SCLC,
sensory neuronopathy, prostate
cranial neuropathies
ANNA-2 (anti-Ri) (19) 65 2:1 þ þ þ þ Jaw dystonia, þþ þþþ þ OMS, dysphagia, diplopia, 60 Breast,
parkinsonism, encephalomyelitis, LEMS ovarian,
chorea SCLC, Bladder
ANNA-3 (81) 65 1:1 þ þ þ þþ þ þþþ Sensory neuronopathy 60 Lung
CRMP5 (anti-CV2) (26) 60 1:1 þ þ þ þ Chorea þ þþ þþ LEMS, retinopathy, 75 SCLC, thymus
cranial neuropathy,
uveitis
GAD-65 (27) 46 3:1 þ þ þþ þ þþ þ þ Diabetes, thyroid disease, 4 Thyroid,
myelopathy, nystagmus breast, lung
GFAP (82) 50 1:1 þ þ þ þ þ þ þ Optic ataxia, 14 Ovarian,
meningoencephalomyelitis lung, breast
Ma1 (30) 60 3:1 þ þþþ þþ Dysphagia 25 Testes,
breast, colon
Ma2 (31) 50 2:1 þþ þþ þþ þ þþ þ Ophthalmoplegia 75 Testes
PCA-1 (Anti-Yo) (18) 52 5:1 þ þþþ þþ 90 Ovary, Uterus,
breast, SCLC
PCA-2 (83) 62 3:1 þ þ þ þþ þ þ þ 90 Lung
SOX-1b (84) þþ þþ þ þ þþ LEMS, OMS 80 SCLC
ZIC-4b (85) 67 1:8 þ þ þ þþþ þ þ LEMS 80 Lung
Abbreviations: ANNA, antineuronal nuclear antibody; ANS, autonomic nervous system; CRMP-5, collapsing response mediator protein 5; GAD-65, glutamic acid decarboxylase 65-kilodalton; GFAP, glial fibrillary acidic protein; PCA,
Purkinje cell cytoplasmic antibody; PNS, peripheral nervous system; SCLC, small cell lung cancer; SOX-1, sex determining region Y box 1 transcription factor; SPS, stiff-person syndrome.
a
Limbic encephalitis is defined as cognitive, epileptic, and/or psychiatric symptoms.
b
Interpret low titers with caution.
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022Autoimmune Encephalitis and Autoantibodies: A Clinical Review REVIEW
Nonstandard Abbreviations: AEautoimmune encephalitis; PNS, paraneoplastic neurologic syndrome; NMDAr, N-methyl-D-as-
partate receptor; ALE, autoimmune limbic encephalitis; CSF, cerebrospinal fluid; EEG, electroencephalogram; HSV, herpes sim-
plex virus; LGI1, leucine-rich, glioma inactivated 1; IvIG, intravenous immunoglobulin.
Author Contributions: All authors confirmed they have contributed to the intellectual content of this paper and have met the follow-
ing 4 requirements: (a) significant contributions to the conception and design, acquisition of data, or analysis and interpretation of
data; (b) drafting or revising the article for intellectual content; (c) final approval of the published article; and (d) agreement to be ac-
countable for all aspects of the article thus ensuring that questions related to the accuracy or integrity of any part of the article are ap-
propriately investigated and resolved.
Authors’ Disclosures or Potential Conflicts of Interest: No authors declared any potential conflicts of interest.
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
References
1. Schulz P, Prüss H. “Hirnsymptome bei Carcinomatose”— Neuroimmunol Neuroinflamm 2021;8:e1014.
Hermann Oppenheim and an early description of a 12. Lancaster E, Dalmau J. Neuronal autoantigens—
paraneoplastic neurological syndrome. J Hist Neurosci pathogenesis, associated disorders and antibody testing.
2015;24:371–7. Nat Rev Neurol 2012;8:380–90.
2. Senties-Madrid H, Vega-Boada F. Paraneoplastic 13. Hébert J, Riche B, Vogrig A, Mun~ iz-Castrillo S, Joubert B,
syndromes associated with anti-Hu antibodies. Isr Med Picard G, et al. Epidemiology of paraneoplastic
Assoc J 2001;3:94–103. neurologic syndromes and autoimmune encephalitides
3. Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, in France. Neurol Neuroimmunol Neuroinflamm 2020;7:
Grisold W, et al. Recommended diagnostic criteria for e883.
paraneoplastic neurological syndromes. J Neurol 14. Parpia AS, Li Y, Chen C, Dhar B, Crowcroft NS.
Neurosurg Psychiatry 2004;75:1135–40. Encephalitis, Ontario, Canada, 2002–2013. Emerg Infect
4. Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner JB, Dis 2016;22:426–32.
Dalmau J. Paraneoplastic limbic encephalitis: neurological 15. Gable M, Sheriff H, Dalmau J, Tilley D, Glaser C. The
symptoms, immunological findings and tumour frequency of autoimmune N-methyl-d-aspartate receptor
association in 50 patients. Brain 2000;123:1481–94. encephalitis surpasses that of individual viral etiologies in
5. Dalmau J, Gleichman A J, Hughes EG, Rossi JE, Peng X, Lai young individuals enrolled in the California Encephalitis
M, et al. Anti-NMDA-receptor encephalitis: case series Project. Clin Infect Dis 2012;54:899–904.
and analysis of the effect of antibodies. Lancet Neurol 16. Dubey D, Pittock SJ, Kelly CR, McKeon A, Lopez-Chiriboga
2008;7:1091–8. AS, Lennon VA, et al. Autoimmune encephalitis
6. Gadoth A, Pittock SJ, Dubey D, McKeon A, Britton JW, epidemiology and a comparison to infectious
Schmeling JE, et al. Expanded phenotypes and outcomes encephalitis. Ann Neurol 2018;83:166–77.
among 256 LGI1/CASPR2-IgG-positive patients. Ann 17. Vogrig A, Gigli GL, Segatti S, Corazza E, Marini A,
Neurol 2017;82:79–92. Bernardini A, et al. Epidemiology of paraneoplastic
7. Irani SR, Gelfand JM, Al-Diwani A, Vincent A. Cell-surface neurological syndromes: a population-based study. J
central nervous system autoantibodies: clinical relevance Neurol 2020;267:26–35.
and emerging paradigms. Ann Neurol 2014;76:168–84. 18. Tsukamoto T, Yamamoto H, Iwasaki Y, Yoshie O, Terunuma
8. Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, H, Suzuki H. Antineural autoantibodies in patients with
Bitnun A, et al.; International Encephalitis Consortium. paraneoplastic cerebellar degeneration. Arch Neurol
Case definitions, diagnostic algorithms, and priorities in 1989;46:1225–9.
encephalitis: consensus statement of the International 19. Pittock SJ, Lucchinetti CF, Lennon VA. Anti-neuronal
Encephalitis Consortium. Clin Infect Dis 2013;57: nuclear autoantibody type 2: paraneoplastic
1114–28. accompaniments. Ann Neurol 2003;53:580–7.
9. Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci 20. Andrade DM, Tai P, Dalmau J, Wennberg R. Tonic seizures:
T, et al. A clinical approach to diagnosis of autoimmune a diagnostic clue of anti-LGI1 encephalitis? Neurology
encephalitis. Lancet Neurol 2016;15:391–404. 2011;76:1355–7.
10. Vogrig A, Mun ~ iz-Castrillo S, Desestret V, Joubert B, 21. Andrade D, Tai P, Dalmau J, Wennberg R. Tonic seizures: a
Honnorat J. Pathophysiology of paraneoplastic and diagnostic clue of anti-LGI1 encephalitis? Neurology
autoimmune encephalitis: genes, infections, and 2011;77:2140; author reply 2141–3.
checkpoint inhibitors. Ther Adv Neurol Disord 2020;13: 22. Navarro V, Kas A, Apartis E, Chami L, Rogemond V, Levy P,
1756286420932797. et al. Motor cortex and hippocampus are the two main
11. Graus F, Vogrig A, Mun ~ iz-Castrillo S, Antoine J-CG, cortical targets in LGI1-antibody encephalitis. Brain 2016;
Desestret V, Dubey D, et al. Updated diagnostic criteria 139:1079–93.
for paraneoplastic neurologic syndromes. Neurol 23. Irani SR, Michell AW, Lang B, Pettingill P, Waters P,
.................................................................................................
January 2022 | 07:01 | 81–98 | JALM 95REVIEW Autoimmune Encephalitis and Autoantibodies: A Clinical Review
Johnson MR, et al. Faciobrachial dystonic seizures 38. Luque FA, Furneaux HM, Ferziger R, Rosenblum MK,
precede Lgi1 antibody limbic encephalitis. Ann Neurol Wray SH, Schold SC, et al. Anti-Ri: an antibody associated
2011;69:892–900. with paraneoplastic opsoclonus and breast cancer. Ann
24. Piquet AL, Khan M, Warner JEA, Wicklund MP, Bennett JL, Neurol 1991;29:241–51.
Leehey MA, et al. Novel clinical features of glycine 39. Baizabal-Carvallo JF, Jankovic J. Autoimmune and
receptor antibody syndrome: a series of 17 cases. Neurol paraneoplastic movement disorders: an update. J Neurol
Neuroimmunol Neuroinflamm 2019;6:e592. Sci 2018;385:175–84.
25. Honorat JA, Komorowski L, Josephs KA, Fechner K, St 40. Probasco JC, Solnes L, Nalluri A, Cohen J, Jones KM, Zan E,
Louis EK, Hinson SR, et al. IgLON5 antibody: Neurological et al. Decreased occipital lobe metabolism by FDG-PET/
accompaniments and outcomes in 20 patients. Neurol CT: an anti–NMDA receptor encephalitis biomarker.
Neuroimmunol Neuroinflamm 2017;4:e385. Neurol Neuroimmunol Neuroinflamm 2018;5:e413.
26. Yu Z, Kryzer TJ, Griesmann GE, Kim K, Benarroch EE, 41. Phillips OR, Joshi SH, Narr KL, Shattuck DW, Singh M, Di
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
Lennon VA. CRMP-5 neuronal autoantibody: marker of Paola M, et al. Superficial white matter damage in anti-
lung cancer and thymoma-related autoimmunity. Ann NMDA receptor encephalitis. J Neurol Neurosurg
Neurol 2001;49:146–54. Psychiatry 2018;89:518–25.
27. Budhram A, Sechi E, Flanagan EP, et al. Clinical spectrum 42. Limotai C, Denlertchaikul C, Saraya AW, Jirasakuldej S.
of high-titre GAD65 antibodies. J Neurol Neurosurg Predictive values and specificity of
Psychiatry 2021;92:645–54. electroencephalographic findings in autoimmune
28. Hara M, Arin ~ o H, Petit-Pedrol M, Sabater L, Titulaer MJ, encephalitis diagnosis. Epilepsy Behav 2018;84:29–36.
Martinez-Hernandez E, et al. DPPX antibody–associated 43. Sonderen AV, Arends S, Tavy DLJ, Bastiaansen AEM, Bruijn
encephalitis: main syndrome and antibody effects. MAAMD, Schreurs MWJ, et al. Predictive value of
Neurology 2017;88:1340–8. electroencephalography in anti-NMDA receptor
29. Petit-Pedrol M, Armangue T, Peng X, Bataller L, Cellucci T, encephalitis. J Neurol Neurosurg Psychiatry 2018;89:
Davis R, et al. Encephalitis with refractory seizures, status 1101–6.
epilepticus, and antibodies to the GABAA receptor: a 44. Schmitt S, Pargeon K, Frechette E, Hirsch L, Dalmau J,
case series, characterisation of the antigen, and analysis Friedman D. Extreme delta brush: a unique EEG pattern
of the effects of antibodies. Lancet Neurol 2014;13: in adults with anti-NMDA receptor encephalitis.
276–86. Neurology 2012;79:1094–100.
30. Dalmau J, Gultekin SH, Voltz R, Hoard R, DesChamps T, 45. Steriade C, Mirsattari S, Murray B, Wennberg R.
Balmaceda C, et al. Ma1, a novel neuron- and testis- Subclinical temporal EEG seizure pattern in LGI1-
specific protein, is recognized by the serum of patients antibody-mediated encephalitis. Epilepsia 2016;57:
with paraneoplastic neurological disorders. Brain 1999; e155-160–e160.
122(Pt 1):27–39. 46. Wennberg R, Steriade C, Chen R, Andrade D. Frontal
31. Dalmau J, Graus F, Villarejo A, et al. Clinical analysis of infraslow activity marks the motor spasms of anti-LGI1
anti-Ma2-associated encephalitis. Brain 2004;127: encephalitis. Clin Neurophysiol 2018;129:59–68.
1831–44. 47. Wennberg R, Maurice C, Carlen PL, Garcia Dominguez L.
32. Greene M, Lai Y, Baella N, Dalmau J, Lancaster E. Pilomotor seizures marked by infraslow activity and
Antibodies to delta/notch-like epidermal growth factor– acetazolamide responsiveness. Ann Clin Transl Neurol
related receptor in patients with anti-Tr, paraneoplastic 2019;6:167–73.
cerebellar degeneration, and Hodgkin lymphoma. JAMA 48. Blinder T, Lewerenz J. Cerebrospinal fluid findings in
Neurol 2014;71:1003–8. patients with autoimmune encephalitis-a systematic
33. Lopez-Chiriboga AS, Komorowski L, Kümpfel T, Probst C, analysis. Front Neurol 2019;10:804.
Hinson SR, Pittock SJ, et al. Metabotropic glutamate 49. Hébert J, Gros P, Lapointe S, Amtashar FS, Steriade C,
receptor type 1 autoimmunity: clinical features and Maurice C, et al. Searching for autoimmune encephalitis:
treatment outcomes. Neurology 2016;86:1009–13. beware of normal CSF. J Neuroimmunol 2020;345:
34. Giordano A, Fazio R, Gelibter S, Minicucci F, Vabanesi M, 577285.
Anzalone N, et al. Diagnosing autoimmune encephalitis 50. Ricken G, Schwaiger C, De Simoni D, Pichler V, Lang J,
in a real-world single-centre setting. J Neurol 2020;267: Glatter S, et al. Detection methods for autoantibodies in
449–60. suspected autoimmune encephalitis. Front Neurol 2018;
35. Kelley B, Patel S, Marin H, Corrigan J, Mitsias P, Griffith B. 9:841.
Autoimmune encephalitis: pathophysiology and imaging 51. Bien CG, Bien CI, Dogan Onugoren M, De Simoni D, Eigler
review of an overlooked diagnosis. A JNR AM J V, Haensch C-A, et al. Routine diagnostics for neural
Neuroradiol 2017;38:1070–8. antibodies, clinical correlates, treatment and functional
36. Steriade C, Tang-Wai DF, Krings T, Wennberg R. Claustrum outcome. J Neurol 2020;267:2101–14.
hyperintensities: a potential clue to autoimmune 52. Titulaer MJ, McCracken L, Gabilondo I, Armangué T,
epilepsy. Epilepsia Open 2017;2:476–80. Glaser C, Iizuka T, et al. Treatment and prognostic factors
37. Ayatollahi P, Tarazi A, Wennberg R. Possible autoimmune for long-term outcome in patients with anti-NMDA
encephalitis with claustrum sign in case of acute SARS- receptor encephalitis: an observational cohort study.
CoV-2 infection. Can J Neurol Sci 2021;48:430–2. Lancet Neurol 2013;12:157–65.
....................................................................................................
96 JALM | 81–98 | 07:01 | January 2022Autoimmune Encephalitis and Autoantibodies: A Clinical Review REVIEW
53. Mun ~ iz-Castrillo S, Haesebaert J, Thomas L, Vogrig A, Pinto efficacy of plasma exchange in patients with autoimmune
A-L, Picard G, et al. Clinical and prognostic value of encephalitis. Ann Clin Transl Neurol 2021;8:763–73.
immunogenetic characteristics in anti-LGI1 encephalitis. 67. Nepal G, Shing YK, Yadav JK, Rehrig JH, Ojha R, Huang DY,
Neurol Neuroimmunol Neuroinflamm 2021;8:e974. et al. Efficacy and safety of rituximab in autoimmune
54. Budhram A, Yang L, Bhayana V, Mills JR, Dubey D. Clinical encephalitis: a meta-analysis. Acta Neurol Scand 2020;
sensitivity, specificity, and predictive value of neural 142:449–59.
antibody testing for autoimmune encephalitis. J Appl Lab 68. Shin Y-W, Lee S-T, Park K-I, Jung K-H, Jung K-Y, Lee SK, et
Med 2022;7:350–56. al. Treatment strategies for autoimmune encephalitis.
55. Kayser MS, Titulaer MJ, Gresa-Arribas N, Dalmau J. Ther Adv Neurol Disord 2018;11:1756285617722347.
Frequency and characteristics of isolated psychiatric 69. Abboud H, Probasco J, Irani SR, et al. Autoimmune
episodes in anti–N-methyl-d-aspartate receptor encephalitis: proposed recommendations for
encephalitis. JAMA Neurol 2013;70:1133–9. symptomatic and long-term management. J Neurol
Downloaded from https://academic.oup.com/jalm/article/7/1/81/6498256 by guest on 19 January 2022
56. Nóbrega-Jr AW, Gregory CP, Schlindwein-Zanini R, Neves Neurosurg Psychiatry 2021;92(8):897–907
FDS, Wolf P, Walz R, et al. Mesial temporal lobe epilepsy 70. Titulaer MJ, Soffietti R, Dalmau J, Gilhus NE, Giometto B,
with hippocampal sclerosis is infrequently associated Graus F, et al.; European Federation of Neurological
with neuronal autoantibodies. Epilepsia 2018;59: Societies. Screening for tumours in paraneoplastic
e152–e156. syndromes: report of an EFNS Task Force: screening for
57. C¸oban A, Ismail Küçükali C, Bilgiç B, Yalçınkaya N, Haytural tumours in PNS. Eur J Neurol 2011;18:19–e3.
H, Ulusoy C, et al. Evaluation of incidence and clinical 71. Arin~ o H, Armangué T, Petit-Pedrol M, Sabater L, Martinez-
features of antibody-associated autoimmune Hernandez E, Hara M, et al. Anti-LGI1-associated cogntive
encephalitis mimicking dementia. Behav Neurol 2014; impairment. Neurology 2016;87:759–64.
2014:935379. 72. Feyissa AM, Lamb C, Pittock SJ, Gadoth A, McKeon A,
58. Pollak TA, Lennox BR, Müller S, Benros ME, Prüss H, Klein CJ, et al. Antiepileptic drug therapy in autoimmune
Tebartz van Elst L, et al. Autoimmune psychosis: an epilepsy associated with antibodies targeting the leucine-
international consensus on an approach to the diagnosis rich glioma-inactivated protein 1. Epilepsia Open 2018;3:
and management of psychosis of suspected 348–56.
autoimmune origin. Lancet Psychiatry 2020;7:93–108. 73. de Bruijn MAAM, van Sonderen A, van Coevorden-
59. McGinty RN, Handel A, Moloney T, Ramesh A, Fower A, Hameete MH, Bastiaansen AEM, Schreurs MWJ, Rouhl
Torzillo E, et al. Clinical features which predict neuronal RPW, et al. Evaluation of seizure treatment in anti-LGI1,
surface autoantibodies in new-onset focal epilepsy: anti-NMDAR, and anti-GABABR encephalitis. Neurology
implications for immunotherapies. J Neurol Neurosurg 2019;92:e2185–96.
Psychiatry 2021;92:291–4. 74. Broadley J, Seneviratne U, Beech P, Buzzard K,
60. Graus F, Escudero D, Oleaga L, Bruna J, Villarejo-Galende Butzkueven H, O’Brien T, et al. Prognosticating
A, Ballabriga J, et al. Syndrome and outcome of antibody- autoimmune encephalitis: a systematic review. J
negative limbic encephalitis. Eur J Neurol 2018;25: Autoimmun 2019;96:24–34.
1011–6. 75. Mun ~ iz-Castrillo S, Hedou JJ, Ambati A, Jones D, Vogrig A,
61. Hébert J, Day GS, Steriade C, Wennberg RA, Tang-Wai DF. Pinto A-L, et al. Distinctive clinical presentation and
Long-term cognitive outcomes in patients with pathogenic specificities of anti-AK5 encephalitis. Brain
autoimmune encephalitis. Can J Neurol Sci 2018;45: [Epub ahead of print] May 12, 2021as doi:
540–4. 10.1093/brain/awab153.
62. Balu R, McCracken L, Lancaster E, Graus F, Dalmau J, 76. Laurido-Soto O, Brier MR, Simon LE, McCullough A,
Titulaer MJ. A score that predicts 1-year functional status Bucelli RC, Day GS. Patient characteristics and outcome
in patients with anti-NMDA receptor encephalitis. associations in AMPA receptor encephalitis. J Neurol
Neurology 2018;92:e244–e252. 2018;266:450–60.
63. Dai Y, Zhang J, Ren H, Zhou X, Chen J, Cui L, et al. Surgical 77. van Coevorden-Hameete MH, de Bruijn MAAM, de Graaff
outcomes in patients with anti-N-methyl D-aspartate E, Bastiaansen DAEM, Schreurs MWJ, Demmers JAA, et al.
receptor encephalitis with ovarian teratoma. Am J Obstet The expanded clinical spectrum of anti-GABABR
Gynecol 2019;221:485.e1–485.e10. encephalitis and added value of KCTD16 autoantibodies.
64. Abboud H, Probasco JC, Irani S, Ances B, Benavides DR, Brain 2019;142:1631–43.
Bradshaw M, et al. Autoimmune encephalitis: proposed 78. Lancaster E, Martinez-Hernandez E, Titulaer MJ, Boulos
best practice recommendations for diagnosis and acute M, Weaver S, Antoine J-C, et al. Antibodies to
management. J Neurol Neurosurg Psychiatry 2021;92: metabotropic glutamate receptor 5 in the Ophelia
757–768 syndrome. Neurology 2011;77:1698–701.
65. Dubey D, Britton J, McKeon A, Gadoth A, Zekeridou A, 79. Zalewski NL, Lennon VA, Lachance DH, Klein CJ, Pittock SJ,
Lopez Chiriboga SA, et al. Randomized placebo- Mckeon A. P/Q- and N-type calcium-channel antibodies:
controlled trial of intravenous immunoglobulin in oncological, neurological, and serological
autoimmune LGI1/CASPR2 epilepsy. Ann Neurol 2020;87: accompaniments: neuronal calcium-channel Abs. Muscle
313–23. Nerve 2016;54:220–7.
66. Zhang Y, Huang H, Chen W, Liu G, Liu F, Su Y. Clinical 80. Pittock SJ, Lucchinetti CF, Parisi JE, Benarroch EE, Mokri B,
.................................................................................................
January 2022 | 07:01 | 81–98 | JALM 97You can also read