Evaluating attitudes and behaviours in the rational use of medicines in health-care services for refugees and migrants in Turkey
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Evaluating attitudes and behaviours in the rational use of medicines in health-care services for refugees and migrants in Turkey
ABSTRACT
Rational use of medicines (RUM) requires that “patients receive medications appropriate to their clinical needs, in
doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them
and their community”. While physicians and pharmacists can help patients to understand and use medications
properly, cultural and linguistic barriers, especially in migrant and refugee situations, poor health literacy, and health-
care workers’ attitudes and behaviours may affect RUM. This mixed study was conducted to evaluate attitudes and
behaviours with respect to RUM in health-care services for refugees and migrants in Turkey. Physicians, pharmacists
and patients participated in surveys, focus group discussions and in-depth interviews in May–October 2020. While
most of the physicians (92.5%) and pharmacists (68.3%) stated that they informed their patients about RUM, patients
expressed a need for more information about medicines and prescriptions. Both pharmacists and physicians reported
that there was high patient demand for antibiotics. Cultural and linguistic barriers at pharmacy level, compatibility
issues affecting different electronic medical recording systems, especially in migrant health centres (MHCs), and a
communication gap between physicians and pharmacists were the main issues affecting pharmaceutical services
(with a likely impact on RUM) for migrants and refugees in Turkey. Health-care services could be enhanced and RUM
improved by giving health-care workers in MHCs and pharmacists regular training on good pharmaceutical care,
promoting the use of language-appropriate visual information materials in patient consultations, providing public
health education on RUM, and bridging the communication gap between pharmacists and physicians.
Keywords © World Health Organization 2021
Some rights reserved. This work is available under the Creative Commons Attribution-
RATIONAL USE OF MEDICINES NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/
licenses/by-nc-sa/3.0/igo).
REFUGEES AND MIGRANTS
Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial
PHARMACEUTICAL CARE
purposes, provided the work is appropriately cited, as indicated below. In any use of this work,
there should be no suggestion that WHO endorses any specific organization, products or services.
The use of the WHO logo is not permitted. If you adapt the work, then you must license your work
under the same or equivalent Creative Commons licence. If you create a translation of this work,
you should add the following disclaimer along with the suggested citation: “This translation was not
created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy
of this translation. The original English edition shall be the binding and authentic edition: Evaluating
attitudes and behaviours in the rational use of medicines in health-care services for refugees and
migrants in Turkey. Copenhagen: WHO Regional Office for Europe; 2021”.
Document number:
Any mediation relating to disputes arising under the licence shall be conducted in accordance with
WHO/EURO:2021-2775-42533-59100 the mediation rules of the World Intellectual Property Organization.
Suggested citation. Evaluating attitudes and behaviours in the rational use of medicines in health-
care services for refugees and migrants in Turkey. Copenhagen: WHO Regional Office for Europe;
2021. Licence: CC BY-NC-SA 3.0 IGO.
Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris.
Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. To
submit requests for commercial use and queries on rights and licensing, see http://www.who.int/
about/licensing.
Third-party materials. If you wish to reuse material from this work that is attributed to a third party,
such as tables, figures or images, it is your responsibility to determine whether permission is needed
for that reuse and to obtain permission from the copyright holder. The risk of claims resulting from
infringement of any third-party-owned component in the work rests solely with the user.
General disclaimers. The designations employed and the presentation of the material in this
publication do not imply the expression of any opinion whatsoever on the part of WHO concerning
the legal status of any country, territory, city or area or of its authorities, or concerning the
delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate
border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they
are endorsed or recommended by WHO in preference to others of a similar nature that are not
mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by
initial capital letters.
All reasonable precautions have been taken by WHO to verify the information contained in this
publication. However, the published material is being distributed without warranty of any kind, either
Cover photo: © WHO expressed or implied. The responsibility for the interpretation and use of the material lies with the
Design and layout: 4PLUS4.dk reader. In no event shall WHO be liable for damages arising from its use.Evaluating attitudes and behaviours in the rational use of medicines in health-care services for refugees and migrants in Turkey
iii Contents Preface............................................................................................................................. iv Acknowledgements........................................................................................................... v Abbreviations.................................................................................................................... vi Executive summary........................................................................................................... vii 1. Background.................................................................................................................. 1 Pharmaceutical services for refugees.............................................................................................. 1 Community pharmacists’ role in improving health and use of medicines................................ 2 Pharmaceutical services for refugees in Turkey............................................................................. 2 Rationale for the study......................................................................................................................... 3 Study aims and objectives.................................................................................................................. 3 2. Methodology................................................................................................................. 4 Study design.......................................................................................................................................... 4 Study population................................................................................................................................... 4 Sampling approach............................................................................................................................... 4 Data collection....................................................................................................................................... 6 Ethical approval..................................................................................................................................... 6 3. Results......................................................................................................................... 7 Demographic characteristics of the study population.................................................................. 7 Perspectives on prescription and consultation services.............................................................. 8 Patients’ compliance with treatment................................................................................................ 15 Health literacy and health communication...................................................................................... 19 Adverse drug reactions (ADRs).......................................................................................................... 22 Electronic prescriptions (e-prescriptions)........................................................................................ 23 Information sources used when prescribing................................................................................... 25 Training in the rational use of medicine (RUM) and training needs of physicians................... 26 Challenges and possible interventions for better pharmaceutical services............................. 27 Which factors are important in developing pharmaceutical services for Syrians?................. 29 4. Discussion.................................................................................................................... 32 5. Conclusion and recommendations................................................................................ 35 References........................................................................................................................ 36
iv
Preface
The conflict in the Syrian Arab Republic has caused one In November 2018 the RHP conducted the Workshop
of the world’s largest and most dynamic displacement on Refugee and Migrant Health in Turkey: Survey
crises, affecting millions of lives. Coordinating all and Research Consultation to identify gaps in the
its activities from the Country Office in Ankara, information and evidence required for programme
WHO supports the response to the crisis through development and adaptation and for informing policies
its operations in Turkey, including the cross-border on migrant health in Turkey. The workshop brought
response from the field office in Gaziantep and a health together more than 57 national and international
response to refugees in Turkey. Through the Refugee experts from academia, the Turkish Ministry of Health,
Health Programme (RHP) in Turkey, efforts have been United Nations agencies and WHO collaborating
made to strengthen the national health system by centres and led to the formulation of the programme’s
supporting employment opportunities for Syrian health research framework. Within this framework, a series
workers and translators, building capacity for mental of studies were implemented in the fields of mental
health care, providing linguistic and culturally sensitive health, health literacy, women’s and children’s health,
health services, and supporting home care for older the health workforce and noncommunicable diseases.
refugees and those with disabilities. This study, entitled Evaluating attitudes and behaviours
in the rational use of medicines in health-care services
Activities of the programme are defined within the for refugees and migrants in Turkey, is one of the studies
scope of the Regional Refugee and Resilience Plan that was implemented within the Refugee Health
(3RP), a broad partnership platform for over 270 Programme research framework. It was implemented
development and humanitarian partners to provide within the scope of the Improved access to health
coordinated support in countries bordering Syria that services for Syrian refugees in Turkey project with
are heavily impacted by the influx of refugees. This funding from the EU Regional Trust Fund in Response to
platform capitalizes on the knowledge, capacities and the Syrian Crisis.
resources of humanitarian and development actors to
provide a single strategic, multisectoral and resilience-
based response. Supported by several donors, WHO’s
activities are complementary to the SIHHAT1 project,
which was funded by the European Union (EU). This
project operates under the EU’s Facility for Refugees in
Turkey and focuses on strengthening the provision of
primary and secondary health-care services to Syrian
refugees, building and supporting a network of migrant
health centres across the country, and employing
additional health personnel, including Syrian doctors
and nurses.
1 SIHHAT is the Turkish acronym of the project named “Health Status of the Syrian Population under Temporary Protection and Related
Services Provided by Turkish Authorities”.v
Acknowledgements
The WHO Health Emergencies team in Turkey would
Authors
like to thank all the stakeholders who contributed to the Melda Keçik
implementation of this study. Special thanks go to the WHO Country Office in Turkey, WHO Regional Office for
management of the WHO Country Office in Turkey and Europe
to Kanuni Keklik, Mesil Aksoy, Fatma Isli, Kattal Fatih
Aydiner and Ozlem Kahraman Tunay of the Ministry of Omur Cinar Elci
Health of the Republic of Turkey. Special thanks also WHO Country Office in Turkey, WHO Regional Office for
go to Elif Goksu and Altin Malaj of the WHO Country Europe
Office in Turkey for their support and to the Turkish
Pharmacists Association (TPA) for their valuable Monica Zikusooka
contributions to data collection, data analysis and WHO Country Office in Turkey, WHO Regional Office for
overall implementation of the study. The research team Europe
also thanks the Tandans Data Science Consulting team
and Mesut Sancar for their efforts and contributions.
Peer reviewers
This report was produced with the financial assistance Dr Lordes Cantarero Arevalo
of the European Union through the EU Regional Trust Associate Professor, Department of Pharmacy,
Fund in Response to the Syrian Crisis. University of Copenhagen, and WHO Collaborating
Centre for Research and Training in the Patient
Perspective on Medicines Use
Dr Margaret Kay
Senior Lecturer at the University of Queensland,
Australia
This document was produced with the financial assistance of the European Union. The
views expressed herein can in no way be taken to reflect the official opinion of the
European Union.vi
Abbreviations
ADR adverse drug reaction
COPD chronic obstructive pulmonary disease
e-prescription electronic prescription
EDQM European Directorate for the Quality of Medicines and HealthCare
EU European Union
FGD focus group discussion
FIP International Pharmaceutical Federation (Fédération Internationale Pharmaceutique)
GPP good pharmacy practice
IDI in-depth interview
KII key informant in-depth interview
MHC migrant health centre
MHTC migrant health training centre
NCD noncommunicable disease
RHP Refugee Health Programme
RUM rational use of medicines
SD standard deviation
SIHHAT Turkish acronym of the project named “Health Status of the Syrian Population under
Temporary Protection and Related Services Provided by Turkish Authorities”
TPA Turkish Pharmacists’ Association
TUFAM Turkish Pharmacovigilance Centervii
Executive summary
Pharmaceutical care is a practice philosophy in which For this study, a mixed methodology was adopted to
pharmacists collaborate directly with other health-care effectively capture perspectives from both patients
professionals and with patients to improve the rational and service providers in three Turkish provinces –
use of medicines (RUM) by identifying, resolving and Istanbul, Ankara and Sanliurfa – and to produce policy
preventing medication-related problems. As health recommendations. A total of 200 physicians (79.0%
professionals who regularly interact with patients, male) and 129 pharmacists (65.1% male) responded to
pharmacists play an essential role in closing the gap the surveys, while in the qualitative part of the study 30
between the potential benefit of medicines and the people participated in focus group discussions, 13 in
actual value realized upon use. Pharmacists should aim key informant in-depth interviews, and 30 in online in-
to contribute to improving health and helping patients depth interviews conducted between May and October
to make rational use of their medicines. They have a 2020. Data collection tools were prepared on the basis
key responsibility to provide patient education on RUM of the European Directorate for the Quality of Medicines
and to support patient compliance with their treatment. and HealthCare (EDQM) pharmaceutical care guidelines,
They also have a role to play in monitoring treatment the joint FIP/WHO good pharmacy practice (GPP)
to verify its effectiveness and to check for any adverse guidelines, and the Turkish GPP guidelines. Prior to
drug reactions. implementation, the questionnaire was translated from
English to Arabic and then back-translated to English by
Patients need pharmacists’ help to understand the a different translator, following the standard procedure
importance of taking medications properly, the correct for cultural adaptation. The questionnaire was then
timing of doses, interactions with foods and other pretested on a sample of subjects and modified prior to
medicines, and possible side effects. However, cultural use. Trained data collectors conducted online interviews
and linguistic barriers and poor health literacy make with participants.
it difficult for patients to get the help they need from
pharmacists, especially in refugee situations. At the While there was a high participation rate for physicians,
same time, pharmacists’ and physicians’ attitudes and with a response rate of 95.7%, the level of interest
behaviours may have an impact on RUM. among pharmacists was relatively low, with a response
rate of 41.6%. With respect to pharmaceutical care
Through field visits and discussions with physicians services, 68.3% of the pharmacists stated that they
working in migrant health centres (MHCs) and informed their patients about RUM. However, these
community pharmacists within the vicinity of MHCs consultation services were limited to an explanation of
serving refugees, WHO in Turkey has established that the use of the medicine at the appropriate time, at the
refugees may face cultural and linguistic barriers in appropriate dose and in an appropriate manner. Almost
using medicines and pharmaceutical care services. all (92.5%) of the physicians claimed that they informed
It is crucial, therefore, that strategies to overcome their patients about the medicines prescribed. Some,
these challenges are adopted, allowing refugees to however, left this job to pharmacists. Patients felt that
use medicines rationally and to make effective use of they needed more information from both physicians
the available pharmaceutical services. This study was and pharmacists about medicines and prescriptions,
conducted to identify attitudes, opinions, behaviour including information on side effects, adverse effects
patterns and challenges that patients, physicians and and doses. At the pharmacies, the main obstacles to
community pharmacists face with respect to RUM providing detailed consultation services were excessive
and pharmaceutical services. The study also aimed to workload and language problems between pharmacy
develop recommendations for interventions to improve staff and patients. There were both cultural and
RUM and pharmaceutical care services for refugees linguistic barriers, and it was clear that pharmacists
and migrants. needed more training in providing high-quality
information and care services to their patients.viii
Although, in general, patients’ compliance with order to enhance health-care services for patients.
treatment was said by the physicians to be sufficient, As a summary, the study results raised the following
the pharmacists and some physicians stated that low recommendations.
compliance continued to be a problem for health-care
services. While some of the pharmacists put patient 1. Syrian health-care professionals working in MHCs
compliance as high as 70%, others reported less than and pharmacists serving refugee populations
60% compliance. The main reason for such a difference should be given regular professional training
was that patients often did not return to the pharmacy sessions on pharmaceutical care services, good
to provide feedback, so pharmacists could not follow up prescribing procedures, RUM, antibiotics, patient
on most patients. and health education and communication, and
pharmacovigilance, in order to improve prescription
It was apparent that, for both physicians and practice and patient monitoring.
pharmacists, patients’ demand for antibiotics was huge
2. Use of language-appropriate visual information
– a fact that was confirmed by patients themselves.
materials, such as pictograms and bilingual labels,
in patient consultations should be promoted in
Compatibility issues affecting different electronic
order to overcome language barriers and simplify
medical recording systems, especially in MHCs, were
information on medicine instructions, doses,
highlighted as another problem for both physicians
precautions and side effects.
and pharmacists. Also, some of the pharmacists
and physicians were not fully aware that they had 3. Public health education on RUM, including public
access to patients’ electronic medical records. This campaigns in Arabic and other languages, should
indicates that patients’ medical history is not taken into be implemented to raise awareness of excessive
consideration by some pharmacists and physicians antibiotic use and the dangers of antimicrobial
in their medical decision-making. There is a major resistance.
professional communication gap between physicians 4. The communication gap between pharmacists and
and pharmacists. Some physicians claimed that physicians should be bridged in order to enhance
pharmacists exceeded their authority on the other hand, health-care services for patients. Activities such
pharmacists said that – because of the communication as joint meetings and training programmes would
gap – they could not intervene even when there were provide an opportunity to improve professional
errors in a prescription. communication between pharmacists and
physicians.
The study participants suggested that it would be highly
beneficial to strengthen both virtual and face-to-face 5. System incompatibilities that affect electronic
training programmes on pharmaceutical care services, medical recording systems should be resolved.
good prescribing procedures, RUM, antibiotics, and Such issues could be resolved by government
pharmacovigilance for Syrian health-care professionals agencies, such as the Turkish Ministry of Health and
working in MHCs and pharmacists in the vicinity of the Social Security Institution.
MHCs serving refugees. In addition, further professional
training sessions for pharmacists on patient and
health education and communication would be helpful
in the context of refugees and migrants. Closing the
communication gap between pharmacists, physicians
and patients would improve pharmaceutical services
for refugees and migrants. To that end, patient
training/consultation materials, such as pictograms
and bilingual labels, should be developed and
disseminated; and linguistic barriers could be reduced
if well-trained Arabic-speaking support staff were
employed in pharmacies. Joint meetings and training
programmes to improve professional communication
between pharmacists and physicians are needed inBackground 1
1. Background
Since the beginning of the Syrian crisis in 2011, Turkey has been one of the primary destinations for Syrian refugees.
During the early years of the crisis, the Turkish government settled most of the refugees in temporary shelters in
the border provinces, but the growing number of refugees gradually exceeded the capacity of these shelters. For
this reason, it became necessary over time to transfer them to residential settlements within the host community,
and today most of the 3.6 million Syrian refugees have been relocated to permanent urban residential settlements.
Initially, the Turkish government provided registration and settlement services through the Disaster and Emergency
Management Authority, but this responsibility was later handed over to the Directorate General of Migration
Management of the Ministry of Interior.
The Government of Turkey, through the Ministry of Health, established the migrant health centre (MHC) system to
meet the health-care needs of the refugees. MHCs are managed through the SIHHAT project, which is operational
in 29 provinces with a high Syrian population density2. Registered refugees have access to all primary health-care
services in Turkey, as well as to MHCs, free of charge. Across Turkey there are currently 178 active MHCs, and these
have been visited by over 1.45 million patients for at least one consultation. The MHC structure was planned and
organized on the model of primary health-care provision in Turkey, so there is no difference in its service organization
from the national health system. However, in some MHCs there is an additional level of specialist outpatient services
in internal medicine, paediatrics and gynaecology, the aim of which is to increase the use of such services and thus to
reduce pressure on the national health-care system.
There are also differences in the financing of MHC services, which are funded by the SIHHAT project and other
government sources, with additional funding from the European Union and other external donors. In addition, the
profile of their health-care personnel and their target population is different. In the Turkish health-care system,
personnel consist of physicians who are either Turkish nationals or appropriately accredited foreigners, nurses and
allied health professionals. In MHCs, health-care service providers are mostly Syrian nationals who are only authorized
to work in these facilities. Like all primary health-care facilities in Turkey, MHCs provide services, including vaccination
services, to anyone regardless of their nationality and registration status. Before starting employment in MHCs, health
workers receive initiation training in the Turkish health-care system through a tailored adaptation training programme
implemented by WHO in collaboration with the Ministry of Health. The adaptation training is delivered in WHO-
supported migrant health training centres (MHTCs), which are located in seven provinces and also provide health-care
services.
Pharmaceutical services for refugees
Refugees and migrants face specific challenges in effectively accessing pharmaceutical services. Some of the critical
challenges to high-quality use of medicines in refugee communities include communication and language constraints,
cultural issues, limited health literacy, financial cost and the health system itself (Kay et al., 2016). Overall, cultural
and linguistic barriers, coupled with poor health literacy, remain significant challenges in the continuum of health-care
services for refugee and migrant populations. It has been noted in the literature that mortality rates among refugees
resulting from infectious diseases, noncommunicable diseases (NCDs), malnutrition, and mental and social stress
are likely to be higher as a result of factors including overcrowding, contaminated and inadequate water supplies,
poor sanitation, and physical and mental stress (Cronin et al., 2008; Heudtlass, Speybroeck & Guha-Sapir, 2016).
The higher level of poor health among refugees is likely to increase the risk of inappropriate use of medicines and
2 SIHHAT is the Turkish acronym of the project named “Health Status of the Syrian Population under Temporary Protection and Related
Services Provided by Turkish Authorities”.2 Evaluating attitudes and behaviours in the rational use of medicines
in health-care services for refugees and migrants in Turkey
adverse drug reactions (ADRs). Their high vulnerability to poor health notwithstanding, refugees and migrants have
cultural, linguistic and health literacy constraints that make it difficult for them to access and use pharmaceutical
services correctly. Similar constraints – linguistic barriers, in particular – make it difficult for physicians and
community pharmacists to provide effective, equitable and understandable services that respond to refugees and
migrants’ cultural and health beliefs and practices. And yet the attitudes and behaviours of these primary role players
towards the use of medicines among refugees and migrants in Turkey is still unknown. To the authors’ knowledge,
there has been no previous study examining pharmaceutical care services for refugees in Turkey. Understanding
the attitudes and behaviours of refugees and health-care providers – especially physicians and pharmacists –
towards pharmaceutical services and the rational use of medicines (RUM) is critical if we are to develop policy
recommendations to ensure high-quality health care for refugees and migrants.
Community pharmacists’ role in improving health and use of medicines
Good pharmacy practice (GPP) guidelines emphasize the importance of medicines as a critical element of health-
care services as part of both primary and secondary prevention (early diagnosis and treatment). However, GPP is not
usually achieved, thereby creating a gap between the proven and actual efficacy of medicines in practice (FIP/WHO,
[n.d.]). This gap is a result of attitude and behaviour issues such as inappropriate medicine selection, inappropriate
dosage, improper administration, poor patient adherence, medicine–medicine and medicine–food interactions, and
ADRs (FIP/WHO, [n.d.]). Even though most of these ADRs are preventable, they increase the length of hospital stays,
economic burden and risk of death (Classen et al., 1997; Johnson & Bootman, 1995; Sultana, Cutroneo & Trifirò, 2013).
Issues such as proper use of medicines, patients with chronic diseases, polypharmacy, use of herbal/traditional
medicines, and medicine–medicine or medicine–food interactions must be reviewed by pharmacists at the time they
dispense medicines (Regulation of Pharmacists and Pharmacies, 2014; Carter & Bonanni, 2019).
The regular interactions between patients and pharmacists mean that the latter, as health professionals, play an
essential role in closing the gap between the potential benefit of medicines and the value they actually achieve in
practice. Pharmacists should aim to contribute to improving health and to help patients to make the best use of
their medicines (FIP/WHO, [n.d.]); they have a key responsibility to provide patient education on RUM and to support
patients’ compliance with treatment; and they have a role to play in monitoring treatment to verify effectiveness
and ADRs. For these reasons, pharmacists should play an active role in health-care services by collaborating with
physicians and patients to produce the best outcomes for patients. A randomized controlled intervention study from
Jordan reported that pharmacist–physician partnership and pharmacists’ involvement in clinical services significantly
reduced treatment-related problems among Syrian refugees (Al Alawneh, Nuaimi & Basheti, 2019). Community
pharmacies are particularly convenient places to access pharmaceutical services because they typically have long
opening hours and offer free services that do not require an appointment. To develop efficient interventions, it is
therefore important to understand community pharmacists’ attitudes and behaviours as they provide pharmaceutical
services, including advice on RUM, to refugees and migrants.
Pharmaceutical services for refugees in Turkey
In Turkey, medicines for outpatient refugee patients are provided by community pharmacies, as they are for the
Turkish population. Registered refugees, however, have access to prescribed medicines free of charge. The cost of
medicines is reimbursed to community pharmacies through the Directorate General of Migration Management of
the Ministry of Interior. Pharmaceutical services are not embedded in MHCs but are provided through community
pharmacies that are easily accessible from nearby MHCs. All community pharmacists are Turkish nationals, as
Syrian nationals are not permitted to practise pharmacy in Turkey. There is also a mandatory electronic prescription
(e-prescription) system in Turkey, which operates in MHCs as well.Background 3
Rationale for the study
Patients need pharmacists’ help to understand the importance of taking medications properly, correct timing of
doses, interactions with foods and other medicines, and possible side effects. However, cultural and linguistic barriers
and poor health literacy make it difficult for patients to get the help they need from pharmacists, especially in refugee
situations, while pharmacists’ and physicians’ attitudes and behaviours may affect RUM.
Staff belonging to the WHO Country Office Refugee Health Programme undertook an exploratory field visit and
held discussions with physicians working in MHCs and with community pharmacists working in the vicinity of
MHCs serving refugee patients in Ankara. Preliminary observations showed that refugees might face cultural and
linguistic barriers in using medicines and pharmaceutical care services. It is, therefore, crucial to adopt strategies
that overcome these challenges, allowing refugees to use medicines rationally and to make effective use of available
pharmaceutical services. Responding to this need, the WHO Refugee Health Programme, in collaboration with the
Turkish Ministry of Health, conducted this study to gain an understanding of all role players’ attitudes and behaviours
towards RUM and community pharmaceutical services. The intention is that the outcomes of the study will be used to
develop strategies and interventions that improve RUM and community pharmaceutical care services for refugees.
Study aims and objectives
The aims of this study are, first, to evaluate the attitudes and behaviours of physicians working at MHCs, of
community pharmacists whose pharmacies are close to MHCs, and of patients who use the services provided by
MHCs; and then to make recommendations for culturally and linguistically appropriate pharmaceutical care services
that meet the primary health-care needs of migrants and refugees living in Turkey.
The specific objectives of the study are:
• to identify the attitudes, opinions and behaviour patterns of patients, physicians and community pharmacists with
respect to RUM and pharmaceutical care services;
• to determine the challenges faced by patients, physicians and community pharmacists with respect to RUM and
pharmaceutical care services; and
• to develop recommendations for patient/user-centred interventions to improve RUM and to provide good
pharmaceutical care services for refugees and migrants.4 Evaluating attitudes and behaviours in the rational use of medicines
in health-care services for refugees and migrants in Turkey
2. Methodology
Study design
A mixed-methods approach was adopted to effectively capture perspectives from both patients and service providers
and to produce policy recommendations. A mixed-methods approach is recommended for capturing data and
producing effective policy recommendations, particularly when investigating complex health problems, such as
patient–provider interactions (NIH, 2018; Lorenzini, 2017; Fiorini, Griffiths & Houdmont, 2016).
Study population
Three distinct populations were included in the study: physicians working at MHCs, community pharmacists whose
pharmacies are close to MHCs, and patients who use the services provided by MHCs. The physician population
consisted entirely of physicians working in MHCs. The pharmacist population was made up of a sample of local
community pharmacists operating within a 1500-metre radius of the sampled MHCs. Patients were selected from
adults (18 years and over) who were using the services provided by the sampled MHCs and consented to participate.
The study was conducted in Istanbul, Ankara and Sanliurfa, which constitute three of the seven provinces where
RHTCs are located. These three provinces reflect the distribution pattern of refugees throughout the country: Sanliurfa
at the Syrian border in the south-east; Ankara in the central plateau; and Istanbul in the west of the country.
Sampling approach
Sampling approach for the quantitative data collection
Physicians working at MHCs and community pharmacists with pharmacies close to MHCs were included in the
quantitative component of the study.
Physicians
The sampling frame for physicians was based on the distribution of the MHCs in Istanbul, Sanliurfa and Ankara
(Table 1). Since the total number of physicians was only 209, all physicians working in the selected MHCs were
invited to participate in the quantitative data collection for the study. The Migrant Health Department of the Ministry
of Health distributed information about the survey, including the study aims and objectives, data collection methods,
confidentiality measures, risks and benefits, and the expectations of participants; it also gave the contact information
of the research team to all physicians in the three provinces.
Table 1. Distribution of MHCs and MHTCs, by province
Province Standard MHCs Extended MHCsa MHTCs Total
Istanbul 48 55 10 113
Sanliurfa 31 28 11 70
Ankara 7 9 10 26
Total 86 92 31 209
a
Extended MHCs provide selected specialized services, such as paediatrics, obstetrics and gynaecology, in addition
to basic family and general practice health-care services.Methodology 5 Pharmacists The total number of practising community pharmacists in the three provinces was 7746 (Istanbul, 5164; Sanliurfa, 490; Ankara, 2092). In Turkey, each pharmacy is registered and owned by one pharmacist. The initial list of pharmacies was provided by the Turkish Pharmacists’ Association (TPA). However, because of the distances and target populations involved, not all the pharmacies serve refugee and migrant patients. Therefore, as a first step in the sampling procedure, a total of 2035 pharmacies situated within a radius of 1500 m of the MHCs were identified on the basis of GIS (geographic information system) data. The sample size was estimated based on the proportional stratified sampling approach, using the WinPepi Epidemiological Calculator (version 11.65) at a 95% confidence interval and 0.05 margin of error. Participating pharmacists were selected randomly, with an expected loss of 20% included as an additional loss to follow-up. The distribution and calculated sample of pharmacies are shown in Table 2. Table 2. Distribution of pharmacies within a 1500 m radius of MHCs and sample estimation, by province Province Pharmacies % Sample Istanbul 1480 72.73 225 Sanliurfa 426 20.93 65 Ankara 129 6.34 20 Total 2035 100.0 310 Sampling approach for the qualitative data collection Physicians working at MHCs, community pharmacists with a pharmacy close to MHCs, and patients using services provided by MHCs were included in the qualitative data collection. Although face-to-face focus group discussions (FGDs) were planned, because of COVID-19 restrictions, online in-depth interviews (IDIs) and key informant in-depth interviews (KIIs) were implemented in addition to virtual FGDs. The distribution of FGDs, KIIs and IDIs among the three participant groups is shown in Table 3. Table 3. Distribution of FGDs, KIIs and IDIs, by participant group Participant group FGDs KIIs IDIs Physicians 5 9 – Community pharmacists – 4 12 Patients – – 18 Total 5 13 30 Physicians Five FGDs, each with six participants, were conducted among physicians: two in Istanbul, two in Sanliurfa and one in Ankara. Additionally, nine KIIs were conducted with representatives of the provincial health directorates, which manage the provincial health systems (including MHCs) under the direction of the Turkish Ministry of Health. Community pharmacists Twelve IDIs were conducted with pharmacists: four each in Istanbul, Sanliurfa and Ankara. Additionally, four KIIs were conducted with the presidents of three provincial chambers of pharmacists, which are professional bodies that monitor and regulate pharmacy health-care services.
6 Evaluating attitudes and behaviours in the rational use of medicines
in health-care services for refugees and migrants in Turkey
Patients
Eighteen IDIs were conducted with refugees who benefit from the service of MHCs: six each in Istanbul, Sanliurfa and
Ankara.
Data collection
Data collection started with surveys and was followed by FGDs, IDIs and KIIs, which were guided by the preliminary
results of the quantitative data collection and conducted between May and October 2020. Quantitative data from
physicians and pharmacists were collected using a questionnaire, while for FGDs, IDIs and KIIs interviewers used
guidelines and set questions. Data collection tools were prepared on the basis of the European Directorate for the
Quality of Medicines and HealthCare (EDQM) pharmaceutical care guidelines, the Turkish GPP guidelines and the joint
FIP/WHO GPP guidelines (FIP/WHO, [n.d.]). Prior to implementation, the questionnaire was translated from English
to Arabic and then back-translated to English by a different translator, following the standard procedure for cultural
adaptation. The questionnaire was then pretested on a sample of subjects and modified prior to use. Trained data
collectors conducted online interviews with participants.
Qualitative data were collected by means of FGDs, IDIs and KIIs. The questions for FGDs, IDIs and KIIs were designed
using the preliminary results of the quantitative data analyses. This allowed observations drawn from the quantitative
data to be explored in depth. Because of COVID-19 pandemic restrictions, qualitative data collection was implemented
using Computer Assisted Personal Interview (CAPI).
Data were collected by a research company in close collaboration with the Ministry of Health, the TPA and WHO
technical staff. Physicians and pharmacists were given secure links to access the web conferencing tool according
to interview schedules provided by MHC managers and the TPA. Patients who agreed to join the in-depth interviews
were also given links to access the web conferencing tool.
Training of data collectors
Data collectors were trained by a public health expert before the data collection in line with the objectives of the study
and under the supervision of WHO technical staff.
Data monitoring and quality checking
Data collection monitoring and data quality checking were conducted alongside data collection under the supervision
of WHO technical staff. Data quality monitoring included checking for logical flow of information, consistency of
answers, contextual links between closed and open-ended questions, and typographical errors. Data collectors were
given one-to-one coaching to improve their performance and eliminate errors.
Challenges for data collection
Since this implementation model was different from previous ones, the study team faced many challenges and
constraints. In both the quantitative and the qualitative data collections, some participants did not attend meetings at
the specified time and date. This was due to technical and other unspecified problems. It was not possible to conduct
virtual FGDs with pharmacists because they were available at different times.
Ethical approval
Ethical approval for the study was received from the WHO Ethics Review Committee, as well as from Gazi University
Ethics Commission through an institutional review board (IRB).Results 7
3. Results
Demographic characteristics of the study population
Two hundred physicians from a total of 209 and 129 pharmacists from a total sample of 310 participated in the study.
The overall response rate was 95.7% for physicians and 41.6% for pharmacists.
Physicians
More than half of the physicians who participated in the survey (54.0%) worked in Istanbul; 33.5% in Sanliurfa; and
12.5% in Ankara. A total of 200 physicians (79.0% male) responded to the survey. Their mean (± standard deviation
(SD)) age was 42.2 ± 11.5 years; their median age was 46 years (range: 26–71). 60.5% of the physicians had a
specialty: the three most common specialties were paediatrics (18%), gynaecology (10.5%) and internal medicine
(10%). 62% of the physicians had more than 15 years’ experience.
Community pharmacists
A majority of the pharmacists who participated in the survey (61.2%) worked in Istanbul; 26.4% in Sanliurfa; and 12.4%
in Ankara. A total of 129 pharmacists (65.1% male) responded to the survey. Their mean (± SD) age was 42.2 ± 11.9
years; their median age was 40 years (range: 22–74). 60.4% of the pharmacists had more than 15 years’ experience
(similar to the physicians in this respect). The pharmacists stated that they saw an average of 89 patients per day.
Patients
At the patient IDIs, eight out of 18 patients stated that they did not have a disease diagnosed by a physician and
did not use any medicine regularly. Diseases mentioned by other patients were blood coagulation problems,
inguinal hernia, migraine, hypertension, hyperglycaemia, cholesterol, glaucoma, heart disease and kidney transplant.
Hypertension and hyperglycaemia were the conditions most commonly mentioned by patients.
All the patients had visited an MHC in the last year, the majority (14 patients) within the last month. The reasons
for visiting MHCs were: prescription (three patients); experiencing pain (six patients); vaccination for children (two
patients); infectious diseases (three patients); heart complaints (one patient); reproductive health complaints (one
patient); and check-up examination (one patient).
84.4% of the physicians reported receiving
requests for prescriptions without an
examination. However, almost all (99%)
stressed that they would never prescribe
antibiotics without an examination.8 Evaluating attitudes and behaviours in the rational use of medicines
in health-care services for refugees and migrants in Turkey
Perspectives on prescription and consultation services
History-taking
Physicians
While planning a patient’s treatment, almost all the physicians (97.5%) asked whether the patient had any allergies.
In addition, 96.0% of the physicians asked female patients about their pregnancy and breastfeeding status before
planning treatment. Three-quarters of the physicians reported that they also asked about surgical history (75.9%) or
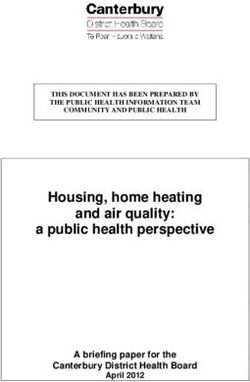
family genetic diseases (73.0%) (Fig. 1).
Fig. 1. Medical history taken by physicians while planning patients’ treatment
Gene�c diseases in the family
Pa�ent’s sex
Surgical history
Other medica�ons used
Liver disease
Other important diseases suffered
Kidney disease
Pa�ent’s age
Any chronic disease
Pregnancy/breas�eeding
Allergies
0 10 20 30 40 50 60 70 80 90 100
%
Generally ask Rarely ask
While 70.5% of the physicians stated that they did not have access to patients’ medical history, 15.5% did not know
whether they had such access (Table 4).
Table 4. Physicians’ access to patients’ health records
Yes No Do not know
Health records
n % n % n %
Medical records 18 14.0 91 70.5 20 15.5
Previous medications and prescriptions 72 55.8 45 34.9 12 9.3
Chronic disease reports 69 53.5 44 34.1 16 12.4
The FGDs revealed that physicians could access a patient’s medical history if the patient was recorded in the Ministry
of Health’s electronic medical recording system. It was also reported that, if patients relocated between cities, it was
impossible to access their medical records. KIIs with physicians supported their claims and also revealed that they
could not always understand the Turkish information given in the electronic medical recording system.Results 9
KII.06.Phy4.3 This is the biggest problem; we do not know how often the patient uses the medicine.
Sometimes we request that information from the pharmacy; this is a serious problem, especially for regions
with a high patient circulation. If they receive a prescription from a local physician, we cannot see that
information in the electronic medical recording system. This is a problem for us.
KII.34.Phy7. We can see a patient’s history from the electronic medical recording system. If the patient
always visits the same centre, we can see all the medical records. But if they visit another MHC, or if they
relocate to another province, we cannot see their medical records. One MHC cannot see a patient’s history
held by another MHC. I wish every doctor was able to see every patient’s history.
Community pharmacists
In Istanbul 74.7% of the pharmacists who participated in the study stated that they could not access the medical
records of their patients; the corresponding figure for Ankara was 81.3% and for Sanliurfa 55.9%. The proportion
of pharmacists in Ankara who could access patients’ previous prescriptions was 56.3%; in Sanliurfa, 94.1%; and in
Istanbul, 39.2%. 56.3% of pharmacists in Ankara and 88.2% of pharmacists in Sanliurfa claimed that they only had
access to patients’ chronic disease reports; the figure for Istanbul was 38.0%. Some pharmacists mentioned that,
through the electronic medical recording system, they could access only current prescriptions, prescriptions made
within the previous year and chronic disease reports.
IDI.34.Pha2. We have access to patients’ medication history and reports. We have access to details of
prescriptions if they were purchased from ourselves previously. However, we do not have access to a
patient’s medication history, duration and dosage unless that medicine was dispensed by my pharmacy. We
have access to medical board reports relating to a patient’s treatment, indicating which medicine was used
and how long it was supposed to be used for. It is not our responsibility to plan our patients’ treatment.
Physicians have access to a patient’s treatment plan. Also, there are concerns over patient privacy and data
confidentiality. So we see the records that cover our own services – there isn’t any concern that we should
have access to more.
IDI.63.Pha1. We can see the medicines they use from the moment they arrived in Turkey through the
electronic medical recording system. But we can only learn about the medicines they used before coming
to Turkey if they tell us. We have the same problem with chronic disease reports.
Patients’ demand for prescriptions without a diagnosis
Physicians
Almost two thirds of physicians (65.5%) said that nothing could influence their decision whether or not to issue
a prescription. They also pointed out that there were posters at MHCs, in Arabic, that aimed to increase patient
awareness of the rational use of antibiotics.
FGD.34.Phy2. The important thing is that I shouldn’t prescribe any unnecessary medicine. I advise him [the
patient] to go back [to the pharmacy] and request those prescribed medicines from the pharmacy. I want
him to understand that this is a serious issue.
The great majority of the physicians (96%) indicated that they did not write a prescription without an examination.
However, 2.5% of physicians stated that they might write a prescription if the patient argued, or if the patient had a
chronic disease (1%), or if they did not have time to explain the illegality of the patient’s request (0.5%).
3 The code KII.06.Phy4 signifies the key informant in-depth interview with physician 4 from Ankara (Phy = physician; Pha = pharmacist; Pat
= patient; 34 = Istanbul, 06 = Ankara, 63 = Sanliurfa).10 Evaluating attitudes and behaviours in the rational use of medicines
in health-care services for refugees and migrants in Turkey
During FGDs, the physicians noted that patients could get any medicine without a prescription in Syria, and they
expected this to continue in Turkey. Sometimes they requested a medicine they had searched for on the internet.
The physicians also stated that patients would go to private physicians or hospitals for examination and then come
back to MHCs to issue their prescriptions. When physicians did not agree to prescribe medicines based on a patient’s
request, tensions emerged, and it was highlighted that this could be a serious problem for physicians.
KII.34.Phy8. Patients do not want to wait in line; they want the doctor to prescribe medicines based on their
own request. They bring prescriptions from private medical centres for us to issue. This can cause trouble.
Poor education and low socioeconomic status exacerbate these discussions.
FGD.34.Phy1. A small number of patients search Google and check medicines online and come to us
without knowing whether the prescription is appropriate or not.
Patients
It was observed that, when physicians were not prepared to prescribe on the basis of a patient’s request, patients
perceived this as a problem. This was mentioned in the IDIs with patients.
IDI.34.Pat6. Sometimes the doctor does not prescribe the medicine I request.
Antibiotics
Physicians
The physicians stated that patient requests for prescriptions of antibiotics were common. Most (84.4%) also
mentioned that they received requests for prescriptions without an examination. However, almost all (99%) stressed
that they would never prescribe antibiotics without an examination. Furthermore, they stated that they provided
information about appropriate use of antibiotics.
As previously mentioned, the physicians noted that it was normal in Syria for patients to get antibiotics whenever they
felt they needed them, without a prescription; they requested antibiotics from physicians or pharmacists even though
they did not need them. According to the physicians, antibiotic usage was a cultural issue for these patients – if they
did not get antibiotics, they felt that they would not get better. The physicians complained that patients came to MHCs
not for treatment but just for a prescription of antibiotics. However, there were also many patients who did follow
physicians’ advice about proper use of antibiotics.
FGD.63.Phy1. The problems are rooted in the common culture. Our society believes in antibiotics, anti-
inflammatory medicines and muscle relaxants. This is because some physicians disseminate this false
information. Some patients listen to our advice when we explain the risks; others don’t.
FGD.63.Phy2. They think if they don’t take antibiotics, they won’t get better.
Community pharmacists
More than the physicians, the pharmacists stated that they frequently received patient requests for antibiotics. Only
3.9% of the pharmacists claimed that they had never received a request for antibiotics without a prescription; 10.1%
had occasionally received such a request. Although the pharmacists provided information on antibiotics, they believed
that the information was insufficient as a result of language issues. Most of the pharmacists (78.3%) provided their
patients with information on the rational use of antibiotics. According to IDIs with pharmacists, refugee patients
believed that antibiotics were the best medicine to treat infectious diseases and frequently asked for antibiotics.
However, the pharmacists added that this number of requests had fallen over the years.Results 11
IDI.34.Pha2. Previously the requests were much more intense – we used to get them almost every day. But
they have become less frequent over time.
Pharmacists mentioned that they referred patients to physicians and provided information on antibiotics that
explained that they should only be used if prescribed.
IDI.06.Pha4. I even had Arabic information brochures from the Ministry of Health that we shared with
patients. We inform them that they should not use antibiotics unless they are needed, but they are very
stubborn about antibiotics.
IDI.34.Pha2. Of course, we give them information. For a year, we had a lot of problems in this regard. We
have seen this not only with Syrian patients but with all patients. Because in previous years they were
available without a prescription.
Sometimes the pharmacists reiterated the challenges they faced in working with physicians to support patients’
treatment. With limited opportunities to engage with physicians on patient prescriptions, they provided antibiotics that
had been prescribed even if they personally did not think it was the correct course of action.
Patients
According to IDIs with patients, five of them (out of 18) stated that they had requested antibiotics from pharmacies
without a prescription.
Consultation services to patients
Physicians
Most physicians (92.5%) stated that they had generally provided information on RUM while counselling their patients;
of these, 67.5% responded that they had always provided this information to their patients.
In FGDs, the physicians highlighted the importance of sharing information on RUM with patients at the time of making
a prescription. According to the physicians, patients trusted them and always looked to them for information on their
medicines. The physicians said that they tried to provide the necessary information in face-to-face conversations,
adding that patients often do not read the patient leaflet. Some mentioned that they took the added precaution of
writing the name of the medicine in Arabic for their patients.
FGD.34.Phy1. While I am prescribing, I disclose all relevant information. I tell them how many medicines I
have prescribed and tell them to come back if they don’t understand when they go to the pharmacy. I write
the name of the medicine in Arabic to help them understand.
Most of the physicians (83.9%) stated that, after giving their patients information, they generally (usually or always)
checked whether they had understood it clearly or not (Fig. 2).You can also read