Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
AAOS-ADA Clinical Practice Guideline Summary
Prevention of Orthopaedic Implant
Infection in Patients Undergoing
Dental Procedures
Abstract
William Watters III, MD The Prevention of Orthopaedic Implant Infection in Patients Under-
Michael P. Rethman, DDS, MS going Dental Procedures evidence-based clinical practice guideline
Nicholas Buck Hanson, MPH was codeveloped by the American Academy of Orthopaedic Sur-
Elliot Abt, DDS geons (AAOS) and the American Dental Association. This guideline
Paul A. Anderson, MD
replaces the previous AAOS Information Statement, “Antibiotic Pro-
phylaxis in Bacteremia in Patients With Joint Replacement,” pub-
Karen C. Carroll, MD, FCAP
lished in 2009. Based on the best current evidence and a system-
Harry C. Futrell, DMD
atic review of published studies, three recommendations have been
Kevin Garvin, MD
created to guide clinical practice in the prevention of orthopaedic
Stephen O. Glenn, DDS implant infections in patients undergoing dental procedures. The
John Hellstein, DDS, MS first recommendation is graded as Limited; this recommendation
Angela Hewlett, MD, MS proposes that the practitioner consider changing the long-standing
David Kolessar, MD practice of routinely prescribing prophylactic antibiotic for patients
Calin Moucha, MD with orthopaedic implants who undergo dental procedures. The
Richard J. O’Donnell, MD second, graded as Inconclusive, addresses the use of oral topical
John E. O’Toole, MD antimicrobials in the prevention of periprosthetic joint infections.
Douglas R. Osmon, MD The third recommendation, a Consensus statement, addresses the
maintenance of good oral hygiene.
Richard Parker Evans, MD
Anthony Rinella, MD
Mark J. Steinberg, DDS, MD values when making treatment deci-
Michael Goldberg, MD Overview and Rationale sions.
Helen Ristic, PhD This clinical practice guideline was
This clinical practice guideline was developed using a rigorous, standard-
Kevin Boyer
approved by the American Academy ized process, beginning with a system-
Patrick Sluka, MPH of Orthopaedic Surgeons (AAOS) atic review of the available literature
William Robert Martin III, MD Board of Directors in December published from 1960 through July 2011
Deborah S. Cummins, PhD 2012 and by the American Dental related to the prevention of orthopae-
Sharon Song, PhD Association (ADA) Council on Scien- dic implant infection in patients under-
Anne Woznica, MLIS tific Affairs in November 2012. The going dental procedures. The system-
purpose of this clinical practice atic review demonstrates where there
Leeaht Gross, MPH
guideline is to help improve preven- is good evidence, where evidence is
tion and treatment based on the cur- lacking, and what topics future research
rent best evidence. could target to improve the prevention
J Am Acad Orthop Surg 2013;21:
180-189
The recommendations in this guide- of orthopaedic implant infection in pa-
line are not intended to be a fixed pro- tients undergoing dental procedures.
http://dx.doi.org/10.5435/
JAAOS-21-03-180
tocol; and as with all evidence-based The AAOS and ADA created this
recommendations, practitioners must guideline as an educational tool to
Copyright 2013 by the American
Academy of Orthopaedic Surgeons.
also rely on their clinical judgment as guide qualified physicians and den-
well as their patients’ preferences and tists through a series of treatment de-
180 Journal of the American Academy of Orthopaedic SurgeonsWilliam Watters III, MD, et al cisions in an effort to improve the needs and resources particular to the orthopaedic implant infection. Most quality and effectiveness of care. locality or institution. treatments are associated with some This guideline should not be con- known risks. In addition, contraindica- strued as including all proper meth- tions vary widely based on the treat- ods of care or as excluding methods Potential Harms, Benefits, ment administered. Therefore, discus- of care reasonably directed to ob- and Contraindications sion of available treatments applicable taining the same results. The ulti- to the individual patient relies on mu- mate judgment regarding any specific The goal of prevention of orthopaedic tual communication between the pa- procedure or treatment must be implant infection in patients undergo- tient, dentist, and physician, weighing made in light of all circumstances ing dental procedures is avoidance of the potential risks and benefits for that presented by the patient and the serious complications resulting from patient. From the American Academy of Orthopaedic Surgeons (AAOS), Rosemont, IL (Dr. Watters, Dr. Moucha, Dr. O’Donnell, Dr. Evans, and Dr. Goldberg), the American Dental Association, Chicago, IL (Dr. Rethman, Dr. Abt, Dr. Futrell, Dr. Glenn, and Dr. Hellstein), the AAOS, Rosemont, and the Congress of Neurological Surgeons, Schaumburg, IL (Dr. Anderson), the College of American Pathologists, Northfield, IL (Dr. Carroll), the Knee Society, Rosemont (Dr. Garvin), the Society for Healthcare Epidemiology of America, Arlington, VA (Dr. Hewlett), the American Association of Hip and Knee Surgeons, Rosemont (Dr. Kolessar), the American Association of Neurological Surgeons, Rolling Meadows, IL, and the Congress of Neurological Surgeons, Schaumburg (Dr. O’Toole), the Musculoskeletal Infection Society, Rochester, MN (Dr. Osmon), the Scoliosis Research Society, Milwaukee, WI (Dr. Rinella), the American Association of Oral and Maxillofacial Surgeons, Rosemont (Dr. Steinberg), the Division of Science and Professional Affairs, the American Dental Association, Chicago (Dr. Ristic and Mr. Hanson), and the Department of Research and Scientific Affairs, the AAOS (Dr. Martin, Dr. Cummins, Dr. Song, Mr. Sluka, Mr. Boyer, Ms. Woznica, and Ms. Gross). Dr. Watters or an immediate family member has received royalties from Stryker; has stock or stock options held in Intrinsic Orthopedics; and serves as a board member, owner, officer, or committee member of the American Board of Spine Surgery and the North American Spine Society (NASS). Dr. Rethman or an immediate family member serves as a paid consultant to Colgate- Palmolive; has stock or stock options held in Colgate-Palmolive and Pfizer; and serves as a board member, owner, officer, or committee member of the American Dental Association Foundation. Dr. Anderson or an immediate family member has received royalties from Pioneer and Stryker; serves as a paid consultant to Aesculap and Pioneer Surgical; serves as an unpaid consultant to Expanding Orthopedics, SI Bone, Spatatec, and Titan Surgical; has stock or stock options held in Pioneer Surgical, SI Bone, Spartec, and Titan Surgical; and serves as a board member, owner, officer, or committee member of the American Academy of Orthopaedic Surgeons (AAOS), American Society for Testing and Materials, NASS, Spine Arthroplasty Society, and the Spine Section of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Dr. Carroll or an immediate family member serves as a board member, owner, officer, or committee member of the American Society for Microbiology. Dr. Garvin or an immediate family member has received royalties from Biomet, and serves as a board member, owner, officer, or committee member of the AAOS, American Orthopaedic Association, and The Knee Society. Dr. Glenn or an immediate family member serves as a board member, owner, officer, or committee member of the American Dental Association and the Oklahoma Dental Association. Dr. Hellstein or an immediate family member serves as a board member, owner, officer, or committee member of the American Academy of Oral and Maxillofacial Pathology, American Board of Oral and Maxillofacial Pathology, and the Basal Cell Carcinoma Nevus Syndrome Life Support Network. Dr. Hewlett or an immediate family member serves as a board member, owner, officer, or committee member of the Society for Healthcare Epidemiology of America. Dr. Kolessar or an immediate family member has stock or stock options held in Zimmer. Dr. Moucha or an immediate family member is a member of a speakers’ bureau or has made paid presentations on behalf of 3M; has stock or stock options held in Auxillium; and serves as a board member, owner, officer, or committee member of the AAOS. Dr. O’Donnell or an immediate family member serves as a board member, owner, officer, or committee member of the Musculoskeletal Tumor Society, the National Comprehensive Cancer Network, the Northern California Chapter of the Western Orthopaedic Association, the Orthopaedic Surgical Osseointegration Society, and the Sarcoma Alliance. Dr. O’Toole or an immediate family member has received royalties from Globus Medical; serves as a paid consultant to Globus Medical and Pioneer Surgical; and serves as an unpaid consultant to Medtronic. Dr. Osmon or an immediate family member serves as a board member, owner, officer, or committee member of the Musculoskeletal Infection Society. Dr. Evans or an immediate family member is a member of a speakers’ bureau or has made paid presentations on behalf of Johnson & Johnson and Smith & Nephew. Dr. Steinberg or an immediate family member serves as a board member, owner, officer, or committee member of the American Association of Oral and Maxillofacial Surgeons. Dr. Goldberg or an immediate family member serves as a board member, owner, officer, or committee member of the AAOS. Dr. Martin or an immediate family member serves as a board member, owner, officer, or committee member of the National Board of Medical Examiners. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Rinella, Mr. Hanson, Dr. Abt, Dr. Futrell, Dr. Ristic, Mr. Boyer, Mr. Sluka, Dr. Cummins, Dr. Song, Ms. Woznica, and Ms. Gross. This clinical practice guideline was approved by the American Academy of Orthopaedic Surgeons on December 7, 2012. The complete evidence-based guideline, American Academy of Orthopaedic Surgeons and the American Dental Association Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures Clinical Practice Guideline, includes all tables, figures, and appendices, and is available at http://www.aaos.org/guidelines. March 2013, Vol 21, No 3 181
Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures
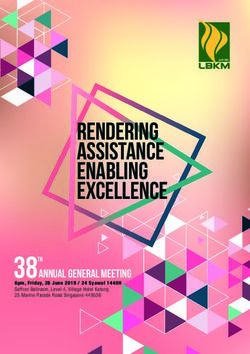
Figure 1 guage and grade of each
recommendation was directly influ-
enced by the best available evidence.
Economical and adverse outcomes
were not formally considered in cre-
ating these recommendations, per
AAOS policy. This guideline was cre-
ated with the best available evidence
as it relates to antibiotic prophylaxis,
dental procedures, and orthopaedic
implant infections.
Forty-seven outside organizations
were solicited to provide peer re-
viewers for this guideline. The draft
was sent to the 17 review organiza-
tions that responded to the solicita-
tion. The disposition of all non-
Overview of the evidence. Just one study (represented by the arching arrow) editorial peer review comments was
was identified in the literature search as providing direct evidence of
moderate strength and considered for the guideline. The results of this study
documented and accompanied this
show that dental procedures are not risk factors for subsequent implant guideline through the public com-
infection and furthermore that antibiotic prophylaxis does not reduce the risk mentary and the AAOS/ADA guide-
of subsequent infection. line approval process. The full guide-
line, along with all supporting
documentation and workgroup dis-
closures, is available on the AAOS
Background Methods Website, www.aaos.org/guidelines
In 2010, more than 302,000 hip re- The guideline was developed based
placements and 658,000 knee re- on a rigorous, standardized process
placements were performed in the commensurate with Institute of Med-
Results
United States. Based on the studies icine standards.15,16 The AAOS-ADA The best available evidence pub-
reviewed for this guideline, the mean work group held an introductory lished in studies that met the inclu-
rate of hip, knee, and spine implant meeting on November 20 and 21, sion criteria was considered for this
infections was 2%; management typ- 2010, to establish the scope of the guideline. The following is a sum-
ically requires further surgery and guideline and the search terms for mary of this evidence. As illustrated
prolonged antibiotic treatment.1-13 the systematic review. At the intro- in Figure 1, the quality of evidence
Causes included entry of microbes ductory meeting, the work group that explains the proposed associa-
into the wound during surgery, he- constructed preliminary recommen- tion between dental procedures and
matogenous spread, recurrence of dations which specified “[what] orthopaedic implant infection varies.
sepsis in a previously infected joint, should be done in [whom], [when], Only one study that provided direct
and contiguous spread of infection [where], and [how often or how evidence of moderate strength was
from a local source.14 long].” The preliminary recommen- identified by the literature search and
In light of the significant morbidity dations functioned as research ques- considered for this guideline. The re-
associated with orthopaedic implant in- tions for the systematic review, not sults of this study show that dental
fections, preventing such infections in as final recommendations or conclu- procedures are not risk factors for
patients undergoing dental procedures sions. Upon completing the system- subsequent implant infection and,
is highly desirable. However, prophy- atic review, the work group partici- furthermore, that antibiotic prophy-
lactic antibiotics also entail risks to in- pated in a 2-day recommendation laxis does not reduce the risk of sub-
dividual patients and, if widely used, are meeting on October 15 and 16, sequent infection.17
plausible contributors to the growing 2011, at which time the final recom- However, a multitude of indirect
problem of bacterial resistance result- mendations and rationales were ed- evidence was included in this guide-
ing from antibiotic overuse. ited, written, and voted on. The lan- line that investigates particular com-
182 Journal of the American Academy of Orthopaedic SurgeonsWilliam Watters III, MD, et al Figure 2 Incidence of bacteremia by procedure group. n = the number of studies pooled ponents of this complex mechanism. dian incidence of bacteremia, but We recognize the diversity of opin- Multiple high-strength studies link common daily habits such as flossing ion concerning the clinical impor- oral procedures to bacteremia, a sur- (ie, interdental cleaners), tooth tance of bacteremia as a surrogate rogate measure of risk for orthopae- brushing, and even chewing resulted outcome for orthopaedic implant in- dic implant infection. Some low- in bacteremia in some cases. fection, and understand the clini- strength studies investigate potential Instances of bacteremia following cian’s concern and rationale for risk factors for these bacteremias. In dental procedures may be modified wanting to prevent bacteremia. addition, multiple moderate-strength by individual risk factors. While the Therefore, we conducted two inde- studies suggest that prophylaxis de- strength of the evidence is low, sev- pendent network meta-analyses on creases the incidence of post–dental eral prognostic studies have ad- the efficacy of antibiotic and topical procedure bacteremia. But no studies dressed a multitude of patient char- antimicrobial prophylaxis for bacter- explain the microbiological relation- acteristics as potential risk factors emia post simple tooth extraction. ship between bacteremia and ortho- for developing bacteremia from den- Other studies exist that investigate paedic implant infection. tal procedures. These low-strength different dental procedures, but the Rates of bacteremia after dental studies report on oral health indica- most robust data reside in tooth ex- procedures varied significantly by tors and general patient characteris- traction studies. Several studies of and within dental procedure group. tics such as age and sex. The results, moderate strength were included in Median incidence rates range from which are often contradictory, vary these analyses. These studies investi- approximately 5% for chewing to across and within procedure groups gated the effect of many different an- upwards of 65% for simple tooth ex- (see the full guideline for tibiotic drugs and topical antimicro- traction and gingivectomy (Figure 2). details).18,25,26,28-30,33,34,40,52-59,65,75-79 No bials. Twenty-one antibiotic As expected, the more invasive oral conclusions about risk factors could studies22,31,53,57,60,80-95 and 13 topical procedures produced the highest me- be drawn from these studies. oral antimicrobial studies22,55,96-106 March 2013, Vol 21, No 3 183
Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures
Table 1 Table 2
Recommendations
Number Needed to Treat (NNT) to Number Needed to Treat (NNT) to
Prevent Bacteremia Post Tooth Prevent Bacteremia Post Tooth
Extraction: Antibioticsa Extraction: Topical Recommendation 1
Antimicrobialsa The practitioner might consider dis-
Treatment NNT
Treatment NNT continuing the practice of routinely
Amoxicillin 1.8 prescribing prophylactic antibiotics
Penicillin 2.5 Saline rinse 70.0
for patients with hip and knee pros-
Erythromycin 5.0 Chlorhexidine rinse 2.5
thetic joint implants undergoing den-
Clindamycin 3.0 Povidone-iodine rinse 2.3
tal procedures.
Josamycin 14.0 Chloramine-T rinse/brush 2.5
Grade of Recommendation: Lim-
Moxifloxacin 1.9 Lugol solution rinse 11.7
ited
Cefaclor 9.3 Hydrogen peroxide rinse 3.9
A Limited recommendation means
IV tetracycline 1.5 Sodium perborate–ascor- 2.5
bic acid rinse the quality of the supporting evi-
IV cefuroxime 2.1 dence that exists is unconvincing or
Phenolated rinse 2.8
IM teicoplanin 2.2 that well-conducted studies show lit-
Placebo rinse N/A
Topical amoxicillin 4.0 tle clear advantage to one approach
Operative field isolation 1.8
Antiseptic rinse 3.2
Isolation + iodine rinse 1.8 versus another.
IM penicillin or IV erythro- 3.7
Isolation + chlorhexidine 1.5 Practitioners should be cautious in
mycin or oral or IV
amoxicillin rinse deciding whether to follow a recom-
mendation classified as Limited and
N/A = not applicable
IM = intramuscular, IV = intravenous a should exercise judgment and be
a The table represents a conversion of
The table represents a conversion of
odds ratio from a forest plot of indirect
odds ratio from a forest plot of indirect alert to emerging publications that
(network) comparisons of topical antimi-
(network) comparisons of antibiotics ver-
crobials versus no treatment report evidence. Patient preference
sus placebo/no treatment
should have a substantial influencing
role.
were included in our network meta- orthopaedic implant infection case
analyses. The majority of the results series,17,107-122 approximately 64% of Recommendation 2
from the individual studies and the the infections were Staphylococcus We are unable to recommend for or
overall effect of these prophylactic species. Of the studies that distin- against the use of topical oral antimi-
agents according to our analyses guished early from late infections, crobials in patients with prosthetic
were favorable and clinically mean- 36.7% were early and 63.3% were joint implants or other orthopaedic
ingful (Tables 1 and 2). late.17,107-111,113-117,120 Dental-related implants undergoing dental proce-
While there was no direct evidence bacteremia varied greatly by proce- dures.
to explain the proposed association dure and study, as did the organism Grade of Recommendation: Incon-
between bacteremia and orthopaedic responsible for the bacteremia.19,22- clusive
implant infection, we summarized 24,28,29,33,35,37-42,44-48,50,51,62,64,65,67-73,89,91,93, An Inconclusive recommendation
the microbiological information per- 123-139No clear association between means that there is a lack of compel-
taining to cases and rates of bactere- the organisms found in the prosthetic ling evidence resulting in an unclear
mia and implant infection, when implant infections and bacteremia balance between benefits and poten-
available, based on our included lit- exists. However, the majority of the tial harm.
erature. According to orthopaedic organisms found in implant infec- Practitioners should feel little con-
implant cohort studies,1-13 approxi- tions are Staphylococcus, and the straint in deciding whether to follow
mately 53% of organisms responsi- majority of the organisms found as a recommendation labeled as Incon-
ble for the infections were Staphylo- the cause of bacteremias are Strepto- clusive and should exercise judgment
coccus species. The overall rate of coccus. and be alert to future publications
infection was approximately 1.5%. Considering all of the above infor- that clarify existing evidence for de-
Of the studies that distinguished mation in accordance with AAOS termining balance of benefits versus
early from late infections,1,4,5,8-11,13 we clinical practice guideline protocol, potential harm. Patient preference
were able to calculate rates of 0.4% the workgroup created the following should have a substantial influencing
and 0.9%, respectively. According to recommendations: role.
184 Journal of the American Academy of Orthopaedic SurgeonsWilliam Watters III, MD, et al
Recommendation 3 this one study of direct evidence was of (eg, implant infection).
In the absence of reliable evidence moderate strength, it did have limita- Recommendation 1 is limited to
linking poor oral health to prosthetic tions. The authors conducted covariate patients with hip and knee prosthe-
joint infection, it is the opinion of analysis on some subgroups of higher ses because the single study of direct
the work group that patients with risk patients. The number of patients in evidence included only patients with
prosthetic joint implants or other or- these subgroups, however, was rela- these types of orthopaedic implants.
thopaedic implants maintain appro- tively small, and there are insufficient There is no direct evidence that met
priate oral hygiene. data to suggest that these patients are our inclusion criteria for patients
at higher risk of experiencing hematog- with other types of orthopaedic im-
Grade of Recommendation: Con-
enous infections. plants.
sensus
Indirect evidence was also consid- Evidence for recommendation 2 is
A Consensus recommendation
ered for recommendation 1. There is sparse. There was no direct evidence
means that expert opinion supports
high-strength evidence that demon- to support or refute the use of pro-
the guideline recommendation even
strates the occurrence of bacteremia phylaxis (topical antimicrobials) be-
though there is no available empiri-
with dental procedures. Historically, fore dental procedures. The same in-
cal evidence that meets the inclusion
there has been a suggestion that bac- direct evidence discussed above
criteria.
teremias can cause hematogenous relating to dental procedures and
Practitioners should be flexible in de-
seeding of total joint implants, both bacteremia was considered for rec-
ciding whether to follow a recommen-
in the early postoperative period and ommendation 2. There is conflicting
dation classified as Consensus, al-
for many years following implanta- evidence regarding the effect of anti-
though they may set boundaries on
tion. Two years post joint arthro- microbial mouth rinse on the inci-
alternatives. Patient preference should
plasty was previously considered the dence of bacteremia post dental pro-
have a substantial influencing role.
critical period for prophylaxis. In ad- cedures. One high-strength study
dition, bacteremias may occur dur- reports no difference in the incidence
Discussion ing normal daily activities, such as of bacteremia following antimicro-
Direct support for recommendation 1 chewing and tooth brushing. It is bial mouth rinsing in patients under-
comes from a single well-conducted likely that these daily activities in- going dental extractions. Conversely,
case-control study. Study enrollment duce many more bacteremias than numerous studies suggest that topical
consisted of 339 patients with pros- do dental procedure–associated bac- antimicrobial prophylaxis decreases
thetic hip or knee infections (cases) and teremias. While evidence supports a the incidence of dental procedure–as-
339 patients with hip or knee arthro- strong association between certain sociated bacteremia. However, there
plasties without infection (controls) dental procedures and bacteremia, is no evidence that application of an-
hospitalized on an orthopaedic service there is no evidence to demonstrate a timicrobial mouth rinses before den-
during the same time period. The com- direct link between dental proce- tal procedures prevents infection of
parison between these groups was for dure–associated bacteremia and in- prosthetic joints or other orthopae-
differences in dental visits (exposure) in fection of prosthetic joints or other dic implants. Due to the lack of
terms of high- and low-risk dental pro- orthopaedic implants. Multiple stud- direct evidence, the contradictory na-
cedures, with and without antibiotic ies of moderate- and high-strength ture of the indirect evidence pertain-
prophylaxis. Results reported as odds evidence suggest that antibiotic pro- ing to topical oral antimicrobials,
ratios with 95% CI demonstrate no phylaxis decreases the risk of dental and continued concern with surro-
statistically significant differences be- procedure–associated bacteremias. gate outcomes, recommendation 2 is
tween groups. Neither dental proce- However, dental-procedure–associ- Inconclusive. The work group is un-
dures nor antibiotic prophylaxis before ated bacteremia is a surrogate out- able to recommend for or against the
dental procedures were associated with come for prosthetic joint infection. use of topical oral antimicrobials.
risk of prosthetic hip or knee infections. There is no evidence that these bacter- Recommendation 3 is an opinion
The authors performed a sample size emias are related to prosthetic joint statement due to the lack of evidence
calculation and withdrawals were low, infections. Surrogate outcomes may relating oral hygiene measures to
thus minimizing attrition bias. The pro- or may not relate to a clinically rele- prosthetic joint or other orthopaedic
spective nature of this study minimized vant patient outcome. A positive sur- implant infections. Oral hygiene
recall bias. Additionally, blinding of the rogate outcome (eg, reduced bactere- measures are low cost, provide po-
treatment group to those assessing out- mias), however, could mask a tential benefit, are consistent with
comes limits detection bias. Although negative patient-centered outcome current practice, and are in accor-
March 2013, Vol 21, No 3 185Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures
dance with good oral health. There is arthroplasty: A possible risk for late 21. Bender IB, Seltzer S, Tashman S, Meloff
infection. Am J Orthop (Belle Mead NJ) G: Dental procedures in patients with
evidence of the relationship of oral 1998;27(3):172-176. rheumatic heart disease. Oral Surg Oral
microflora to bacteremia. This bacte- Med Oral Pathol 1963;16:466-473.
8. Sancheti KH, Laud NS, Bhende H,
remia may be associated with poor Reddy G, Pramod N, Mani JN: The 22. Casolari C, Neglia R, Forabosco A,
oral hygiene. This implies that im- INDUS knee prosthesis: Prospective Galetti R, Fabio U: Incidence of oral
multicentric trial of a posteriorly bacteremia and antimicrobial
provement of oral hygiene (or main- prophylaxis. J Chemother 1989;1(4
stabilized high-flex design: 2 years
tenance of good oral hygiene) may follow-up. Indian J Orthop 2009;43(4): suppl):968-971.
be beneficial in reducing bacteremia. 367-374. 23. Heimdahl A, Hall G, Hedberg M, et al:
Detection and quantitation by lysis-
These recommendations are not in- 9. Smith JA, Dunn HK, Manaster BJ:
Cementless femoral revision arthroplasty. filtration of bacteremia after different
tended to stand alone. Treatment de- 2- to 5-year results with a modular oral surgical procedures. J Clin
cisions should be made in light of all titanium alloy stem. J Arthroplasty 1997; Microbiol 1990;28(10):2205-2209.
12(2):194-201. 24. Khairat O: The non-aerobes of post-
circumstances presented by the pa-
10. Soultanis K, Mantelos G, Pagiatakis A, extraction bacteremia. J Dent Res 1966;
tient. Treatments and procedures ap- 45(4):1191-1197.
Soucacos PN: Late infection in patients
plicable to the individual patient rely with scoliosis treated with spinal 25. Enabulele OI, Aluyi HS, Omokao O:
on mutual communication between instrumentation. Clin Orthop Relat Res Incidence of bacteraemia following teeth
2003;411:116-123. extraction at the dental clinic of the
patient, physician, dentist, and other
11. Uçkay I, Lübbeke A, Emonet S, et al: University of Benin Teaching Hospital,
healthcare practitioners in accor- Benin city, Nigeria. Afr J Biotechnol
Low incidence of haematogenous seeding
dance with evidence-based medicine to total hip and knee prostheses in 2008;7(10):1390-1393.
applicability. (See the full guideline patients with remote infections. J Infect 26. Takai S, Kuriyama T, Yanagisawa M,
2009;59(5):337-345. Nakagawa K, Karasawa T: Incidence
at http://www.aaos.org/research/
12. Wagner M, Wagner H: Medium-term and bacteriology of bacteremia
guidelines/PUDP/dental_guideline.asp) associated with various oral and
results of a modern metal-on-metal
system in total hip replacement. Clin maxillofacial surgical procedures. Oral
Orthop Relat Res 2000;379:123-133. Surg Oral Med Oral Pathol Oral Radiol
Endod 2005;99(3):292-298.
References 13. Wimmer C, Nogler M, Frischhut B:
Influence of antibiotics on infection in 27. Josefsson K, Heimdahl A, von Konow L,
spinal surgery: A prospective study of Nord CE: Effect of phenoxymethylpeni-
1. Ainscow DA, Denham RA: The risk of 110 patients. J Spinal Disord 1998; cillin and erythromycin prophylaxis on
haematogenous infection in total joint 11(6):498-500. anaerobic bacteraemia after oral surgery.
replacements. J Bone Joint Surg Br 1984; J Antimicrob Chemother 1985;16(2):
66(4):580-582. 14. Della Valle CJ, Zuckerman JD, Di 243-251.
Cesare PE: Periprosthetic sepsis. Clin
2. Choong PF, Dowsey MM, Carr D, Daffy Orthop Relat Res 2004;420:26-31. 28. Cherry M, Daly CG, Mitchell D,
J, Stanley P: Risk factors associated with Highfield J: Effect of rinsing with
acute hip prosthetic joint infections and 15. Institute of Medicine: Clinical Practice povidone-iodine on bacteraemia due to
outcome of treatment with a rifampin- Guidelines We Can Trust. Washington, scaling: A randomized-controlled trial.
based regimen. Acta Orthop 2007;78(6): DC, National Academies Press, 2011. J Clin Periodontol 2007;34(2):148-155.
755-765.
16. Institute of Medicine: Finding What 29. Forner L, Larsen T, Kilian M,
3. Goodman SB, Oh KJ, Imrie S, Hwang K, Works in Health Care: Standards for Holmstrup P: Incidence of bacteremia
Shegog M: Revision total hip Systematice Reviews. Washington, DC, after chewing, tooth brushing and
arthroplasty in juvenile chronic arthritis: National Academies Press, 2011. scaling in individuals with periodontal
17 revisions in 11 patients followed for inflammation. J Clin Periodontol 2006;
4-12 years. Acta Orthop 2006;77(2): 17. Berbari EF, Osmon DR, Carr A, et al: 33(6):401-407.
242-250. Dental procedures as risk factors for
prosthetic hip or knee infection: A 30. De Leo AA, Schoenknecht FD, Anderson
4. Hamilton H, Jamieson J: Deep infection hospital-based prospective case-control MW, Peterson JC: The incidence of
in total hip arthroplasty. Can J Surg study. Clin Infect Dis 2010;50(1):8-16. bacteremia following oral prophylaxis
2008;51(2):111-117. on pediatric patients. Oral Surg Oral
18. Lineberger LT, De Marco TJ: Evaluation Med Oral Pathol 1974;37(1):36-45.
5. Klenerman L, Seal D, Sullens K: of transient bacteremia following routine
Combined prophylactic effect of periodontal procedures. J Periodontol 31. Hall G, Hedström SA, Heimdahl A,
ultraclean air and cefuroxime for 1973;44(12):757-762. Nord CE: Prophylactic administration of
reducing infection in prosthetic surgery. penicillins for endocarditis does not
Acta Orthop Belg 1991;57(1):19-24. 19. Rogosa M, Hampp EG, Nevin TA, reduce the incidence of postextraction
Wagner HN Jr, Driscoll EJ, Baer PN: bacteremia. Clin Infect Dis 1993;17(2):
6. Mont MA, Yoon TR, Krackow KA, Blood sampling and cultural studies in 188-194.
Hungerford DS: Clinical experience with the detection of postoperative
a proximally porous-coated second- bacteremias. J Am Dent Assoc 1960;60: 32. Forner L, Nielsen CH, Bendtzen K,
generation cementless total hip 171-180. Larsen T, Holmstrup P: Increased
prosthesis: Minimum 5-year follow-up. plasma levels of IL-6 in bacteremic
J Arthroplasty 1999;14(8):930-939. 20. Wada K, Tomizawa M, Sasaki I: Study periodontis patients after scaling. J Clin
on bacteriemia in patients with pyorrhea Periodontol 2006;33(10):724-729.
7. Petrie RS, Hanssen AD, Osmon DR, alveolaris caused by surgical operations.
Ilstrup D: Metal-backed patellar J Nihon Univ Sch Dent 1968;10(2):52- 33. Daly CG, Mitchell DH, Highfield JE,
component failure in total knee 57. Grossberg DE, Stewart D: Bacteremia
186 Journal of the American Academy of Orthopaedic SurgeonsWilliam Watters III, MD, et al
due to periodontal probing: A clinical 47. Gürel HG, Basciftci FA, Arslan U: 60. Lockhart PB, Brennan MT, Sasser HC,
and microbiological investigation. Transient bacteremia after removal of a Fox PC, Paster BJ, Bahrani-Mougeot FK:
J Periodontol 2001;72(2):210-214. bonded maxillary expansion appliance. Bacteremia associated with
Am J Orthod Dentofacial Orthop 2009; toothbrushing and dental extraction.
34. Daly C, Mitchell D, Grossberg D, 135(2):190-193. Circulation 2008;117(24):3118-3125.
Highfield J, Stewart D: Bacteraemia
caused by periodontal probing. Aust 48. Erverdi N, Kadir T, Ozkan H, Acar A: 61. Sconyers JR, Albers DD, Kelly R:
Dent J 1997;42(2):77-80. Investigation of bacteremia after Relationship of bacteremia to
orthodontic banding. Am J Orthod toothbrushing in clinically healthy
35. Morozumi T, Kubota T, Abe D, Shimizu Dentofacial Orthop 1999;116(6):687- patients. Gen Dent 1979;27(3):51-52.
T, Komatsu Y, Yoshie H: Effects of 690.
irrigation with an antiseptic and oral 62. Sconyers JR, Crawford JJ, Moriarty JD:
administration of azithromycin on 49. Savarrio L, Mackenzie D, Riggio M,
Relationship of bacteremia to
bacteremia caused by scaling and root Saunders WP, Bagg J: Detection of
toothbrushing in patients with
planing. J Periodontol 2010;81(11): bacteraemias during non-surgicalroot
periodontitis. J Am Dent Assoc 1973;
1555-1563. canal treatment. J Dent 2005;33(4):293-
303. 87(3):616-622.
36. Lofthus JE, Waki MY, Jolkovsky DL,
et al: Bacteremia following subgingival 50. Baumgartner JC, Heggers JP, Harrison 63. Nixon PP, Littler P, Davies K, Krishnam
irrigation and scaling and root planing. JW: The incidence of bacteremias related MS: Does sialography require antibiotic
J Periodontol 1991;62(10):602-607. to endodontic procedures: I. Nonsurgical prophylaxis? Br J Radiol 2009;82(981):
endodontics. J Endod 1976;2(5):135- 732-734.
37. Waki MY, Jolkovsky DL, Otomo-Corgel
140.
J, et al: Effects of subgingival irrigation 64. Lamey PJ, Macfarlane TW, Patton DW,
on bacteremia following scaling and root 51. Baumgartner JC, Heggers JP, Harrison Samaranayake LP, Ferguson MM:
planing. J Periodontol 1990;61(7):405- JW: Incidence of bacteremias related to Bacteraemia consequential to sialog-
411. endodontic procedures: II. Surgical raphy. Br Dent J 1985;158(6):218-220.
endodontics. J Endod 1977;3(10):399-
38. Lafaurie GI, Mayorga-Fayad I, Torres 65. Valdés C, Tomás I, Alvarez M, Limeres J,
402.
MF, et al: Periodontopathic Medina J, Diz P: The incidence of
microorganisms in peripheric blood after 52. Bhanji S, Williams B, Sheller B, Elwood bacteraemia associated with tracheal
scaling and root planing. J Clin T, Mancl L: Transient bacteremia intubation. Anaesthesia 2008;63(6):588-
Periodontol 2007;34(10):873-879. induced by toothbrushing a comparison 592.
39. Lucartorto FM, Franker CK, Maza J: of the Sonicare toothbrush with a
Postscaling bacteremia in HIV-associated conventional toothbrush. Pediatr Dent 66. Ali MT, Tremewen DR, Hay AJ,
gingivitis and periodontitis. Oral Surg 2002;24(4):295-299. Wilkinson DJ: The occurrence of
Oral Med Oral Pathol 1992;73(5):550- bacteraemia associated with the use of
53. Wahlmann U, Al-Nawas B, Jütte M, oral and nasopharyngeal airways.
554. Wagner W: Clinical and microbiological Anaesthesia 1992;47(2):153-155.
40. Crasta K, Daly CG, Mitchell D, Curtis B, efficacy of single dose cefuroxime
Stewart D, Heitz-Mayfield LJ: prophylaxis for dental surgical 67. Dinner M, Tjeuw M, Artusio JF Jr:
Bacteraemia due to dental flossing. J Clin procedures. Int J Antimicrob Agents Bacteremia as a complication of
Periodontol 2009;36(4):323-332. 1999;12(3):253-256. nasotracheal intubation. Anesth Analg
1987;66(5):460-462.
41. Ramadan AE, Zaki SA, Nour ZM: A 54. Roberts GJ, Watts R, Longhurst P,
study of transient bacteremia following Gardner P: Bacteremia of dental origin 68. Berry FA Jr, Blankenbaker WL, Ball CG:
the use of dental floss silk and and antimicrobial sensitivity following Comparison of bacteremia occurring
interdental stimulators. Egypt Dent J oral surgical procedures in children. with nasotracheal and orotracheal
1975;21(4):19-28. Pediatr Dent 1998;20(1):28-36. intubation. Anesth Analg 1973;52(6):
873-876.
42. Berger SA, Weitzman S, Edberg SC, 55. Lockhart PB: An analysis of bacteremias
Casey JI: Bacteremia after the use of an during dental extractions: A double- 69. Onçağ O, Cökmez B, Aydemir S,
oral irrigation device: A controlled study blind, placebo-controlled study of Balcioğlu T: Investigation of bacteremia
in subjects with normal-appearing chlorhexidine. Arch Intern Med 1996; following nasotracheal intubation.
gingiva. Comparison with use of 156(5):513-520. Paediatr Anaesth 2005;15(3):194-198.
toothbrush. Ann Intern Med 1974;80(4):
510-511. 56. Okabe K, Nakagawa K, Yamamoto E: 70. Hansen CP, Westh H, Brok KE, Jensen
Factors affecting the occurrence of R, Bertelsen S: Bacteraemia following
43. Oral irrigation and bacteremia. J N C bacteremia associated with tooth orotracheal intubation and oesophageal
Dent Soc 1972;55(2):23-24. extraction. Int J Oral Maxillofac Surg balloon dilatation. Thorax 1989;44(8):
1995;24(3):239-242. 684-685.
44. Romans AR, App GR: Bacteremia, a
result from oral irrigation in subjects 57. Coulter WA, Coffey A, Saunders ID, 71. King RC, Crawford JJ, Small EW:
with gingivitis. J Periodontol 1971; Emmerson AM: Bacteremia in children Bacteremia following intraoral suture
42(12):757-760. following dental extraction. J Dent Res removal. Oral Surg Oral Med Oral
1990;69(10):1691-1695. Pathol 1988;65(1):23-28.
45. Felix JE, Rosen S, App GR: Detection of
bacteremia after the use of an oral 58. Trivedi DN: Bacteraemia due to 72. Wampole HS, Allen AL, Gross A: The
irrigation device in subjects with operative procedure. J Indian Dent incidence of transient bacteremia during
periodontitis. J Periodontol 1971;42(12): Assoc 1984;56(12):447-452. periodontal dressing change.
785-787. J Periodontol 1978;49(9):462-464.
59. Silver JG, Martin AW, McBride BC:
46. Wank HA, Levison ME, Rose LF, Cohen Experimental transient bacteraemias in 73. Brown AR, Papasian CJ, Shultz P,
DW: A quantitative measurement of human subjects with varying degrees of Theisen FC, Shultz RE: Bacteremia and
bacteremia and its relationship to plaque plaque accumulation and gingival intraoral suture removal: Can an
control. J Periodontol 1976;47(12):683- inflammation. J Clin Periodontol 1977; antimicrobial rinse help? J Am Dent
686. 4(2):92-99. Assoc 1998;129(10):1455-1461.
March 2013, Vol 21, No 3 187Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures
74. Murphy AM, Daly CG, Mitchell DH, 86. Head TW, Bentley KC, Millar EP, povidone-iodine and chlorhexidine. J Am
Stewart D, Curtis BH: Chewing fails to deVries JA: A comparative study of the Dent Assoc 1995;126(8):1145-1149.
induce oral bacteraemia in patients with effectiveness of metronidazole and
periodontal disease. J Clin Periodontol penicillin V in eliminating anaerobes 99. Scopp IW, Orvieto LD: Gingival
2006;33(10):730-736. from postextraction bacteremias. Oral degerming by povidone-iodine irrigation:
Surg Oral Med Oral Pathol 1984;58(2): Bacteremia reduction in extraction
75. Barbosa M, Carmona IT, Amaral B, 152-155. procedures. J Am Dent Assoc 1971;
et al: General anesthesia increases the 83(6):1294-1296.
risk of bacteremia following dental 87. Jokinen MA: Bacteremia following
extractions. Oral Surg Oral Med Oral dental extraction and its prophylaxis. 100. Sweet JB, Gill VJ, Chusid MJ, Elin RJ:
Pathol Oral Radiol Endod 2010;110(6): Suom Hammaslaak Toim 1970;66(3):69- Nitroblue tetrazolium and Limulus
100. assays for bacteremia after dental
706-712.
extraction: Effect of topical antiseptics.
88. Khairat O: An effective antibiotic cover J Am Dent Assoc 1978;96(2):276-281.
76. Ashare A, Stanford C, Hancock P, et al:
for the prevention of endocarditis
Chronic liver disease impairs bacterial
following dental and other post- 101. Tomás I, Alvarez M, Limeres J, et al:
clearance in a human model of induced operative bacteraemias. J Clin Pathol Effect of a chlorhexidine mouthwash on
bacteremia. Clin Transl Sci 2009;2(3): 1966;19(6):561-566. the risk of postextraction bacteremia.
199-205. Infect Control Hosp Epidemiol 2007;
89. Maskell JP, Carter JL, Boyd RB, 28(5):577-582.
77. Lockhart PB, Brennan MT, Thornhill M, Williams RJ: Teicoplanin as a
et al: Poor oral hygiene as a risk factor prophylactic antibiotic for dental 102. Cutcher JL, Goldberg JR, Lilly GE, Jones
for infective endocarditis-related bacteraemia. J Antimicrob Chemother JC: Control of bacteremia associated
bacteremia. J Am Dent Assoc 2009; 1986;17(5):651-659. with extraction of teeth: II. Oral Surg
140(10):1238-1244. Oral Med Oral Pathol 1971;31(5):602-
90. Roberts GJ, Radford P, Holt R: 605.
78. Tomás I, Pereira F, Llucián R, Poveda R, Prophylaxis of dental bacteraemia with
Diz P, Bagán JV: Prevalence of oral amoxycillin in children. Br Dent J 103. Francis LE, DeVries J, Lang D: An oral
bacteraemia following third molar 1987;162(5):179-182. antiseptic for the control of post-
surgery. Oral Dis 2008;14(1):89-94. extraction bacteraemia. J Can Dent
91. Shanson DC, Shehata A, Tadayon M, Assoc (Tor) 1973;39(1):55-57.
79. Brennan MT, Kent ML, Fox PC, Norton Harris M: Comparison of intravenous
HJ, Lockhart PB: The impact of oral teicoplanin with intramuscular 104. Jones JC, Cutcher JL, Goldberg JR, Lilly
disease and nonsurgical treatment on amoxycillin for the prophylaxis of GE: Control of bacteremia associated
bacteremia in children. J Am Dent Assoc streptococcal bacteraemia in dental with extraction of teeth. Oral Surg Oral
2007;138(1):80-85. patients. J Antimicrob Chemother 1987; Med Oral Pathol 1970;30(4):454-459.
80. Lockhart PB, Brennan MT, Kent ML, 20(1):85-93.
105. Nasif AS: The incidence of post-
Norton HJ, Weinrib DA: Impact of 92. Shanson DC, Akash S, Harris M, extraction bacteremia after irrigation of
amoxicillin prophylaxis on the incidence, Tadayon M: Erythromycin stearate, the gingival sulcus with hydrogen
nature, and duration of bacteremia in 1.5 g, for the oral prophylaxis of peroxide solution. Egypt Dent J 1977;
children after intubation and dental streptococcal bacteraemia in patients 23(3):51-55.
procedures. Circulation 2004;109(23): undergoing dental extraction: Efficacy
2878-2884. and tolerance. J Antimicrob Chemother 106. Yamalik MK, Yücetas S, Abbasoğlu U:
1985;15(1):83-90. Effects of various antiseptics on
81. Aitken C, Cannell H, Sefton AM, et al: bacteremia following tooth extraction.
Comparative efficacy of oral doses of 93. Shanson DC, Cannon P, Wilks M: J Nihon Univ Sch Dent 1992;34(1):28-
clindamycin and erythromycin in the Amoxycillin compared with penicillin V 33.
prevention of bacteraemia. Br Dent J for the prophylaxis of dental
1995;178(11):418-422. bacteraemia. J Antimicrob Chemother 107. Chiu FY, Chen CM: Surgical
1978;4(5):431-436. débridement and parenteral antibiotics in
82. Cannell H, Kerawala C, Sefton AM, infected revision total knee arthroplasty.
et al: Failure of two macrolide antibiotics 94. Vergis EN, Demas PN, Vaccarello SJ, Yu Clin Orthop Relat Res 2007;461:130-
to prevent post-extraction bacteraemia. VL: Topical antibiotic prophylaxis for 135.
Br Dent J 1991;171(6):170-173. bacteremia after dental extractions. Oral
Surg Oral Med Oral Pathol Oral Radiol 108. Cordero-Ampuero J, Esteban J, García-
83. Diz Dios P, Tomás Carmona I, Limeres Cimbrelo E: Oral antibiotics are effective
Posse J, Medina Henríquez J, Fernández Endod 2001;91(2):162-165.
for highly resistant hip arthroplasty
Feijoo J, Alvarez Fernández M: 95. deVries J, Francis LE, Lang D: Control infections. Clin Orthop Relat Res 2009;
Comparative efficacies of amoxicillin, of post-extraction bacteraemias in the 467(9):2335-2342.
clindamycin, and moxifloxacin in penicillin-hypersensitive patient. J Can
prevention of bacteremia following Dent Assoc (Tor) 1972;38(2):63-66. 109. Cordero-Ampuero J, Esteban J, García-
dental extractions. Antimicrob Agents Cimbrelo E, Munuera L, Escobar R:
Chemother 2006;50(9):2996-3002. 96. Jokinen MA: Prevention of Low relapse with oral antibiotics and
postextraction bacteremia by local two-stage exchange for late arthroplasty
84. Hall G, Heimdahl A, Nord CE: Effects prophylaxis. Int J Oral Surg 1978;7(5): infections in 40 patients after 2-9 years.
of prophylactic administration of 450-452. Acta Orthop 2007;78(4):511-519.
cefaclor on transient bacteremia after
dental extraction. Eur J Clin Microbiol 97. Macfarlane TW, Ferguson MM, 110. Crockarell JR, Hanssen AD, Osmon DR,
Infect Dis 1996;15(8):646-649. Mulgrew CJ: Post-extraction Morrey BF: Treatment of infection with
bacteraemia: Role of antiseptics and débridement and retention of the
85. Hall G, Nord CE, Heimdahl A: antibiotics. Br Dent J 1984;156(5):179- components following hip arthroplasty.
Elimination of bacteraemia after dental 181. J Bone Joint Surg Am 1998;80(9):1306-
extraction: Comparison of erythromycin 1313.
and clindamycin for prophylaxis of 98. Rahn R, Schneider S, Diehl O, Schäfer V,
infective endocarditis. J Antimicrob Shah PM: Preventing post-treatment 111. Fink B, Makowiak C, Fuerst M, Berger I,
Chemother 1996;37(4):783-795. bacteremia: Comparing topical Schäfer P, Frommelt L: The value of
188 Journal of the American Academy of Orthopaedic SurgeonsWilliam Watters III, MD, et al
synovial biopsy, joint aspiration and 120. Waldman BJ, Hostin E, Mont MA, Bacteraemia following incision and
C-reactive protein in the diagnosis of late Hungerford DS: Infected total knee drainage of dento-alveolar abscesses. Br
peri-prosthetic infection of total knee arthroplasty treated by arthroscopic Dent J 1990;169(2):51-53.
replacements. J Bone Joint Surg Br 2008; irrigation and débridement.
90(7):874-878. J Arthroplasty 2000;15(4):430-436. 131. Martin WJ, Schirger A: Prevention of
bacteremia after oral surgery. Minn Med
112. Hoad-Reddick DA, Evans CR, Norman 121. Windsor RE, Insall JN, Urs WK, Miller 1964;47:1519-1523.
P, Stockley I: Is there a role for extended DV, Brause BD: Two-stage
antibiotic therapy in a two-stage revision reimplantation for the salvage of total 132. Burden DJ, Coulter WA, Johnston CD,
of the infected knee arthroplasty? J Bone knee arthroplasty complicated by Mullally B, Stevenson M: The prevalence
Joint Surg Br 2005;87(2):171-174. infection: Further follow-up and of bacteraemia on removal of fixed
refinement of indications. J Bone Joint orthodontic appliances. Eur J Orthod
113. Insall JN, Thompson FM, Brause BD: Surg Am 1990;72(2):272-278. 2004;26(4):443-447.
Two-stage reimplantation for the salvage
of infected total knee arthroplasty. 122. Wroblewski BM: One-stage revision of 133. Conner HD, Haberman S, Collings CK,
J Bone Joint Surg Am 1983;65(8):1087- infected cemented total hip arthroplasty. Winford TE: Bacteremias following
1098. Clin Orthop Relat Res 1986;211:103- periodontal scaling in patients with
107.
healthy appearing gingiva. J Periodontol
114. Jerosch J, Schneppenheim M:
123. Lucas V, Roberts GJ: Odontogenic 1967;38(6):466-472.
Management of infected shoulder
replacement. Arch Orthop Trauma Surg bacteremia following tooth cleaning
134. Gutverg M: Studies on bacteremia
2003;123(5):209-214. procedures in children. Pediatr Dent
2000;22(2):96-100. following oral surgery: Some
115. Mont MA, Waldman B, Banerjee C, prophylactic approaches to bacteremia
Pacheco IH, Hungerford DS: Multiple 124. Silver JG, Martin AW, McBride BC: and the results of tissue examination of
irrigation, debridement, and retention of Experimental transient bacteraemias in excised gingiva. J Periodontol 1962;33:
components in infected total knee human subjects with clinically healthy 105.
arthroplasty. J Arthroplasty 1997;12(4): gingivae. J Clin Periodontol 1979;6(1):
33-36. 135. Kinane DF, Riggio MP, Walker KF,
426-433.
MacKenzie D, Shearer B: Bacteraemia
116. Muñoz-Mahamud E, García S, Bori G, 125. Marzoni FA, Kelly DR: Bacteremia following periodontal procedures. J Clin
et al: Comparison of a low-pressure and following cleft palate repair: A Periodontol 2005;32(7):708-713.
a high-pressure pulsatile lavage during prospective study. Ann Plast Surg 1983;
débridement for orthopaedic implant 10(6):473-474. 136. Giglio JA, Rowland RW, Dalton HP,
infection. Arch Orthop Trauma Surg Laskin DM: Suture removal-induced
126. Piñeiro A, Tomás I, Blanco J, Alvarez M,
2011;131(9):1233-1238. bacteremia: A possible endocarditis risk.
Seoane J, Diz P: Bacteraemia following
dental implants’ placement. Clin Oral J Am Dent Assoc 1992;123(8):65-66,
117. Rao N, Crossett LS, Sinha RK, Le Frock 69-70.
JL: Long-term suppression of infection in Implants Res 2010;21(9):913-918.
total joint arthroplasty. Clin Orthop 127. Winslow MB, Kobernick SD: Bacteremia 137. Soliman NA, el-Batawy YA, Abdallah
Relat Res 2003;414:55-60. after prophylaxis. J Am Dent Assoc AK: Bacteriologic study of the systemic
1960;61:69-72. disturbances accompanying primary
118. Rodríguez D, Pigrau C, Euba G, et al; teething. Egypt Dent J 1977;23(2):111-
REIPI Group (Spanish Network for 128. Debelian GJ, Olsen I, Tronstad L: 113.
Research in Infectious Disease): Acute Bacteremia in conjunction with
haematogenous prosthetic joint endodontic therapy. Endod Dent 138. Crawford JJ, Sconyers JR, Moriarty JD,
infection: Prospective evaluation of Traumatol 1995;11(3):142-149. King RC, West JF: Bacteremia after
medical and surgical management. Clin tooth extractions studied with the aid of
Microbiol Infect 2010;16(12):1789- 129. Rahn R, et al: The effect of topical prereduced anaerobically sterilized
1795. Povidone-Iodine and Chlorhexidine on culture media. Appl Microbiol 1974;
the incidence of bacteremia following 27(5):927-932.
119. Soriano A, Gómez J, Gómez L, et al: dental treatment procedures. Hygiene +
Efficacy and tolerability of prolonged Medizin 1994;19(3):128-131. 139. Peterson LJ, Peacock R: The incidence of
linezolid therapy in the treatment of bacteremia in pediatric patients
orthopedic implant infections. Eur J Clin 130. Flood TR, Samaranayake LP, following tooth extraction. Circulation
Microbiol Infect Dis 2007;26(5):353- MacFarlane TW, McLennan A, 1976;53(4):676-679.
356. MacKenzie D, Carmichael F:
March 2013, Vol 21, No 3 189You can also read