EFFECTIVENESS OF PUBLIC HEALTH MEASURES IN REDUCING THE INCIDENCE OF COVID-19, SARS-COV-2 TRANSMISSION, AND COVID-19 MORTALITY: SYSTEMATIC REVIEW ...
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
RESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Effectiveness of public health measures in reducing the incidence
of covid-19, SARS-CoV-2 transmission, and covid-19 mortality:
systematic review and meta-analysis
Stella Talic,1,2 Shivangi Shah,1 Holly Wild,1,3 Danijela Gasevic,1,4 Ashika Maharaj,1
Zanfina Ademi,1,2 Xue Li,4,6 Wei Xu,4 Ines Mesa-Eguiagaray,4 Jasmin Rostron,4
Evropi Theodoratou,4,5 Xiaomeng Zhang,4 Ashmika Motee,4 Danny Liew,1,2 Dragan Ilic1
1
School of Public Health and ABSTRACT 37 assessed multiple public health measures as a
Preventive Medicine, Monash OBJECTIVE “package of interventions.” Eight of 35 studies were
University, Melbourne, 3004 VIC, To review the evidence on the effectiveness of included in the meta-analysis, which indicated a
Australia
2 public health measures in reducing the incidence of reduction in incidence of covid-19 associated with
Monash Outcomes Research
and health Economics (MORE) covid-19, SARS-CoV-2 transmission, and covid-19 handwashing (relative risk 0.47, 95% confidence
Unit, Monash University, VIC, mortality. interval 0.19 to 1.12, I2=12%), mask wearing (0.47,
Australia 0.29 to 0.75, I2=84%), and physical distancing (0.75,
3
DESIGN
Torrens University, VIC, Australia 0.59 to 0.95, I2=87%). Owing to heterogeneity of
4
Systematic review and meta-analysis.
Centre for Global Health, The the studies, meta-analysis was not possible for the
Usher Institute, University of DATA SOURCES
Edinburgh, Edinburgh, UK outcomes of quarantine and isolation, universal
Medline, Embase, CINAHL, Biosis, Joanna Briggs,
5
Cancer Research UK Edinburgh lockdowns, and closures of borders, schools, and
Global Health, and World Health Organization
Centre, MRC Institute of Genetics workplaces. The effects of these interventions were
COVID-19 database (preprints).
and Molecular Medicine, synthesised descriptively.
University of Edinburgh, ELIGIBILITY CRITERIA FOR STUDY SELECTION
Edinburgh, UK CONCLUSIONS
Observational and interventional studies that
6
School of Public Health and This systematic review and meta-analysis suggests
assessed the effectiveness of public health measures
The Second Affiliated Hospital, that several personal protective and social measures,
Zhejiang University School of in reducing the incidence of covid-19, SARS-CoV-2
including handwashing, mask wearing, and physical
Medicine, Hangzhou, China transmission, and covid-19 mortality.
distancing are associated with reductions in the
Correspondence to: S Talic MAIN OUTCOME MEASURES
stella.talic@monash.edu incidence covid-19. Public health efforts to implement
(ORCID 0000-0001-7739-3381) The main outcome measure was incidence of public health measures should consider community
Additional material is published covid-19. Secondary outcomes included SARS-CoV-2 health and sociocultural needs, and future research
online only. To view please visit transmission and covid-19 mortality. is needed to better understand the effectiveness of
the journal online.
DATA SYNTHESIS public health measures in the context of covid-19
Cite this as: BMJ 2021;375:e068302
http://dx.doi.org/10.1136/ DerSimonian Laird random effects meta-analysis was vaccination.
bmj-2021-068302 performed to investigate the effect of mask wearing, SYSTEMATIC REVIEW REGISTRATION
Accepted: 21 October 2021 handwashing, and physical distancing measures PROSPERO CRD42020178692.
on incidence of covid-19. Pooled effect estimates
with corresponding 95% confidence intervals were
computed, and heterogeneity among studies was Introduction
assessed using Cochran’s Q test and the I2 metrics, The impact of SARS-CoV-2 on global public health and
with two tailed P values. economies has been profound.1 As of 14 October 2021,
there were 239 007 759 million cases of confirmed
RESULTS
covid-19 and 4 871 841 million deaths with covid-19
72 studies met the inclusion criteria, of which 35
worldwide.2
evaluated individual public health measures and
A variety of containment and mitigation strategies
WHAT IS ALREADY KNOWN ON THIS TOPIC have been adopted to adequately respond to covid-19,
with the intention of deferring major surges of patients
Public health measures have been identified as a preventive strategy for
in hospitals and protecting the most vulnerable
influenza pandemics
people from infection, including elderly people and
The effectiveness of such interventions in reducing the transmission of SARS- those with comorbidities.3 Strategies to achieve these
CoV-2 is unknown goals are diverse, commonly based on national risk
WHAT THIS STUDY ADDS assessments that include estimation of numbers of
patients requiring hospital admission and availability
The findings of this review suggest that personal and social measures, including
of hospital beds and ventilation support.
handwashing, mask wearing, and physical distancing are effective at reducing
Globally, vaccination programmes have proved
the incidence of covid-19
to be safe and effective and save lives.4 5 Yet most
More stringent measures, such as lockdowns and closures of borders, schools, vaccines do not confer 100% protection, and it is not
and workplaces need to be carefully assessed by weighing the potential negative known how vaccines will prevent future transmission
effects of these measures on general populations of SARS-CoV-2,6 given emerging variants.7-9 The
Further research is needed to assess the effectiveness of public health measures proportion of the population that must be vaccinated
after adequate vaccination coverage against covid-19 to reach herd immunity depends
the bmj | BMJ 2021;375:e068302 | doi: 10.1136/bmj-2021-068302 1RESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
greatly on current and future variants.10 This public health measures, particularly in policy decision
vaccination threshold varies according to the country making.19
and population’s response, types of vaccines, groups Previous systematic reviews on the effectiveness of
prioritised for vaccination, and viral mutations, public health measures to treat covid-19 lacked the
among other factors.6 Until herd immunity to covid-19 inclusion of analytical studies,20 a comprehensive
is reached, regardless of the already proven high approach to data synthesis (focusing only on one
vaccination rates,11 public health preventive strategies measure),21 a rigorous assessment of effectiveness
are likely to remain as first choice measures in disease of public health measures,22 an assessment of the
prevention,12 particularly in places with a low uptake certainty of the evidence,23 and robust methods for
of covid-19 vaccination. Measures such as lockdown comparative analysis.24 To tackle these gaps, we
(local and national variant), physical distancing, performed a systematic review of the evidence on the
mandatory use of face masks, and hand hygiene have effectiveness of both individual and multiple public
been implemented as primary preventive strategies to health measures in reducing the incidence of covid-19,
curb the covid-19 pandemic.13 SARS-CoV-2 transmission, and covid-19 mortality.
Public health (or non-pharmaceutical) interventions When feasible we also did a critical appraisal of the
have been shown to be beneficial in fighting respiratory evidence and meta-analysis.
infections transmitted through contact, droplets,
and aerosols.14 15 Given that SARS-CoV-2 is highly Methods
transmissible, it is a challenge to determine which This systematic review and meta-analysis
measures might be more effective and sustainable for were conducted in accordance with PRISMA25
further prevention. (supplementary material 1, table 1) and with
Substantial benefits in reducing mortality were PROSPERO (supplementary material 1, table 2).
observed in countries with universal lockdowns in
place, such as Australia, New Zealand, Singapore, Eligibility criteria
and China. Universal lockdowns are not, however, Articles that met the population, intervention,
sustainable, and more tailored interventions need comparison, outcome, and study design criteria
to be considered; the ones that maintain social lives were eligible for inclusion in this systematic review
and keep economies functional while protecting (supplementary material 1, table 3). Specifically,
high risk individuals.16 17 Substantial variation exists preventive public health measures that were tested
in how different countries and governments have independently were included in the main analysis.
applied public health measures,18 and it has proved a Multiple measures, which generally contain a “package
challenge for assessing the effectiveness of individual of interventions”, were included as supplementary
material owing to the inability to report on the
individual effectiveness of measures and comparisons
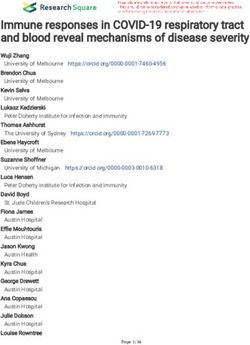
Visual Abstract Hands, face, space v covid-19 on which package led to enhanced outcomes. The
Effectiveness of public health measures
public health measures were identified from published
Summary Several public health measures, including handwashing, mask World Health Organization sources that reported
wearing, and physical distancing, were associated with a reduction on the effectiveness of such measures on a range of
in incidence of covid-
communicable diseases, mostly respiratory infections,
Study design such as influenza.
72 Met inclusion criteria 37 Excluded from analysis Given that the scientific community is concerned
Systematic review
and meta-analysis
Assessed multiple measures about the ability of the numerous mathematical
as a “package of interventions”
Evaluated individual models, which are based on assumptions, to predict
35
Risk of bias measures the course of virus transmission or effectiveness of
0 Low 27 Excluded from analysis interventions,26 this review focused only on empirical
6 Medium Owing to heterogeneity of studies studies. We excluded case reports and case studies,
2 Serious 8 Included in meta-analysis (effects synthesised descriptively)
modelling and simulation studies, studies that
provided a graphical summary of measures without
3 6 5 clear statistical assessments or outputs, ecological
studies that provided a descriptive summary of the
measures without assessing linearity or having
Assessed handwashing Assessed mask wearing Assessed physical distancing
comparators, non-empirical studies (eg, commentaries,
editorials, government reports), other reviews, articles
involving only individuals exposed to other pathogens
Outcomes Relative risk % CI
that can cause respiratory infections, such as severe
Random effects model results . .
acute respiratory syndrome or Middle East respiratory
Handwashing
syndrome, and articles in a language other than English.
Mask wearing
Physical distancing Information sources
http://bit.ly/BMJc19phm © 2021 BMJ Publishing group Ltd. We carried out electronic searches of Medline,
Embase, CINAHL (Cumulative Index to Nursing and
2 doi: 10.1136/bmj-2021-068302 | BMJ 2021;375:e068302 | the bmjRESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Allied Health Literature, Ebsco), Global Health, Biosis, with corresponding 95% confidence intervals were
Joanna Briggs, and the WHO COVID-19 database (for reported for the associations between the public
preprints). A clinical epidemiologist (ST) developed health measures and incidence of covid-19. When
the initial search strategy, which was validated by two necessary, we transformed effect metrics derived from
senior medical librarians (LR and MD) (supplementary different studies to allow pooled analysis. We used the
material 1, table 4). The updated search strategy was Dersimonian Laird random effects model to estimate
last performed on 7 June 2021. All citations identified pooled effect estimates along with corresponding 95%
from the database searches were uploaded to confidence intervals for each measure. Heterogeneity
Covidence, an online software designed for managing among individual studies was assessed using
systematic reviews,27 for study selection. the Cochran Q test and the I2 test.31 All statistical
analyses were conducted in R (version 4.0.3) and all
Study selection P values were two tailed, with P=0.05 considered to
Authors ST, DG, SS, AM, ET, JR, XL, WX, IME, and XZ be significant. For the remaining studies, when meta-
independently screened the titles and abstracts and analysis was not feasible, we reported the results in a
excluded studies that did not match the inclusion narrative synthesis.
criteria. Discrepancies were resolved in discussion
with the main author (ST). The same authors retrieved Public and patient involvement
full text articles and determined whether to include No patients or members of the public were directly
or exclude studies on the basis of predetermined involved in this study as no primary data were
selection criteria. Using a pilot tested data extraction collected. A member of the public was, however, asked
form, authors ST, SS, AM, JR, XL, WX, AM, IME, and to read the manuscript after submission.
XZ independently extracted data on study design,
intervention, effect measures, outcomes, results, and Results
limitations. ST, SS, AM, and HW verified the extracted A total of 36 729 studies were initially screened,
data. Table 5 in supplementary material 1 provides of which 36 079 were considered irrelevent. After
the specific criteria used to assess study designs. exclusions, 650 studies were eligible for full text
Given the heterogeneity and diversity in how studies review and 72 met the inclusion criteria. Of these
defined public health measures, we took a common studies, 35 assessed individual interventions and were
approach to summarise evidence of these interventions included in the final synthesis of results (fig 1) and 37
(supplementary material 1, table 6). assessed multiple interventions as a package and are
included in supplementary material 3, tables 2 and
Risk of bias within individual studies 3. The included studies comprised 34 observational
SS, JR, XL, WX, IME, and XZ independently assessed studies and one interventional study, eight of which
risk of bias for each study, which was cross checked were included in the meta-analysis.
by ST and HW. For non-interventional observational
studies, a ROBINS-I (risk of bias in non-randomised Risk of bias
studies of interventions) risk of bias tool was used.28 According to the ROBINS-I tool,28 the risk of bias was
For interventional studies, a revised tool for assessing rated as low in three studies,32-34 moderate in 24
risk of bias in randomised trials (RoB 2) tool was studies,35-58 and high to serious in seven studies.59-65
used.29 Reviewers rated each domain for overall risk of One important source of serious or critical risk of bias
bias as low, moderate, high, or serious/critical. in most of the included studies was major confounding,
which was difficult to control for because of the novel
Data synthesis nature of the pandemic (ie, natural settings in which
The DerSimonian and Laird method was used for multiple interventions might have been enforced at
random effects meta-analysis, in which the standard once, different levels of enforcement across regions,
error of the study specific estimates was adjusted to and uncaptured individual level interventions
incorporate a measure of the extent of variation, or such as increased personal hygiene). Variations in
heterogeneity, among the effects observed for public testing capacity and coverage, changes to diagnostic
health measures across different studies. It was criteria, and access to accurate and reliable outcome
assumed that the differences between studies are a data on covid-19 incidence and covid-19 mortality,
result of different, yet related, intervention effects being was a source of measurement bias for numerous
estimated. If fewer than five studies were included in studies (fig 2). These limitations were particularly
meta-analysis, we applied a recommended modified prominent early in the pandemic, and in low income
Hartung-Knapp-Sidik-Jonkman method.30 environments.47 52 62 63 65 The randomised controlled
trial66 was rated as moderate risk of bias according
Statistical analysis to the ROB-2 tool. Missing data, losses to follow-up,
Because of the differences in the effect metrics lack of blinding, and low adherence to intervention
reported by the included studies, we could only all contributed to the reported moderate risk. Tables 1
perform quantitative data synthesis for three and 2 in supplementary material 2 summarise the risk
interventions: handwashing, face mask wearing, of bias assessment for each study assessing individual
and physical distancing. Odds ratios or relative risks measures.
the bmj | BMJ 2021;375:e068302 | doi: 10.1136/bmj-2021-068302 3RESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
51 878
States (n=9), Europe (n=7), the Middle East (n=3), Africa
Records identified (n=3), South America (n=1), and Australia (n=1). Thirty
18 532 Embase 6901 CINAHL 3173 Preprints WHO four of the studies were observational and one was a
15 399 Medline 7873 Joanna Briggs, Biosis, COVID-19 randomised controlled trial. The study designs of the
and Global Health database observational studies comprised natural experiments
(n=11), quasi-experiments (n=3), a prospective cohort
15 149 (n=1), retrospective cohorts (n=8), case-control (n=2),
Duplicates and cross sectional (n=9). Twenty six studies assessed
social measures,32 34 35 37-42 44 46-48 52 53 55-61 63-65 67
36 729 12 studies assessed personal protective
Records screened measures,36 43 45 49 50 57 58 60 63 66 68 three studies assessed
travel related measures,54 58 62 and one study assessed
36 079 environmental measures57 (some interventions
Records excluded overlapped across studies). The most commonly
measured outcome was incidence of covid-19 (n=18),
650 followed by SARS-CoV-2 transmission, measured as
Full text articles assessed reproductive number, growth number, or epidemic
doubling time (n=13), and covid-19 mortality (n=8).
578 Table 1 in supplementary material 3 provides detailed
Full text articles excluded
information on each study.
148 Inadequate study design
120 Editorials or commentaries
136 Simulation studies Effects of interventions
89 No reported or ineligible outcomes Personal protective measures
33 Ineligible setting or population Handwashing and covid-19 incidence—Three studies
15 Ineligible intervention
15 Reports with a total of 292 people infected with SARS-CoV-2 and
22 Duplicates 10 345 participants were included in the analysis of the
effect of handwashing on incidence of covid-19.36 60 63
72 Overall pooled analysis suggested an estimated 53%
Total non-statistically significant reduction in covid-19
35 Studies assessing individual interventions incidence (relative risk 0.47, 95% confidence interval
8 Included in quantitative synthesis 0.19 to 1.12, I2=12%) (fig 3). A sensitivity analysis
27 Included in qualitative synthesis
37 Studies assessing multiple interventions (see supplementary material) without adjustment showed a significant reduction in
covid-19 incidence (0.49, 0.33 to 0.72, I2=12%) (fig
Fig 1 | Flow of articles through the review. WHO=World Health Organization 4). Risk of bias across the three studies ranged from
moderate36 60 to serious or critical63 (fig 2).
Study characteristics Mask wearing and covid-19 incidence—Six studies
Studies assessing individual measures with a total of 2627 people with covid-19 and 389 228
Thirty five studies provided estimates on the participants were included in the analysis examining the
effectiveness of an individual public health measures. effect of mask wearing on incidence of covid-19 (table
The studies were conducted in Asia (n=11), the United 1).36 43 57 60 63 66 Overall pooled analysis showed a 53%
reduction in covid-19 incidence (0.47, 0.29 to 0.75),
Risk of bias although heterogeneity between studies was substantial
Serious or critical High Moderate Low (I2=84%) (fig 5). Risk of bias across the six studies ranged
40 from moderate36 57 60 66 to serious or critical43 63 (fig 2).
No of studies
Mask wearing and transmission of SARS-CoV-2,
30 covid-19 incidence, and covid-19 mortality—The results
of additional studies that assessed mask wearing (not
included in the meta-analysis because of substantial
20
differences in the assessed outcomes) indicate
a reduction in covid-19 incidence, SARS-CoV-2
10 transmission, and covid-19 mortality. Specifically,
a natural experiment across 200 countries showed
0 45.7% fewer covid-19 related mortality in countries
where mask wearing was mandatory (table 1).49
M sult of
om nt
ta
tio om
t n
Co udy f
g
st n o
in
en tio
da
tc e
Another natural experiment study in the US reported a
s
iss e
ns
an Se ion
re n
nd
en fr
ou rem
d tio
to io
rv ca
g
rv n
in ct
ou
in
fi
rte lec
te io
29% reduction in SARS-CoV-2 transmission (measured
of su
i
ts le
in ss
nf
in viat
po Se
ea
of Cla
M
e
ed e
t
as the time varying reproductive number Rt) (risk ratio
nd D
re
0.71, 95% confidence interval 0.58 to 0.75) in states
cip
rti
te
where mask wearing was mandatory.58
pa
in
Fig 2 | Summary of risk of bias across studies assessing individual measures using risk A comparative study in the Hong Kong Special
of bias in non-randomised studies of interventions (ROBINS-I) tool Administrative Region reported a statistically
4 doi: 10.1136/bmj-2021-068302 | BMJ 2021;375:e068302 | the bmjRESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Study Intervention Relative risk Weight Relative risk
(95% CI) (%) (95% CI)
Doung-Ngern 2020
Handwashing 19.1 0.34 (0.13 to 0.88)
Lio 2021 Handwashing 17.8 0.30 (0.11 to 0.81)
Xu 2020 Handwashing 63.1 0.58 (0.40 to 0.84)
Random effects model (adjusted) Handwashing 100.0 0.47 (0.19 to 1.12)
Test for heterogeneity: τ2=0.053; P=0.32; I2=12%
0.1 0.5 1 2 5
Fig 3 | Meta-analysis of evidence on association between handwashing and incidence of covid-19 using modified
Hartung-Knapp-Sidik-Jonkman adjusted random effect model
significant lower cumulative incidence of covid-19 on the incidence of covid-19.37 53 57 60 63 Overall pooled
associated with mask wearing than in selected countries analysis indicated a 25% reduction in incidence of
where mask wearing was not mandatory (table 1).68 covid-19 (relative risk 0.75, 95% confidence interval
Similarly, another natural experiment involving 15 0.59 to 0.95, I2=87%) (fig 6). Heterogeneity among
US states reported a 2% statistically significant daily studies was substantial, and risk of bias ranged from
decrease in covid-19 transmission (measured as case moderate37 53 57 60 to serious or critical63 (fig 2).
growth rate) at ≥21 days after mask wearing became
mandatory,50 whereas a cross sectional study reported Physical distancing and transmission of SARS-CoV-2
that a 10% increase in self-reported mask wearing and covid-19 mortality
was associated with greater odds for control of SARS- Studies that assessed physical distancing but were not
CoV-2 transmission (adjusted odds ratio 3.53, 95% included in the meta-analysis because of substantial
confidence interval 2.03 to 6.43).45 The five studies differences in outcomes assessed, generally reported
were rated at moderate risk of bias (fig 2). a positive effect of physical distancing (table 2). A
natural experiment from the US reported a 12%
Environmental measures decrease in SARS-CoV-2 transmission (relative risk
Disinfection in household and covid-19 incidence 0.88, 95% confidence interval 0.86 to 0.89),40 and
Only one study, from China, reported the association a quasi-experimental study from Iran reported a
between disinfection of surfaces and risk of secondary reduction in covid-19 related mortality (β −0.07,
transmission of SARS-CoV-2 within households (table 95% confidence interval −0.05 to −0.10; PRESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Table 1 | Study characteristics and main results from studies that assessed individual personal protective and environmental measures
Public health Outcome Study Risk of
Reference, country Study design measure Sample size measure duration Effect estimates: conclusions bias
Doung-Ngern et al,63 Case-control Handwashing 211 cases, 839 Incidence 1-31 MarRegular handwashing: adjusted odds Serious or
Thailand controls 2020 ratio 0.34 (95% confidence interval 0.13 critical
to 0.87): associated with lower risk of
SARS-CoV-2*
Lio et al,36 China Case-control Handwashing 24 cases, 1113 Incidence 17 Mar-15 Adjusted odds ratio 0.30 (95% Moderate
controls Apr 2020 confidence interval 0.11 to 0.80):
reduction in odds of becoming
infectious*
Xu et al,60 China Cross sectional Handwashing n=8158 Incidence 22 Feb-5 Mar Relative risk 3.53 (95% confidence Moderate
comparative 2020 interval 1.53 to 8.15): significantly
increased risk of infection with no
handwashing*
Bundgaard et al,66 Randomised Mask wearing 2392 cases, 2470 Incidence Apr and May Odds ratio 0.82 (95% confidence Moderate
Denmark controlled controls 2020 interval 0.54 to 1.23): 46% reduction to
23% increase in infection*
Doung-Ngern et al,63 Case-control Mask wearing 211 cases, 839 Incidence 1-31 Mar Adjusted odds ratio 0.23 (95% Serious or
Thailand controls 2020 confidence interval 0.09 to 1.60): critical
associated with lower risk of SARS-CoV-2
infection*
Lio et al,36 China Case-control Mask wearing 24 cases, 1113 Incidence 17 Mar-15 Odds ratio 0.30 (95% confidence Moderate
controls Apr 2020 interval 0.10 to 0.86): 70% risk
reduction*
Xu et al,60 China Cross sectional Mask wearing 8158 people Incidence 22 Feb-5 Mar Relative risk 12.38 (95% confidence Moderate
comparative 2020 interval 5.81 to 26.36): significantly
increased risk of infection*
Krishnamachari et al,43 Natural Mask wearing 50 states Incidence Apr 2020 3-6 months, adjusted odds ratio 1.61 Serious or
US experiment (cumulative rate) (95% confidence interval 1.23 to 2.10): critical
>6 months, 2.16 (1.64 to 2.88): higher
incidence rate with later mask mandate
than with mask mandate in first month*
Wang et al,57 China Retrospective Mask wearing 335 people Incidence 28 Feb-27 Odds ratio 0.21 (95% confidence Moderate
cohort (assessed as Mar 2020 interval 0.06 to 0.79): 79% reduction in
attack rate†) transmission of SARS-CoV-2*
Cheng et al,68 China Longitudinal Mask wearing 961 cases (HKSAR), Incidence 31 Dec 2019- Incidence rate 49.6% (South Korea) v Moderate
comparative (South Korea v average control not 8 Apr 2020 11.8% (HKSAR) PRESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Study Intervention Relative risk Weight Relative risk
(95% CI) (%) (95% CI)
Bundagaard 2021 Mask wearing 22.2 0.82 (0.54 to 1.24)
Doung-Ngern 2020 Mask wearing 7.6 0.23 (0.05 to 0.97)
Krishnamachari 2021 Mask wearing 26.6 0.77 (0.71 to 0.84)
Lio 2021 Mask wearing 11.1 0.30 (0.10 to 0.88)
Xu 2020 Mask wearing 23.6 0.34 (0.24 to 0.48)
Wang 2020 Mask wearing 8.9 0.21 (0.06 to 0.76)
Random effects model Mask wearing 100.0 0.47 (0.29 to 0.75)
Test for heterogeneity: τ2=0.214; PRESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Table 2 | Study characteristics and main results from studies assessing individual social measures
Public health Study dura- Risk of
Reference, country Study design measure Sample size Outcome tion Effect estimates: conclusions bias
Jarvis et al,65 UK Cross sectional Stay at home 1356 cases R0 Feb-24 Mar R0: pre-intervention 3.6, post-intervention 0.60 Serious or
or isolation 2020 (95% confidence interval 0.37 to 0.89): 3.0 R0 critical
decrease
Khosravi et al,55 Iran Cross sectional Stay at home 993 cases R0 20 Feb-01 Apr R0: pre-intervention 2.70 (95% confidence Moderate
or isolation 2020 interval 2.10 to 3.40), post-intervention 1.13
(1.03 to 1.25): 1.5 R0 decrease
Dreher et al,41 US Retrospective Stay at home 49 states and R0 NS Odds ratio 0.07 (95% confidence interval 0.01 Low
cohort or isolation territories to 0.37): decrease in odds of having a positive
R0 result*
Liu et al,58 US Natural Stay at home 50 states Rt 21 Jan-31 May Risk ratio 0.49 (95% confidence interval 0.43 to Moderate
experiment or isolation 2020 0.54): contributed about 51% to reduction in Rt*
Alfano et al,52 Italy Natural Lockdown 202 countries, Incidence 22 Jan-10 May β coefficient −235.8 (standard error −11.04), Serious or
experiment 22 018 people 2020 PRESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Table 2 | Continued
Public health Study dura- Risk of
Reference, country Study design measure Sample size Outcome tion Effect estimates: conclusions bias
Guo et al,40 US Natural Business 50 states and one Rt 29 Jan-31 July Relative risk 0.88 (95% confidence interval 0.86 Moderate
experiment closure territory (Virgin 2020 to 0.89): associated with 12% decrease in risk
Islands) of Rt*
Voko et al,53 Europe Natural Physical 28 countries Incidence 1 Feb-18 Apr Incidence rate ratio 1.23 (95% confidence Moderate
experiment distancing 2020 interval 1.19 to 1.28), 0.98 (0.97 to 0.99): 26%
decrease in incidence*
Van den Berg et Retrospective Physical 99 390 staff Incidence 24 Sep 2020- ≥3 v ≥6 feet adjusted incidence rate ratio 1.01 Moderate
al,37 US cohort distancing (adjusted) 27 Jan 2021 (95% confidence interval 0.75 to 1.36), larger
physical distancing not associated with lower
rates of SARS-CoV-2*‡
Xu et al,60 China Cross sectional Physical 8158 people Incidence 22 Feb-5 Mar Relative risk 2.63 (95% confidence interval 1.48 Moderate
comparative distancing 2020 to 4.67): significantly increased risk of infection*
Doung-Ngern et al,63 Case-control Physical 211 cases, 839 Incidence 1-31 Mar >1m physical distance adjusted odds ratio Serious or
Thailand distancing controls 2020 0.15; 95% confidence interval 0.04 to 0.63)): critical
associated with lower risk of SARS-CoV-2
infection*
Wang et al,57 China Retrospective Physical 335 people Incidence 28 Feb-27 Mar Odds ratio 18.26 (95% confidence interval 3.93 Moderate
cohort distancing (proportions 2020 to 84.79): risk of household transmission was
assessed as 18 times higher with frequent daily close contact
attack rate†) with the primary case*
Alimohamadi et al,47 Quasi- Physical NS Incidence, 20 Feb-13 Incidence β coefficient −1.70 (95% confidence Serious or
Iran experimental distancing mortality May 2020 interval −2.3 to 1.1), mortality β coefficient critical
−0.07 (−0.05 to −0.10): reduced incidence and
mortality*
Quaife et al,61 Africa Cross-sectional Physical 237 cases R0 1 -31 May R0: pre-intervention 2.64, post-intervention 0.60 Moderate
comparative distancing 2020 (interquartile range 0.50-0.68): 2.04 decrease
in R0
Guo et al,40 US Natural Physical 50 states and one Rt 29 Jan-31 Jul Relative risk 0.88 (95% confidence interval 0.86 Moderate
experiment distancing territory (Virgin 2020 to 0.89): associated with a 12% decrease in risk
Islands) of Rt*
R0=reproductive number; Rt=time varying reproductive number.
*Interpretation of findings as reported in the original manuscript.
†Percentage of individuals who tested positive over a specified period.
‡Not an effective intervention.
retrospective cohort study observed a 14.1% reduction reported that lockdown was associated with an 11%
in risk after implementation of universal lockdown reduction in transmission of SARS-CoV-2 (relative risk
(table 2).46 These studies were rated at high risk of 0.89, 95% confidence interval 0.88 to 0.91).40 All the
bias52 and moderate risk of bias46 56 (fig 2). studies were rated at low risk of bias33 39 to moderate
risk40 64 (fig 2).
Lockdown and covid-19 mortality
The three studies that assessed universal lockdown Travel related measures
and covid-19 mortality generally reported a decrease Restricted travel and border closures
in mortality (table 2).35 38 42 A natural experiment study Border closure was assessed in one natural experiment
involving 45 US states reported a decrease in covid-19 study involving nine African countries (table 3).62
related mortality of 2.0% (95% confidence interval Overall, the countries recorded an increase in the
−3.0% to 0.9%) daily after lockdown had been made incidence of covid-19 after border closure. These
mandatory.35 A Brazilian quasi-experimental study studies concluded that the implementation of border
reported a 27.4% average difference in covid-19 related closures within African countries had minimal effect
mortality rates in the first 25 days of lockdown.42 In on the incidence of covid-19. The study had important
addition, a natural experiment study reported about limitations and was rated at serious or critical risk of
30% and 60% reductions in covid-19 related mortality bias. In the US, a natural experiment study reported that
post-lockdown in Italy and Spain over four weeks post- restrictions on travel between states contributed about
intervention, respectively.38 All three studies were 11% to a reduction in SARS-CoV-2 transmission (table
rated at moderate risk of bias (fig 2). 3).36 The study was rated at moderate risk of bias (fig 2).
Lockdown and transmission of SARS-CoV-2 Entry and exit screening (virus or symptom screening)
Four studies assessed universal lockdown and One retrospective cohort study assessed screening of
transmission of SARS-CoV-2 during the first few symptoms, which involved testing 65 000 people for
months of the pandemic (table 2). The decrease in fever (table 3).54 The study found that screening for
reproductive number (R0) ranged from 1.27 in Italy fever lacked sensitivity (ranging from 18% to 24%)
(pre-intervention 2.03, post-intervention 0.76)39 to in detecting people with SARS-CoV-2 infection. This
2.09 in India (pre-intervention 3.36, post-intervention translated to 86% of the population with SARS-CoV-2
1.27),64 and 3.97 in China (pre-intervention 4.95, post- remaining undetected when screening for fever. The
intervention 0.98).33 A natural experiment from the US study was rated at moderate risk of bias (fig 2).
the bmj | BMJ 2021;375:e068302 | doi: 10.1136/bmj-2021-068302 9RESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Table 3 | Study characteristics and main results from studies that assessed individual travel measures
Reference, Public health Outcome
country Study design measure Sample size measure Study duration Effect estimates: conclusions Risk of bias
Emeto et al,62 Natural Border closure 9 countries Rt 14 Feb-19 Jul See supplementary table for data on all countries: Serious or
Africa experiment 2020 minimal effect on reducing transmission (Rt)*† critical
Liu et al,58 Natural Interstate travel 50 states Rt 21 Jan-31 May Risk ratio 0.89 (95% confidence interval 0.84 to Moderate
USA experiment restrictions 2020 0.95): contributed about 11% to reduction in Rt*
Mitra et al,54 Retrospective Screening for fever 65 000 people Daily growth 9 Mar-13 May Sensitivity 24%: 86% of cases not detected—poor Moderate
Australia cohort rate 2020 sensitivity of identifying people with SARS-CoV-2*
R0=reproductive number; Rt=time varying reproductive number.
*Interpretation of findings as reported in the original manuscript.
†Not an effective intervention
Multiple public health measures small number of individual studies (RESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
Comparison with other studies Empirical evidence from restricted travel and
Previous literature reviews have identified mask wearing full border closures is also limited, as it is almost
as an effective measure for the containment of SARS- impossible to study these strategies as single
CoV-2103; the caveat being that more high level evidence measures. Current evidence from a recent narrative
is required to provide unequivocal support for the literature review suggested that control of movement,
effectiveness of the universal use of face masks.104 105 along with mandated quarantine, travel restrictions,
Additional empirical evidence from a recent randomised and restricting nationals from entering areas of
controlled trial (originally published as a preprint) high infection, are effective measures, but only with
indicates that mask wearing achieved a 9.3% reduction good compliance.122 A narrative literature review
in seroprevalence of symptomatic SARS-CoV-2 infection of travel bans, partial lockdowns, and quarantine
and an 11.9% reduction in the prevalence of covid-19- also suggested effectiveness of these measures,123
like symptoms.106 Another systematic review showed and another rapid review further supported travel
stronger effectiveness with the use of N95, or similar, restrictions and cross border restrictions to stop the
respirators than disposable surgical masks,107 and a spread of SARS-CoV-2.124 It was impossible to make
study evaluating the protection offered by 18 different such observations in the current review because of
types of fabric masks found substantial heterogeneity limited evidence. A German review, however, suggested
in protection, with the most effective mask being that entry, exit, and symptom screening measures to
multilayered and tight fitting.108 However, transmission prevent transmission of SARS-CoV-2 are not effective
of SARS-CoV-2 largely arises in hospital settings in which at detecting a meaningful proportion of cases,125 and
full personal protective measures are in place, which another review using real world data from multiple
suggests that when viral load is at its highest, even the countries found that border closures had minimal
best performing face masks might not provide adequate impact on the control of covid-19.126
protection.51 Additionally, most studies that assessed Although universal lockdowns have shown a
mask wearing were prone to important confounding protective effect in lowering the incidence of covid-19,
bias, which might have altered the conclusions drawn SARS-CoV-2 transmission, and covid-19 mortality,
from this review (ie, effect estimates might have been these measures are also disruptive to the psychosocial
underestimated or overestimated or can be related to and mental health of children and adolescents,127 global
other measures that were in place at the time the studies economies,128 and societies.129 Partial lockdowns
were conducted). Thus, the extent of such limitations on could be an alternative, as the associated effectiveness
the conclusions drawn remain unknown. can be high,125 especially when implemented early
A 2020 rapid review concluded that quarantine is in an outbreak,85 and such measures would be less
largely effective in reducing the incidence of covid-19 disruptive to the general population.
and covid-19 mortality. However, uncertainty over It is important to also consider numerous sociopolitical
the magnitude of such an effect still remains,109 and socioeconomic factors that have been shown to
with enhanced management of quality quarantine increase SARS-CoV-2 infection130 131 and covid-19
facilities for improved effective control of the mortality.132 Immigration status,82 economic status,81
101
epidemics urgently needed.110 In addition, findings and poverty and rurality98 can influence individual
on the application of school and workplace closures and community compliance with public health
are still inconclusive. Policy makers should be measures. Poverty can impact the ability of communities
aware of the ambiguous evidence when considering to physically distance,133 especially in crowded living
school closures, as other potentially less disruptive environments,134 135 as well as reduce access to personal
physical distancing interventions might be more protective measures.134 135 A recent study highlights
appropriate.21 Numerous findings from studies on that “a one size fits all” approach to public health
the efficacy of school closures showed that the risk measures might not be effective at reducing the spread
of transmission within the educational environment of SARS-CoV-2 in vulnerable communities136 and could
often strongly depends on the incidence of covid-19 exacerbate social and economic inequalities.135 137
in the community, and that school closures are most As such, a more nuanced and community specific
successfully associated with control of SARS-CoV-2 approach might be required. Even though screening is
transmission when other mitigation strategies are in highly recommended by WHO138 because a proportion
place in the community.111-117 School closures have of patients with covid-19 can be asymptomatic,138
been reported to be disruptive to students globally and screening for symptoms might miss a larger proportion
are likely to impair children’s social, psychological, of the population with covid-19. Hence, temperature
and educational development118 119 and to result in screening technologies might need to be reconsidered
loss of income and productivity in adults who cannot and evaluated for cost effectiveness, given such measures
work because of childcare responsibilities.120 are largely depended on symptomatic fever cases.
Speculation remains as how best to implement
physical distancing measures.121 Studies that assess Strengths and limitations of this review
physical distancing measures might interchangeably The main strength of this systematic review was the
study physical distancing with lockdown35 52 56 64 use of a comprehensive search strategy to identify and
and other measures and thus direct associations are select studies for review and thereby minimise selection
difficult to assess. bias. A clinical epidemiologist developed the search
the bmj | BMJ 2021;375:e068302 | doi: 10.1136/bmj-2021-068302 11RESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
strategy, which was validated by two senior medical covid-19. The narrative results of this review indicate
librarians. This review followed a comprehensive an effectiveness of both individual or packages of
appraisal process that is recommended by the public health measures on the transmission of SARS-
Cochrane Collaboration31 to assess the effectiveness CoV-2 and incidence of covid-19. Some of the public
of public health measures, with specifically validated health measures seem to be more stringent than
tools used to independently and individually assess others and have a greater impact on economies and
the risk of bias in each study by study design. the health of populations. When implementing public
This review has some limitations. Firstly, high quality health measures, it is important to consider specific
evidence on SARS CoV-2 and the effectiveness of public health and sociocultural needs of the communities
health measures is still limited, with most studies and to weigh the potential negative effects of the
having different underlying target variables. Secondly, public health measures against the positive effects
information provided in this review is based on current for general populations. Further research is needed to
evidence, so will be modified as additional data assess the effectiveness of public health measures after
become available, especially from more prospective adequate vaccination coverage has been achieved. It
and randomised studies. Also, we excluded studies is likely that further control of the covid-19 pandemic
that did not provide certainty over the effect measure, depends not only on high vaccination coverage and
which might have introduced selection bias and limited its effectiveness but also on ongoing adherence to
the interpretation of effectiveness. Thirdly, numerous effective and sustainable public health measures.
studies measured interventions only once and others We thank medical subject librarians Lorena Romero (LR) and Marshall
multiple times over short time frames (days v month, or Dozier (MD) for their expert advice and assistance with the study
no timeframe). Additionally, the meta-analytical portion search strategy.
of this study was limited by significant heterogeneity Contributors: ST, DG, DI, DL, and ZA conceived and designed the
study. ST, DG, SS, AM, HW, WX, JR, ET, AM, XL, XZ, and IME collected
observed across studies, which could neither be
and screened the data. ST, DG, and DI acquired, analysed, or
explored nor explained by subgroup analyses or meta- interpreted the data. ST, HW, and SS drafted the manuscript. All
regression. Finally, we quantitatively assessed only authors critically revised the manuscript for important intellectual
content.. XL and ST did the statistical analysis. NA obtained funding.
publications that reported individual measures; studies
LR and MD provided administrative, technical, or material support. ST
that assessed multiple measures simultaneously were and DI supervised the study. ST and DI had full access to all the data in
narratively analysed with a broader level of effectiveness the study and take responsibility for the integrity of the data and the
accuracy of the data analysis. ST is the guarantor. The corresponding
(see supplementary material 3, table 3). Also, we
author attests that all listed authors meet authorship criteria and that
excluded studies in languages other than English. no others meeting the criteria have been omitted.
Funding: No funding was available for this research. ET is supported
Methodological limitations of studies included in by a Cancer Research UK Career Development Fellowship (grant No
the review C31250/A22804). XZ is supported by The Darwin Trust of Edinburgh.
Several studies failed to define and assess for Competing interests: All authors have completed the ICMJE uniform
disclosure form at www.icmje.org/disclosure-of-interest/and declare: ET
potential confounders, which made it difficult is supported by a Cancer Research UK Career Development Fellowship
for our review to draw a one directional or causal and XZ is supported by The Darwin Trust of Edinburgh; no financial
conclusion. This problem was mainly because we relationships with any organisations that might have an interest in the
submitted work in the previous three years; and no other relationships
were unable to study only one intervention, given that or activities that could appear to have influenced the submitted work.
many countries implemented several public health Ethical approval: Not required.
measures simultaneously; thus it is a challenge to Data sharing: No additional data available.
disentangle the impact of individual interventions (ie, The lead author (ST) affirms that the manuscript is an honest,
physical distancing when other interventions could accurate, and transparent account of the study reported; no important
be contributing to the effect). Additionally, studies aspects of the study have been omitted. Dissemination to participants
and related patient and public communities: It is anticipated to
measured different primary outcomes and in varied disseminate the results of this research to wider community via press
ways, which limited the ability to statistically analyse release and social media platforms.
other measures and compare effectiveness. Provenance and peer review: Not commissioned; externally peer
Further pragmatic randomised controlled trials and reviewed.
natural experiment studies are needed to better inform This is an Open Access article distributed in accordance with the
Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license,
the evidence and guide the future implementation of which permits others to distribute, remix, adapt, build upon this work
public health measures. Given that most measures non-commercially, and license their derivative works on different
depend on a population’s adherence and compliance, terms, provided the original work is properly cited and the use is non-
commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
it is important to understand and consider how
these might be affected by factors. A lack of data in 1 McKee M, Stuckler D. If the world fails to protect the economy,
the assessed studies meant it was not possible to COVID-19 will damage health not just now but also in the future. Nat
Med 2020;26:640-2. doi:10.1038/s41591-020-0863-y.
understand or determine the level of compliance and 2 World Health Organization. WHO Coronavirus (COVID-19) Dashboard.
adherence to any of the measures. 2021. https://covid19.who.int/
3 Parodi SM, Liu VX. From Containment to Mitigation of COVID-19 in
the US. JAMA 2020;323:1441-2. doi:10.1001/jama.2020.3882.
Conclusions and policy implications 4 Bernal JL, Andrews N, Gower C, et al. Early effectiveness of
Current evidence from quantitative analyses indicates COVID-19 vaccination with BNT162b2 mRNA vaccine and
ChAdOx1 adenovirus vector vaccine on symptomatic disease,
a benefit associated with handwashing, mask wearing, hospitalisations and mortality in older adults in England. medRxiv
and physical distancing in reducing the incidence of 2021:2021.03.01.21252652.
12 doi: 10.1136/bmj-2021-068302 | BMJ 2021;375:e068302 | the bmjRESEARCH
BMJ: first published as 10.1136/bmj-2021-068302 on 17 November 2021. Downloaded from http://www.bmj.com/ on 27 December 2021 by guest. Protected by copyright.
5 Chodick G, Tene L, Patalon T, et al. Assessment of Effectiveness of 29 Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for
1 Dose of BNT162b2 Vaccine for SARS-CoV-2 Infection 13 to 24 assessing risk of bias in randomised trials. BMJ 2019;366:l4898.
Days After Immunization. JAMA Netw Open 2021;4:e2115985. doi:10.1136/bmj.l4898.
doi:10.1001/jamanetworkopen.2021.15985. 30 Röver C, Knapp G, Friede T. Hartung-Knapp-Sidik-Jonkman approach and
6 Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating its modification for random-effects meta-analysis with few studies. BMC
herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet Med Res Methodol 2015;15:99. doi:10.1186/s12874-015-0091-1.
2020;396:1614-6. doi:10.1016/S0140-6736(20)32318-7. 31 Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ. Welch VA, ed.
7 Khateeb J, Li Y, Zhang H. Emerging SARS-CoV-2 variants of concern Cochrane Handbook for Systematic Reviews of Interventions.: Chichester,
and potential intervention approaches. Crit Care 2021;25:244. UK: Wiley; 2019. 2nd edn. https://training.cochrane.org/handbook.
doi:10.1186/s13054-021-03662-x. 32 Vlachos J, Hertegård E, B Svaleryd H. The effects of school closures on
8 Singh J, Pandit P, McArthur AG, Banerjee A, Mossman K. Evolutionary SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A
trajectory of SARS-CoV-2 and emerging variants. Virol J 2021;18:166. 2021;118:e2020834118. doi:10.1073/pnas.2020834118.
doi:10.1186/s12985-021-01633-w. 33 Wang J, Liao Y, Wang X, et al. Incidence of novel coronavirus (2019-
9 Sanyaolu A, Okorie C, Marinkovic A, et al. The emerging SARS-CoV-2 nCoV) infection among people under home quarantine in Shenzhen,
variants of concern. Ther Adv Infect Dis 2021;8:20499361211024372. China. Travel Med Infect Dis 2020;37:101660. doi:10.1016/j.
doi:10.1177/20499361211024372. tmaid.2020.101660.
10 World Health Organization. Coronavirus disease (COVID-19): Herd 34 Al-Tawfiq JA, Sattar A, Al-Khadra H, et al. Incidence of COVID-19
immunity, lockdowns and COVID-19. 2020. www.who.int/news- among returning travelers in quarantine facilities: A longitudinal
room/q-a-detail/herd-immunity-lockdowns-and-covid-19 study and lessons learned. Travel Med Infect Dis 2020;38:101901-
11 Henry DA, Jones MA, Stehlik P, Glasziou PP. Effectiveness of 01. doi:10.1016/j.tmaid.2020.101901.
COVID-19 vaccines: findings from real world studies. Med J Aust 35 Siedner MJ, Harling G, Reynolds Z, et al. Correction: Social distancing
2021;215:149-151.e1. doi:10.5694/mja2.51182. to slow the US COVID-19 epidemic: Longitudinal pretest-posttest
12 World Health Organization. COVID-19 strategy update. 2020. www. comparison group study. PLoS Med 2020;17:e1003376.
who.int/docs/default-source/coronaviruse/covid-strategy-update- doi:10.1371/journal.pmed.1003376.
14april2020.pdf?sfvrsn=29da3ba0_19 36 Lio CF, Cheong HH, Lei CI, et al. Effectiveness of personal
13 Hollingsworth TD, Klinkenberg D, Heesterbeek H, Anderson RM. protective health behaviour against COVID-19. BMC Public Health
Mitigation strategies for pandemic influenza A: balancing conflicting 2021;21:827. doi:10.1186/s12889-021-10680-5.
policy objectives. PLoS Comput Biol 2011;7:e1001076-76. 37 Van den Berg P, Schechter-Perkins EM, Jack RS, et al. Effectiveness
doi:10.1371/journal.pcbi.1001076. of 3 Versus 6 ft of Physical Distancing for Controlling Spread of
14 Aledort JE, Lurie N, Wasserman J, Bozzette SA. Non-pharmaceutical Coronavirus Disease 2019 Among Primary and Secondary Students
public health interventions for pandemic influenza: an evaluation and Staff: A Retrospective, Statewide Cohort Study. Clin Infect Dis
of the evidence base. BMC Public Health 2007;7:208-08. 2021. doi:10.1093/cid/ciab230.
doi:10.1186/1471-2458-7-208. 38 Tobías A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic
15 World Health Organization. Non-pharmaceutical public health in Italy and Spain after one month follow up. Sci Total Environ
measures for mitigating the risk and impact of epidemic and 2020;725:138539. doi:10.1016/j.scitotenv.2020.138539.
pandemic influenza 2019. 2019. https://apps.who.int/iris/bitstream/ 39 Guzzetta G, Riccardo F, Marziano V, et al; COVID-19 Working Group,2.
handle/10665/329438/9789241516839-eng.pdf?ua=1. Impact of a Nationwide Lockdown on SARS-CoV-2 Transmissibility,
16 Yang Chan EY, Shahzada TS, Sham TST, et al. Narrative review of Italy. Emerg Infect Dis 2021;27:267. doi:10.3201/eid2701.202114.
non-pharmaceutical behavioural measures for the prevention of 40 Guo C, Chan SHT, Lin C, et al. Physical distancing implementation,
COVID-19 (SARS-CoV-2) based on the Health-EDRM framework. Br ambient temperature and Covid-19 containment: An observational
Med Bull 2020;136:46-87. doi:10.1093/bmb/ldaa030. study in the United States. Sci Total Environ 2021;789:147876.
17 Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 doi:10.1016/j.scitotenv.2021.147876.
restrictions: an analysis of countries and regions in Asia Pacific 41 Dreher N, Spiera Z, McAuley FM, et al. Policy Interventions, Social
and Europe. Lancet 2020;396:1525-34. doi:10.1016/S0140- Distancing, and SARS-CoV-2 Transmission in the United States: A
6736(20)32007-9. Retrospective State-level Analysis. Am J Med Sci 2021;361:575-84.
18 Wong MC, Huang J, Teoh J, Wong SH. Evaluation on different non- doi:10.1016/j.amjms.2021.01.007.
pharmaceutical interventions during COVID-19 pandemic: An analysis of 42 Silva L, Figueiredo Filho D, Fernandes A. The effect of lockdown
139 countries. J Infect 2020;81:e70-1. doi:10.1016/j.jinf.2020.06.044. on the COVID-19 epidemic in Brazil: evidence from an interrupted
19 Hellewell J, Abbott S, Gimma A, et al; Centre for the Mathematical time series design. Cad Saude Publica 2020;36:e00213920.
Modelling of Infectious Diseases COVID-19 Working Group. Feasibility of doi:10.1590/0102-311x00213920.
controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet 43 Krishnamachari B, Morris A, Zastrow D, Dsida A, Harper B, Santella AJ.
Glob Health 2020;8:e488-96. doi:10.1016/S2214-109X(20)30074-7 The role of mask mandates, stay at home orders and school closure
20 Mendez-Brito A, El Bcheraoui C, Pozo-Martin F. Systematic review of in curbing the COVID-19 pandemic prior to vaccination. Am J Infect
empirical studies comparing the effectiveness of non-pharmaceutical Control 2021;49:1036-42. doi:10.1016/j.ajic.2021.02.002.
interventions against COVID-19. J Infect 2021;83:281-93. 44 Iwata K, Doi A, Miyakoshi C. Was school closure effective in mitigating
doi:10.1016/j.jinf.2021.06.018. coronavirus disease 2019 (COVID-19)? Time series analysis using
21 Viner RM, Russell SJ, Croker H, et al. School closure and management Bayesian inference. Int J Infect Dis 2020;99:57-61. doi:10.1016/j.
practices during coronavirus outbreaks including COVID-19: a rapid ijid.2020.07.052.
systematic review. Lancet Child Adolesc Health 2020;4:397-404. 45 Rader B, White LF, Burns MR, et al. Mask-wearing and control of SARS-
doi:10.1016/S2352-4642(20)30095-X. CoV-2 transmission in the USA: a cross-sectional study. Lancet Digit
22 Regmi K, Lwin CM. Factors Associated with the Implementation of Health 2021;3:e148-57. doi:10.1016/S2589-7500(20)30293-4.
Non-Pharmaceutical Interventions for Reducing Coronavirus Disease 46 Pillai J, Motloba P, Motaung KSC, et al. The effect of lockdown
2019 (COVID-19): A Systematic Review. Int J Environ Res Public regulations on SARS-CoV-2 infectivity in Gauteng Province, South
Health 2021;18:4274. doi:10.3390/ijerph18084274. Africa. S Afr Med J 2020;110:1119-23. doi:10.7196/SAMJ.2020.
23 Rizvi RF, Craig KJT, Hekmat R, et al. Effectiveness of non-pharmaceutical v110i11.15222.
interventions related to social distancing on respiratory viral 47 Alimohamadi Y, Holakouie-Naieni K, Sepandi M, Taghdir M. Effect of
infectious disease outcomes: A rapid evidence-based review and Social Distancing on COVID-19 Incidence and Mortality in Iran Since
meta-analysis. SAGE Open Med 2021;9:20503121211022973. February 20 to May 13, 2020: An Interrupted Time Series Analysis.
doi:10.1177/20503121211022973. Risk Manag Healthc Policy 2020;13:1695-700. doi:10.2147/RMHP.
24 Ayouni I, Maatoug J, Dhouib W, et al. Effective public health measures S265079.
to mitigate the spread of COVID-19: a systematic review. BMC Public 48 Auger KA, Shah SS, Richardson T, et al. Association Between
Health 2021;21:1015. doi:10.1186/s12889-021-11111-1. Statewide School Closure and COVID-19 Incidence and Mortality in
25 Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred the US. JAMA 2020;324:859-70. doi:10.1001/jama.2020.14348.
reporting items for systematic reviews and meta-analyses: 49 Leffler CT, Ing E, Lykins JD, Hogan MC, McKeown CA, Grzybowski
the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. A. Association of Country-wide Coronavirus Mortality with
doi:10.1016/j.jclinepi.2009.06.005. Demographics, Testing, Lockdowns, and Public Wearing of Masks. Am
26 Holmdahl I, Buckee C. Wrong but Useful - What Covid-19 J Trop Med Hyg 2020;103:2400-11. doi:10.4269/ajtmh.20-1015.
Epidemiologic Models Can and Cannot Tell Us. N Engl J Med 50 Lyu W, Wehby GL. Community Use Of Face Masks And COVID-19:
2020;383:303-5. doi:10.1056/NEJMp2016822. Evidence From A Natural Experiment Of State Mandates In The
27 Covidence Systematic Review Software. Veritas Health Innovation, US. Health Aff (Millwood) 2020;39:1419-25. doi:10.1377/
Melbourne Australia. www.covidence.org hlthaff.2020.00818.
28 Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing 51 Cheng Y, Ma N, Witt C, et al. Face masks effectively limit the
risk of bias in non-randomised studies of interventions. BMJ probability of SARS-CoV-2 transmission. Science 2021;372:1439-
2016;355:i4919. doi:10.1136/bmj.i4919. 43. doi:10.1126/science.abg6296.
the bmj | BMJ 2021;375:e068302 | doi: 10.1136/bmj-2021-068302 13You can also read