Group B Streptococcus Colonization in Late Pregnancy and Invasive Infection in Neonates in China: A Population-Based 3-Year Study
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Original Paper
Neonatology 2019;115:301–309 Received: May 21, 2018
Accepted after revision: October 1, 2018
DOI: 10.1159/000494133 Published online: February 25, 2019
Group B Streptococcus Colonization in Late
Pregnancy and Invasive Infection in Neonates in
China: A Population-Based 3-Year Study
Yao Zhu a Jing Huang a Xin-Zhu Lin a Chao Chen b
a Department of Neonatology, Maternal and Child Care Hospital of Xiamen, Xiamen, China; b Department of
Neonatology, Children’s Hospital of Fudan University, Shanghai, China
Keywords Logistic regression analysis indicated that gestational bacte-
Group B Streptococcus · Late pregnancy · Neonate · Group riuria, GBS disease in infants from previous pregnancies, and
B Streptococcus early-onset disease chorioamnionitis were risk factors for GBS-EOD (p = 0.007,
p = 0.000, and p = 0.018, respectively). IAP effectively pro-
tected against neonatal GBS-EOD (p = 0.011). Conclusions:
Abstract GBS colonization was detected in nearly 14% of late preg-
Background: As no population-based studies of group B nant women. The IAP for reducing GBS-EOD was effective.
Streptococcus (GBS) colonization rates in late pregnancy (at Therefore, universal screening of maternal GBS and subse-
35–37 weeks of gestation) have been conducted in China, quent IAP for those with GBS colonization should be imple-
the incidence of and risk factors for neonatal early-onset GBS mented in China. © 2019 S. Karger AG, Basel
disease (GBS-EOD) in China remains poorly understood. Ob-
jectives: To determine the GBS colonization rate in late preg-
nancy and neonatal GBS infection in Xiamen, China, and to
assess the effectiveness of intrapartum antibiotic prophylax- Introduction
is (IAP) for the prevention of neonatal GBS-EOD. Methods: A
total of 49,908 pregnant women were enrolled between Group B Streptococcus (GBS) has been reported to
April 1, 2014 and March 31, 2017. Bacterial culture was used constitute part of the vaginal flora of 10–30% of preg-
to diagnose GBS infection in both pregnant women and ne- nant women [1]. GBS colonization of the vagina is usu-
onates. Women with GBS colonization received IAP during ally asymptomatic. However, GBS infection can cause
parturition or rupture of fetal membranes. Results: The GBS asymptomatic bacteremia and urinary tract infections,
colonization rate was 13.89% (6,933/49,908); 50,772 neo- such as pyelonephritis, in pregnant women [1, 2]. GBS
nates were born to 49,908 pregnant women, of whom 75 has been implicated as a cause of human postpartum sep-
(1.48 per 1,000) were diagnosed with GBS-EOD. The inci-
dence of GBS-EOD among neonates born to GBS-positive
mothers (8.77‰; 62/7,068) was 29 times higher than that of Xin-Zhu Lin
Department of Neonatology, Maternal and Child Care Hospital of Xiamen
neonates born to GBS-negative mothers (0.30‰; 13/43,704). No.10, Zhenhai Road, Siming District
Xiamen 361003 (China)
E-Mail xinzhufj @ 163.com
46.4.80.155 - 12/15/2020 8:43:51 AM
© 2019 S. Karger AG, Basel Chao Chen
Department of Neonatology, Children’s Hospital of Fudan University
Iceland Consortium - Nova
No. 399, Wanyuan Road, Minhang District
E-Mail karger@karger.com
Shanghai (China)
www.karger.com/neo
Downloaded by:
E-Mail chen6010 @ 163.comTotal (n = 51,734)
Excluded (n = 322)
Fetal malformation (n = 61)
Habitual abortion (n = 74)
Use of antibiotics (n = 1)
Eligible (n = 51,412)
No GBS screening (n = 1,504)
Antenatal examination in
another hospital (n = 685)
Refused consent (n = 337)
Omission of screening (n = 482)
GBS screening (n = 49,908)
GBS-positive group GBS-negative group
(n = 6,933) (n = 42,975)
Fig. 1. Subject enrollment and selection GBS-EOD (n = 62) GBS-EOD (n = 13)
flow chart.
sis as GBS present in the vagina can be transmitted to Methods
neonates during delivery [1, 3]. Roughly 2% of neonates
Subject Populations
infected with GBS develop invasive infection leading to Inclusion Criteria. Pregnant women at 35–37 weeks of gesta-
sepsis, pneumonia, and less commonly meningitis [2]. tion or with preterm delivery, who submitted vaginal swabs for
Thus, the guidelines for GBS screening and intrapartum GBS bacterial culture.
antibiotic prophylaxis (IAP) developed by the Centers for Exclusion Criteria. Women (1) who did not undergo GBS
Disease Control and Prevention (CDC) recommend that screening; (2) with prenatal diagnosis of fetal malformation; (3)
who underwent habitual abortion (abortion ≥3 times consecutive-
pregnant woman should be tested for GBS between 35 ly); and (4) had received antibiotics in the week prior to admission.
and 37 weeks of pregnancy, and pregnant women positive Of the 51,734 admitted pregnant women to our hospital for la-
for GBS should receive IAP during labor. The coloniza- bor between April 1, 2014 and March 31, 2017, 49,908 women and
tion rate of GBS in pregnant women and the disease bur- 50,933 newborns (including 61 stillbirths) were enrolled in this
den in developing countries are currently unknown as study (Fig. 1). GBS-infected infants from previous pregnancies
were defined as previously delivered infants with invasive GBS dis-
large, population-based sampling studies are rarely con- ease, identified via medical record review.
ducted. Rates of GBS colonization in the vagina during
late-pregnancy women have been reported to be 10.1– Study Data Set
32.4% in China [4, 5]. However, GBS has not been con- A questionnaire consisting of three categories was designed to
sidered a major neonatal pathogen, which may have over- collect demographic and clinical information from each of the en-
rolled pregnant women and newborns.
looked invasive neonatal GBS infections. Furthermore,
routine screening for GBS colonization in late pregnancy Specimen Collection
has not been widely followed. This study retrospectively GBS Culture. Vaginal secretions were collected from the lower
investigated the vaginal GBS colonization rate in late third of the vagina of 49,908 pregnant women at 35–37 weeks of
pregnancy and its effect on neonatal GBS infection using gestation or with preterm birth (regardless of gestation age) by
swab, which were inserted into the plastic TranSwab device (pro-
population-based sampling at a single center. vided by Qi Xing Biotechnology Company of China, Taiwan).
Then the plastic tube was cultured at 35 ° C with 5% CO2 for 24–48
h. Chromogenic agars in the tube underwent color change in the
presence of β-hemolytic colonies of GBS.
46.4.80.155 - 12/15/2020 8:43:51 AM
302 Neonatology 2019;115:301–309 Zhu/Huang/Lin/Chen
DOI: 10.1159/000494133
Iceland Consortium - Nova
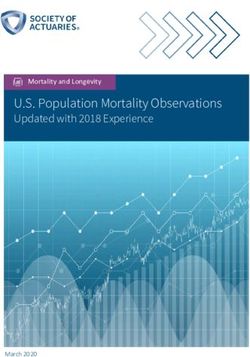
Downloaded by:Color version available online
25
22.47%
21.42% 21.01%
20.23%
20
17.24% 17.45% 16.25%
GBS colonization rate, %
16.33%
14.66% 15.05%
164.44% 14.47% 14.66%
15 16.36% 13.07% 13.27% 13.21%
12.49% 15.69%
14.58%
13.37% 12.95% 10.50% 13.61%
12.61% 12.37% 12.08%
10 11.87% 11.95%
9.63% 9.56% 9.29%
8.46% 8.70%
5 7.13%
6.29% 2014–2015
2015–2016
2016–2017
0
April May June July Aug. Sep. Oct. Nov. Dec. Jan. Feb. March
Month
Fig. 2. GBS colonization rate over 3 years.
Tracheal secretions, gastric fluid, and blood samples were col- Statistical Analyses
lected from neonates born to the enrolled pregnant women and Continuous data were calculated as means and standard devia-
subsequently admitted into the neonatal ward. GBS was detected tion, and Student’s t test was used to determine the significance of
in these samples by culture detection. differences between continuous variables. Categorical variables
were expressed as percentage and analyzed by χ2 test or Fisher’s
Study Definitions/Diagnosis Criteria exact test. GBS-EOD was assessed with univariate and multivariate
Early-Onset GBS Disease (GBS-EOD). Positive GBS culture in methods. Multivariate analysis was performed using binary logis-
tracheal secretions (collected within 30 min after admission, prior tic regression analysis. A p value 20% in November and December, 2014, and then de-
(a) Standard IAP. Intravenous injection of penicillin (5 million clining again (Fig. 2).
units i.v. initial dose, then 2.5–3.0 million units every 4 h until de-
livery), ampicillin (2 g i.v. initial dose, then 1 g i.v. every 4 h until Risk Factors of GBS Vaginal Colonization in Late
delivery) or cefazolin (2 g i.v. initial dose, then 1 g i.v. every 8 h
until delivery) for GBS prophylaxis completed ≥4 h before deliv- Pregnancy Women
ery. During labor or rupture of membranes, IAP was given to all This cohort was divided into a GBS-positive and GBS-
women testing positive for GBS colonization, excluding those un- negative groups according to GBS detection. The demo-
dergoing cesarean delivery with intact amniotic membranes before graphic and clinical characteristics of the two groups are
the onset of labor. listed in Table 1. There was a statistically significant dif-
(b) Non-Standard IAP. Intravenous injection of antibiotics for
GBS prophylaxis completed < 4 h before delivery, or using addi- ference in the rate of multiple pregnancy, gestational dia-
tional antibiotics (e.g., clindamycin or vancomycin), or no admin- betes mellitus, gestational vaginitis, gestational bacteri-
istration of antibiotics before delivery. uria, and GBS disease in previous offspring. The percent-
46.4.80.155 - 12/15/2020 8:43:51 AM
GBS Detection in Pregnancy and Neonatology 2019;115:301–309 303
Neonates DOI: 10.1159/000494133
Iceland Consortium - Nova
Downloaded by:Table 1. Demographic and clinical characteristics of GBS-positive and GBS-negative mothers
Characteristics GBS-positive GBS-negative t/χ2 value p
(n = 6,933) (n = 42,975)
Maternal age, years 29.70±4.30 29.51±4.32 0.404 0.625Table 2. Outcomes of pregnancy in GBS-positive and GBS-negative groups
Variables GBS-positive GBS-negative χ2 value p
(n = 6,933) (n = 42,975)
Cesarean section 2,413 (34.80) 14,485 (33.71) 3.219 0.073
PROM 1,039 (14.99) 6,148 (14.31) 2.241 0.134
Chorioamnionitis 1,174 (16.93) 3,807 (8.86) 433.266 0.000
MSAF 491 (7.08) 3,328 (7.74) 3.702 0.054
Preterm labor 420 (6.06) 2,386 (5.55) 2.880 0.090
Fetal distress 698 (10.07) 4,074 (9.48) 2.386 0.122
IUGR 445 (6.40) 3,025 (7.04) 3.552 0.059
Intrapartum temperature ≥37.5° C 1,256 (18.12) 4,313 (10.04) 393.176 0.000
Postpartum hemorrhage 135 (1.95) 894 (2.08) 0.524 0.469
Postpartum GBS mastitis 18 (0.26) 46 (0.11) 10.853 0.001
Data are presented as n (%). PROM, premature rupture of membranes; IUGR, intrauterine growth retardation;
MSAF, meconium-stained amniotic fluid.
Table 3. Birth outcomes in the GBS-positive and GBS-negative groups
Variables GBS-positive GBS-negative χ2 value p
(n = 6,933) (n = 42,975)
Total childbirths 7,100 43,833
Live births 7,068 43,704
Stillbirths 32 (0.45) 129 (0.29) 4.744 0.029
Male gender 3,530 (49.94) 22,276 (50.97) 2.566 0.109
Preterm 432 (6.11) 2,538 (5.81) 1.026 0.311
34 weeks ≤ GA < 37 weeks 324 (4.58) 1,837 (4.20) 2.165 0.141
GATable 4. Characteristics of 75 GBS-EOD cases had non-standard IAP (5.14%; 9/175, p = 0.000). No p
value < 0.05 was noted in univariate analysis after we
Variables Cohort divided GBS-negative women into GBS-EOD and non-
(n = 75)
GBS-EOD groups.
Maternal
AgeTable 5. Perinatal risk factors in neonatal GBS-EOD and non-GBS-EOD groups
Variables GBS-EOD Non-GBS-EOD χ2 value p
(n = 62) (n = 6,871)
Maternal
Age 2 (3.23) 77 (1.12) – 0.157a
18 h 15 (24.19) 776 (11.29) 10.116 0.001
Intrapartum temperature ≥37.5° C 20 (32.26) 1,236 (17.99) 8.434 0.004
Chorioamnionitis 24 (38.71) 1,150 (16.74) 21.090 0.000
Fetal distress 8 (12.90) 690 (10.04) 0.555 0.456
Standard IAP 53 (85.48) 6705 (97.58) 31.812 0.000
Neonatal
Male gender 33 (53.23) 3,497 (50.90) 0.134 0.715
Premature 5 (8.06) 427 (6.21) 0.113 0.737
Low birth weight (18 h 0.473 0.346 1.875 1 0.171 1.605 0.815–3.161
Intrapartum temperature ≥37.5° C –0.093 0.389 0.057 1 0.811 0.911 0.425–1.954
Chorioamnionitis 0.853 0.359 5.632 1 0.018 2.346 1.160–4.745
Standard IAP –1.167 0.460 6.429 1 0.011 0.311 0.126–0.767
Small for gestational age 0.287 0.395 0.562 1 0.468 1.332 0.614–2.890
Constant –3.553 0.485 53.767 1 0.000 0.029
PROM, premature rupture of membranes.
In this study, the vaginal GBS colonization rates fluc- Such fluctuations may suggest intermittent, seasonal GBS
tuated remarkably from month to month. GBS positivity colonization [20].
was lowest in the summer, while over 20% of subjects Case reports have suggested that inhibition of vaginal
were GBS-positive in the winter (November to January). lactobacillus can increase vaginal pH, harming the vagi-
46.4.80.155 - 12/15/2020 8:43:51 AM
GBS Detection in Pregnancy and Neonatology 2019;115:301–309 307
Neonates DOI: 10.1159/000494133
Iceland Consortium - Nova
Downloaded by:nal microecology, which may facilitate GBS colonization. IAP should be provided to pregnant women experiencing
Thus, our data indicated that pregnant women with vag- GBS bacteriuria, unexplained bacteriuria, or with a med-
initis, urinary tract infection, and gestational diabetes ical history of invasive GBS disease in previous pregnan-
mellitus provide more favorable conditions for vaginal cies. We call for universal screening of pregnant women
GBS colonization, as expected. GBS colonization may for GBS colonization at 35–37 weeks of gestation, and to
also progress to GBS infection including asymptomatic ensure that standard IAP is available for GBS-positive
bacteriuria, urinary tract infection, bacteremia, chorio- women.
amnionitis, and endometritis in pregnant women. The Our study has limitations. This retrospective and sin-
incidence of chorioamnionitis and perinatal fever are sig- gle-center study design carries inherent bias. Our GBS
nificantly higher in GBS-positive pregnant women in this culture technique was not the most sensitive, and only a
study, because GBS β-hemolytic toxin tends to bind and single vaginal swab from each subject was collected,
penetrate chorion. GBS can invade the uterine cavity and which may lead to underestimation of GBS colonization
cause GBS infection in amniotic fluid. The fetus became rates. Our findings were limited to the pregnant popula-
infected when GBS-infected amniotic fluid was inhaled, tion in Xiamen metropolitan area between 2004 and
which could explain the high frequencies of stillbirth and 2017. Large, multicenter GBS clinical investigations are
severe asphyxia among GBS-positive pregnant women in required to support the development of national CDC
our study. guidelines and to reduce the impact of GBS colonization
GBS is a major invasive bacterial pathogen with early- for mothers and children.
onset (GBS-EOD from birth to 7 days old) or late-onset
(aged >1 week) neonates in Europe, USA, and other de-
veloped countries with reported EOD rates from 0.5 to 4 Conclusions
per 1,000 live births [21]. This study indicated that the
overall incidence of GBS-EOD was 1.48/1,000 live births In this retrospective study, we found that the average
in Xiamen, China, which was significantly higher than the GBS-positive rate was 14%, fluctuating remarkably from
rate reported in Japan (0.08/1,000) [22], Thailand (0.10– month to month (from < 9 to >21%). The rate of GBS-
0.27/1,000), or other regions of China (0.28/1,000) [23, EOD in infants born to GBS-positive mothers was 29
24]. However, the rate was similar to that reported in 1993 times that in neonates born to GBS-negative mothers. We
in the USA (1.7/1,000) before the establishment of mater- also found that standard IAP significantly reduced GBS-
nal GBS universal screening by the CDC [1]. Neverthe- EOD in the offspring of these mothers. Our findings sup-
less, GBS-EOD represents a severe threat to neonates at port universal screening for GBS colonization in preg-
the most vulnerable stage of life. The previously reported nant women at 35–37 weeks of gestation and implemen-
lower incidence of GBS-EOD in China may reflect a lack tation of IAP for GBS-positive pregnant women.
of effective monitoring of GBS infection.
This study indicated that the incidence of GBS-EOD
in infants born to GBS-positive mothers was 29 times Acknowledgments
higher than in those born to GBS-negative mothers, sim-
This work was supported by the Science and Technology Plan-
ilar to the 25-fold higher incidence reported in the USA
ning Project of Xiamen 2017 (3502Z20171006).
[25]. Risk factors for neonatal GBS-EOD identified in this
study include high load of GBS colonization (i.e., gesta-
tional bacteriuria and GBS disease in previous offspring) Statement of Ethics
and chorioamnionitis. An effective approach to prevent
neonatal GBS-EOD is to screen pregnant women prior to The ethics committee of the Xiamen Maternity and Child
labor and prescribe IAP if positive. In the study, 6,758 Health Care Hospital approved the study, and all participants pro-
cases received standard IAP, and the incidence of neona- vided written informed consent.
tal GBS-EOD was reduced to 0.78%, significantly lower
than that achieved with non-standard IAP (5.14%). IAP
has reduced neonatal GBS-EOD incidence by 80% (from Disclosure Statement
1.7 per 1,000 live births in 1993 to 0.4 in 2008) in the USA The authors declare that they have no conflict of interest.
[1, 26]. Routine screening for GBS colonization in late
pregnancy in China has yet to be established. However,
46.4.80.155 - 12/15/2020 8:43:51 AM
308 Neonatology 2019;115:301–309 Zhu/Huang/Lin/Chen
DOI: 10.1159/000494133
Iceland Consortium - Nova
Downloaded by:References
1 Verani JR, McGee L, Schrag SJ; Division of 11 Ma TW, Chan V, So CH, Hui AS, Lee CN, Hui 18 Li XH, Wu HL, Sun J. Fluorescent quantita-
Bacterial Diseases, National Center for Im- AP, et al. Prevention of early onset group B tive PCR method and chromogenic culture
munization and Respiratory Diseases, Cen- streptococcal disease by universal antenatal method for detecting group B streptococcus
ters for Disease Control and Prevention culture-based screening in all public hospitals in pregnant women. Zhongguo Fuyou Baoji-
(CDC). Prevention of perinatal group B strep- in Hong Kong. J Matern Fetal Neonatal Med. an. 2017;32:2779–81.
tococcal disease—revised guidelines from 2018 Apr;31(7):881–7. 19 Davies HD, Miller MA, Faro S, Gregson D,
CDC, 2010. MMWR Recomm Rep. 2010 Nov; 12 Lu B, Li D, Cui Y, Sui W, Huang L, Lu X. Ep- Kehl SC, Jordan JA. Multicenter study of a
59(RR-10):1–23. idemiology of Group B streptococcus isolated rapid molecular-based assay for the diagnosis
2 Pettersson K. Perinatal infection with Group from pregnant women in Beijing, China. Clin of group B Streptococcus colonization in
B streptococci. Semin Fetal Neonatal Med. Microbiol Infect. 2014 Jun;20(6):O370–3. pregnant women. Clin Infect Dis. 2004 Oct;
2007 Jun;12(3):193–7. 13 Wang YC, He SJ. Correlation between the col- 39(8):1129–35.
3 Blaschke AJ, Pulver LS, Korgenski EK, Savitz onization of group B streptococcus and the 20 Lin XZ, Wu JN, Zhang XQ. Relationship be-
LA, Daly JA, Byington CL. Clindamycin-re- level of defensins in pregnant women in tween group B Streptococcus colonization in
sistant group B Streptococcus and failure of Hanzhong. Xiandai Jianyan Yixue Zazhi. late pregnancies and neonatal infection. Chin
intrapartum prophylaxis to prevent early-on- 2013;28:87–9. J Perinat Med. 2016;19:491–6.
set disease. J Pediatr. 2010 Mar;156(3):501–3. 14 Money D, Dobson S, Cole L, Karacabeyli E, 21 Edmond KM, Kortsalioudaki C, Scott S,
4 Shi CY, Qu SH, Yang L, Yang HX. [Detection Blondel-Hill E, Milner R, et al. An evaluation Schrag SJ, Zaidi AK, Cousens S, et al. Group
of maternal colonization of group B strepto- of a rapid real time polymerase chain reaction B streptococcal disease in infants aged young-
coccus in late pregnancy by real-time poly- assay for detection of group B streptococcus er than 3 months: systematic review and me-
merase chain reaction and its effect on peri- as part of a neonatal group B streptococcus ta-analysis. Lancet. 2012 Feb; 379(9815): 547–
natal outcome]. Zhonghua Fu Chan Ke Za prevention strategy. J Obstet Gynaecol Can. 56.
Zhi. 2010 Jan;45(1):12–6. Chinese. 2008 Sep;30(9):770–5. 22 Matsubara K, Hoshina K, Suzuki Y. Early-on-
5 Michael W, Jiang PR, Cao Y. Neonatal group 15 Berkley JA, Lowe BS, Mwangi I, Williams T, set and late-onset group B streptococcal dis-
B streptococcal infection during perinatal pe- Bauni E, Mwarumba S, et al. Bacteremia ease in Japan: a nationwide surveillance study,
riod. Chin J Evid Based Pediatr. 2011;6:241–4. among children admitted to a rural hospital 2004-2010. Int J Infect Dis. 2013 Jun;
6 Edwards MS, Baker CJ. Group B streptococcal in Kenya. N Engl J Med. 2005 Jan; 352(1):39– 17(6):e379–84.
infections. 5th ed. Philadelphia (PA): Saun- 47. 23 Yossuck P, Preedisripipat K. Neonatal group
ders; 2005. 16 Chaudhary M, Rench MA, Baker CJ, Singh P, B streptococcal infection: incidence and clini-
7 Shao XM, Ye HM, Qiu XS. Practical Neona- Hans C, Edwards MS. Group B Streptococcal cal manifestation in Siriraj Hospital. J Med
tology. 4th ed. Beijing: People's Medical Pub- Colonization Among Pregnant Women in Assoc Thai. 2002 Aug;85 Suppl 2:S479–87.
lishing House; 2011. Delhi, India. Pediatr Infect Dis J. 2017 Jul; 24 Liu H, Zeng H, Wang W, Deng Q, Margarit I,
8 Xie X, Gou WL. Obstetrics and Gynecology. 36(7):665–9. Rinaudo CD, et al. Estimating the burden of
8th ed. Beijing: People's Medical Publishing 17 Marió MJ, Valenzuela I, Vásquez AE, Illanes invasive Group B Streptococcal disease in
House; 2013. SE. Prevention of Early-onset Neonatal young infants in southern mainland China:
9 Spencer JP. Management of mastitis in breast- Group B Streptococcal Disease. Rev Obstet an observational study. Int J Clin Exp Med.
feeding women. Am Fam Physician. 2008 Sep; Gynecol. 2013;6(2):63–8. 2015 Aug;8(8):13699–707.
78(6):727–31. 25 Boyer KM, Gotoff SP. Strategies for chemo-
10 Yu HW, Lin HC, Yang PH, Hsu CH, Hsieh prophylaxis of GBS early-onset infections.
WS, Tsao LY, et al. Group B streptococcal in- Antibiot Chemother (1971). 1985;35:267–80.
fection in Taiwan: maternal colonization and 26 Melin P. Neonatal group B streptococcal dis-
neonatal infection. Pediatr Neonatol. 2011 ease: from pathogenesis to preventive strate-
Aug;52(4):190–5. gies. Clin Microbiol Infect. 2011 Sep; 17(9):
1294–303.
46.4.80.155 - 12/15/2020 8:43:51 AM
GBS Detection in Pregnancy and Neonatology 2019;115:301–309 309
Neonates DOI: 10.1159/000494133
Iceland Consortium - Nova
Downloaded by:You can also read