Transcriptomic signatures in breast cancer - RSC Publishing
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
View Article Online / Journal Homepage / Table of Contents for this issue
HIGHLIGHT www.rsc.org/molecularbiosystems | Molecular BioSystems
Transcriptomic signatures in breast cancer
Jianjiang Fu and Stefanie S. Jeffrey*
DOI: 10.1039/b618163e
High throughput DNA microarray technology has been broadly applied to the
study of breast cancer to classify molecular subtypes, to predict outcome, survival,
response to treatment, and for the identification of novel therapeutic targets.
Open Access Article. Published on 05 June 2007. Downloaded on 11/17/2021 1:24:38 PM.
Although results are promising, this technology will not have a full impact on
routine clinical practice until there is further standardization of techniques and
optimal clinical trial design. Due to substantial disease heterogeneity and the
number of genes being analyzed, collaborative, multi-institutional studies are
required to accrue enough patients for sufficient statistical power. Newer
bioinformatic approaches are being developed to assist with the analysis of this
important data.
Introduction now aimed at tailoring treatment for the profiling and other ‘‘-omic’’ technologies
individual patient, known as ‘‘person- facilitate discovery of relevant signatures
Breast cancer involves a wide range of alized medicine’’.5 This requires develop- that may have an impact on prognosis
pathological entities with diverse clinical ing an accurate prognostic profile to (forecasting clinical outcome), prediction
courses. It is the most common malig- define which patients should receive (forecasting tumor response to a specific
nancy and leading cause of cancer death systemic therapy (hormone or chemo- therapy), and provide further insights
among American women between the therapy) before and/or after surgery, into tumor biology,6,7 informing both the
ages 20 to 59 and the second cause of and to decide which systemic treatments clinician and the scientist.
cancer death in women aged 60 to 79.1 In are most suitable for a given patient.
the UK and US, breast cancer mortality The recent development of DNA Molecular classification by
is declining,2 attributed to the implemen- microarray and related technologies
tation of widespread screening mammo- gene expression profiling
provides an opportunity to perform
graphy, earlier diagnosis, and advances more detailed and individualized tumor Using DNA microarrays, breast cancer
in adjuvant treatment.3 Treatment deci- characterization. heterogeneity has been confirmed at the
sions are usually made according to Microarray technology, with its ability gene expression level.8 Multiple breast
general guidelines,4 but not all patients to simultaneously analyze tens of cancer subtypes with distinct gene
benefit from their treatment. Efforts are thousands genes, has transformed our expression patterns and different pro-
understanding of human breast cancer. gnoses have been identified in primary
Stanford University Medical Center, MSLS Previous classification systems histori- breast cancers and their metastases. A
Building, Room P214, 1201 Welch Road, M/C cally relied on light microscopic findings Stanford–Norway collaborative research
5494, Stanford, CA, USA 94305-5494.
E-mail: ssj@stanford.edu; and single marker-tumor features (e.g. program revealed that breast cancers can
Fax: +1 650-724-3229; Tel: +1 650-723-0799 estrogen receptor, ER). Expression be classified into five or six distinct
Jianjiang Fu, PhD, graduated her medical and postgraduate
from China Pharmaceutical training at the University of
University with a BS degree. California, San Francisco. Dr
He earned his PhD from the Jeffrey is Associate Professor of
Institute of Materia Medica at Surgery at Stanford University
Peking Union Medical College School of Medicine and the
as a pharmacologist specializing John and Marva Warnock
in tumor pharmacology. Dr Fu Faculty Scholar in Cancer
is a postdoctoral research fellow Research. She was a key mem-
in the Jeffrey lab at Stanford ber of the Stanford–Norway
University School of Medicine. team that pioneered the use of
His current interest is in the DNA microarrays to study
genomic characterization of breast cancer. Her lab is now
circulating tumor cells and developing and applying novel
Jianjiang Fu metastases in breast cancer. Stefanie S. Jeffrey technologies for the study of
circulating tumor cells and can-
Stefanie S. Jeffrey, MD, graduated from Harvard University with cer metastases.
an AB in Chemistry and Physics and an MA in Chemistry. She did
466 | Mol. BioSyst., 2007, 3, 466–472 This journal is ß The Royal Society of Chemistry 2007View Article Online
immunohistochemical protein markers
(e.g. ER, PR, HER2, HER1/EGFR,
basal cytokeratins).22 Recently, the lumi-
nal A and basal-like subtypes have been
analyzed and validated on three different
microarray platforms.23 In addition to
previously identified genes, signatures
revealed distinct biological pathways:
luminal A tumors expressed genes
involved in fatty acid metabolism and
Open Access Article. Published on 05 June 2007. Downloaded on 11/17/2021 1:24:38 PM.
steroid hormone-mediated signaling;
basal-like tumors expressed cell prolif-
eration and differentiation genes and
pathway genes involved in p21-mediated
and G1-S checkpoint signaling. A possi-
ble new subtype characterized by high
expression of interferon (IFN)-regulated
genes has been identified and linked
to lymph node metastasis and poor
prognosis.16
Using a novel approach and combined
data from 599 microarrays, Kapp et al.24
present evidence in support of the
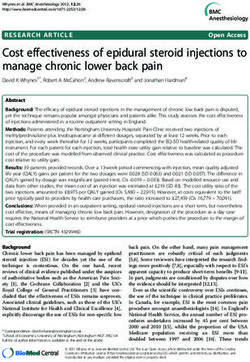
Fig. 1 Expression profiles of 119 breast cancers and 16 normal tissues. Tumors cluster into most consistently identifiable subtypes:
defined molecular subtypes. ESR1+/ERBB22, ESR2/ERBB22,
ERBB2+. Different sets of gene pairs
molecular subtypes based their microar- express genes characteristic of breast were considered, statistically validated,
ray expression data and this result has basal epithelial cells, including strong and compared to clinical outcome.
been established in other datasets world- expression of basal cytokeratins 5, 6 Tumors described by Sorlie centroids
wide9–17 (Fig. 1). and 17. These tumors show high expres- were generally grouped into expected
Perou et al.10 originally showed that sion of proliferation/cell cycle-related categories (luminals were ESR+/
breast tumor samples separate into two genes, lack ER and ER-related genes, ERBB22; basals were ESR2/ERBB22;
groups defined by ER status. Tumors in show low ERBB2 (HER2/neu) expres- and ERBB2-overexpressing tumors were
the ER-positive group have expression sion; and show low expression of BRCA1 mainly ERBB2+ subtype).
patterns reminiscent of the luminal protein.19,20 In addition, basal-like
epithelial cells of the breast, expressing tumors usually have aggressive features Outcome prediction by gene
luminal cytokeratins 8/18, ER (ESR1) such high tumor grade and TP53 muta- expression profiling
and genes associated with ER overex- tions.11,18,21 The ERBB2-overexpressing
pression such as GATA3 and NAT1. subtype is characterized by overexpres- Metastases are the main cause of death in
There are at least two subtypes of ER- sion of genes in a 17q amplicon that breast cancer patients, and improving the
positive tumors,11 luminal A and luminal include ERBB2 and GRB7. Like the means of foretelling their development is
B (we now term the luminal B group basal-like subtype, ERBB2-overexpres- a major goal of current clinical
‘‘highly proliferating luminals’’).18 These sing tumors have a high proportion of research.25–30 Genomic-based tests pre-
two hormone receptor-overexpressing TP53 mutations,11,18,21 and are signifi- dicting the likelihood of tumor recur-
tumor classes are distinguished by gene cantly more likely to be grade III.21 rence provide information about the
expression patterns and markedly differ- Finally, a normal breast-like subtype molecular biology of metastasis and
ent clinical outcomes. Luminal A tumors was identified that has some character- provide a gauge of outcome prediction
have, in general, the highest expression of istics in common with normal breast for new cases.7–9,13,31–40
ER and ER-related genes. Luminal B tissue, including adipose and other non- A 70-gene prognosis signature was
tumors show expression of luminal/ER- epithelial tissue components of the tumor developed by van’t Veer31 et al. In this
related genes, but are further distin- microenvironment. These tumors, like study, the investigators selected 78 lymph
guished by relatively high expression of normal breast tissue, show relative over- node-negative patients, with primary
proliferation and cell cycle-related genes. expression of basal epithelial genes and sporadic breast cancer, who were less
Conversely, hormone receptor nega- relative underexpression of luminal than 55 years old; expression profiles
tive breast cancers comprise two distinct epithelial genes. Invasive lobular breast were compared between 34 patients who
subtypes, ERBB2-overexpressing and cancers often show normal-like expres- developed distant metastasis within
basal-like, that differ in biology and sion profiles.11,12 5 years and 44 patients who remained
behavior; both show comparatively poor The distinct subtypes of breast disease-free for at least 5 years. ER status
outcomes. Basal-like tumors highly cancer have also been characterized by and other clinical variables were not
This journal is ß The Royal Society of Chemistry 2007 Mol. BioSyst., 2007, 3, 466–472 | 467View Article Online
considered when the molecular predictor signature would have potentially spared Histological grading of breast cancer
was developed. A 70-gene marker set was as many as 40% of node-negative provides clinically important prognostic
developed to classify tumors into good patients for whom chemotherapy would information.56–59 Gene expression profil-
and poor prognosis groups. Not surpris- have been recommended.44 This signa- ing of tumors having different histologi-
ingly, genes significantly up-regulated in ture also warrants prospective testing in cal grades is under study. Ma et al.
the poor prognosis signature included larger clinical trials. However, as many created distinct low grade (grade I) and
those involved in cell cycle, invasion and clinicians know, ER-positive patients high grade (grade III) signatures based
metastasis, angiogenesis, and signal may relapse distantly 8 or more years on laser microdissection and DNA
transduction. This 70-gene signature has after diagnosis, so 5 year follow-up microarrays.60 Sotiriou et al.61 identified
been validated in larger series.32 The may be too short a time interval for a 97-gene signature that they designate
Open Access Article. Published on 05 June 2007. Downloaded on 11/17/2021 1:24:38 PM.
largest series evaluated 302 multi-institu- distinguishing good vs. poor prognostic the gene expression grade index (GGI).
tional tumor samples from 403 node- signatures, particularly for patients of This was comprised mainly of genes
negative women, who were less than 60 years or less.45–48 involved in cell cycle regulation and
61 years old and who did not receive Hypoxia (low oxygen) is clinically proliferation. Based on this signature,
systemic therapy, and found that the 70- recognized as an important determinant intermediate grade (grade II) tumors
gene signature added independent prog- of metastasis and poor patient outcome were subdivided into two groups with
nostic information to conventionally of breast cancer.49,50 Chi et al. analyzed high and low risks of recurrence, demon-
used prognostic criteria, although it differential expression in global tran- strating that the GGI may be used to
did not perform as well in this script levels in response to hypoxia in classify intermediate grade tumors more
larger trial with longer clinical follow- primary epithelial cells, including renal accurately.62 More recently, a group
up.41 Commercially available on the proximal tubule epithelial cells, normal from the Genome Institute of Singapore
MammaPrint1 array (Agendia BV, breast epithelial cells, and endothelial reported six genes highlighted from 264
Amsterdam, The Netherlands), the 70- cells. This gene expression signature was grade-associated genes identified by the
gene profile will be prospectively proposed to serve as a measure of expression profiles of 347 primary inva-
compared to a clinical-pathological hypoxia response activation in different sive breast cancers. These six genes were
prognostic tool (Adjuvant! Online) in human cancers, and to provide clinical able to subdivide high and low grade
selecting approximately 6000 node- outcome prediction in breast cancer.51 tumors and also classify intermediate
negative patients for adjuvant chemo- Furthermore, when lysyl oxidase (LOX), grade tumors into two distinct subtypes,
therapy in the microarray in node an extracellular matrix enzyme up- termed G2a and G2b, which possessed
negative disease may avoid chemother- regulated by hypoxia, is overexpressed similar, but not identical, clinical out-
apy (MINDACT, http://www.eortc.be/ in human tumors, it is associated with come to grade I and grade III tumors,
services/unit/mindact/) trial from the poorer distant metastasis-free and overall respectively.63
European Organization for Research survival in ER-negative breast cancer Metastases to sites distant from the
and Treatment of Cancer.42 patients, and LOX inhibition eliminates breast may contain tissue-specific expres-
A different prognostic signature based metastasis formation in a model sion profiles. Breast cancer most com-
on a different array platform was system.50,52 Given that cancer invasion monly spreads to bone marrow, lung,
recently published by Wang et al., speci- and metastasis possess many histological liver, brain, and adrenal gland.64,65
fying 76 genes (60 genes for ER-positive similarities and may parallel some Discovering genes that are functionally
and 16 genes for ER-negative breast cellular behaviors of normal wound important for tissue-specific metastasis
tumors) that distinguished lymph node- healing,53,54 Chang et al. identified a could help explain underlying tissue-
negative patients who developed distant 677-gene signature based on gene expres- tropism.66 Using the MDA-MB-231
metastases within five years.33 This pro- sion profiles of fibroblasts from ten human breast cancer cell line as a model
file was found to be applicable to both anatomic sites in response to serum system, Kang and Minn et al.67,68 identi-
pre- and postmenopausal patients and exposure, which seems to represent the fied a gene set that acted cooperatively to
patients with 10–20 mm tumors, an role of fibroblasts in wound healing.55 cause osteolytic metastasis. Analyzing
especially common but not well-studied More recently, the reproducibility of the this cell line-derived bone profile in
group. The genes in this prognostic association between this serum-response 25 primary breast tumors, there was
signature belonged to many functional gene expression signature and breast 67% sensitivity and 80% specificity for
classes, including cell death, cell cycle cancer progress was examined on a developing bone-only metastases in
and proliferation, transcriptional regula- database of 295 breast cancer patients, patients. An 86-gene bone metastatic
tion, immune response, and growth, which also had been used to identify signature was identified by Woelfle and
suggesting that different pathways can and validate a 70-gene profile.31,32 colleagues between tumors from BM-
influence disease progression.33,43 A The results revealed that not only positive and BM-negative patients. This
multi-center trial testing this signature distant metastasis-free survival but also gene set was mainly characterized by
on a separate group of 180 breast tumors overall survival was strikingly reduced transcriptional repression genes and
verified it as a strong predictor for in patients whose tumors expressed requires validation in a different data
remaining distant metastasis-free at this serum-response signature compared set.69 Smid et al. reported that 69 genes
5 years. Moreover, comparing it to to tumors that did not express the may be involved in bone metastasis based
conventionally-used criteria, use of the signature.34,35 on 107 primary breast tumors in patients
468 | Mol. BioSyst., 2007, 3, 466–472 This journal is ß The Royal Society of Chemistry 2007View Article Online
who all were lymph node-negative at the high-throughput reverse transcriptase microarrays to analyze the gene expres-
time of diagnosis and who experienced polymerase chain reaction technique.78 sion profiling of oncogene and tumor-
relapse in the bone and other organs.69,70 They developed an 85-gene classifier for suppressor gene regulated pathways.86–88
They found that bone-only metastases partial or complete response, which was In each case, they identified a signature
involved the fibroblast growth factor validated in an additional 26 patients. that represented the activated status of
receptor-MAPK pathway. A study ana- Two groups, one from Baylor College of each oncogenic pathway. In addition to
logous to Kang’s report described a lung Medicine and the other from Millennium successfully predicting the activation
metastasis profile for breast cancer.72 A Pharmaceuticals and the M. D. status of each of the pathways in a range
95-gene set was identified and reduced Anderson Cancer Center, have used of human and mouse tumors, oncogenic
to 54 candidate genes by requiring microarrays to study the response of pathway activation predicted the in vitro
Open Access Article. Published on 05 June 2007. Downloaded on 11/17/2021 1:24:38 PM.
that these genes also be differentially locally advanced breast cancers to pri- sensitivity of a broad range of human
expressed across multiple independent mary chemotherapy in 30 and 42 patients, tumor cell lines to drugs targeting spe-
lung-metastatic clones of breast cancer respectively.79–82 Multi-gene predictors cific pathways. The analysis of oncogenic
cell lines. The 54-gene signature was of response were generated. These pathway signatures may offer guidance
validated in a cohort of 82 breast cancer included a 92-gene list that initially in the appropriate selection of tumor-
patients with a 10 year follow-up, and predicted at least 75% tumor regression specific combination therapies—multiple
appeared to be a strong clinical predictor in response to four cycles of docetaxol in drugs that target multiple pathways—
for lung selective metastasis.72 The ability 24 patients, which was validated in an based on information specifying the
to predict site-specific metastasis based independent set of six patients. However, activation state of these pathways.
TM
on gene expression profiling of a primary further analysis of residual tumors after Oncotype DX is a commercial clini-
tumor may permit targeted therapeutic three months of docetaxel treatment, cally-validated multi-gene assay that
intervention and could help increase revealed the residual cells had similar provides a quantitative assessment of
patient survival. expression profiles to those that the likelihood of distant breast cancer
were initially resistant. Differentially recurrence in lymph node-negative, ER-
Gene expression profiling for expressed genes between initially sensi- positive breast cancer and also assesses
prediction of response to tive and ultimately docetaxel-resistant the benefit from adjuvant chemotherapy
cells included those involved in cell cycle in these patients. This 21-gene signature
treatments
arrest at G2/M, fatty acid/phospholipid was established based on the paraffin-
Breast cancer is among the most sensitive metabolism or the mammalian target of embedded tumor tissue from tamoxifen-
to chemotherapy compared to other solid rapamycin (mTOR) survival pathway treated patients89–94 and was shown to
tumors. Systemic therapy for breast that involves vesicular trafficking, predict risk for distant recurrence or
cancer includes hormonal therapy, chem- oxidative bursts, and protein/organelle death in several independent studies.
otherapy, and novel agents.5 Several metabolism.83 A separate 74-gene list Studying similar tumors, another signa-
single agent and combination chemother- predicting pathologic complete response ture, the HOXB13 : IL17BR expression
apy regimens are effective treatments for to sequential weekly paclitaxel and ratio was identified and confirmed to
breast cancer, such as cyclophosphamide, fluorouracil + doxorubicin + cyclopho- predict survival and recurrence in tamox-
doxorubicin, 5-fluorouracil (5-FU) and sphamide (T/FAC) neoadjuvant chemo- ifen-treated patients with ER-positive
taxanes.5 In clinical practice, chemother- therapy in 24 patients was independently node-negative breast cancer.95–97 In a
apy is applied empirically despite the fact validated in an additional 18 patients. different study, Jansen and colleagues
that not all patients benefit from those Another group from Germany reported a identified genes that predicted response
agents. Hence, there is a need to identify 512-gene signature, enriched for genes to tamoxifen in recurrent ER-positive
predictive biomarkers for its efficacy. involved in transforming growth factor- breast carcinomas.98 Golub’s group
Currently, with the recent technological beta and RAS-mediated signaling path- recently described a ‘‘connectivity
advances, it is anticipated that gene ways, to predict pathologic complete map’’ linking bioactive small-molecule
expression profiling in predicting efficacy response to primary systemic therapy perturbagens, gene signatures, and dis-
and safety of breast cancer treatment with gemcitabine, epirubicin, and doce- ease states based on DNA microarray
may allow the definition of a pattern of taxel.84 Although all groups reported an assessment.99
clinically useful discriminatory gene association between gene expression pro-
expression. file and treatment outcome, the predic-
Limitation and prospects
Taxanes are a class of antimicrotubule tive power was too low for current
agents that are proven to be effective and clinical use and larger validation studies DNA microarray analysis has been
are routinely used in multidrug therapy are underway or planned. shown to be a powerful tool in uncover-
of primary and advanced breast can- Huang et al. established several gene ing the mechanistic insights into tumor
cers.73–77 Several groups have analyzed expression phenotypic models controlled biology. It is being used to study almost
the gene expression profiles of patients by oncogenes, such as HRAS, MYC and all the aspects of cancer biology, from
that may benefit from taxane therapy. E2Fs, and applied microarrays to analyze diagnosis to prognosis to drug responses,
A Japanese group studied 44 primary regulatory pathways that predicted and for the development of new antic-
or locally recurrent breast cancers oncogenic phenotypes.85 More recently, ancer agents. It provides opportunities
treated with docetaxel using a 2453-gene Bild et al. from the same group used for more detailed characterization of
This journal is ß The Royal Society of Chemistry 2007 Mol. BioSyst., 2007, 3, 466–472 | 469View Article Online
cancer biology and impacts on our 5 V. Stearns, N. E. Davidson and T. Ikdahl, R. Kåresen, A.-L. Børresen-
D. A. Flockhart, Pharmacogenomics J., Dale and S. S. Jeffrey, Breast Cancer
understanding of malignant diseases. 2004, 4, 143–153. Res., 2007, 9(R30), DOI: 101186/bcr1675.
While reports of DNA microarray 6 S. S. Jeffrey, M. J. Fero, A. L. Borresen- 19 D. M. Abd El-Rehim, G. Ball, S. E.
studies in oncology are exciting, the use Dale and D. Botstein, Mol. Interventions, Pinder, E. Rakha, C. Paish, J. F.
of this technology has not yet been 2002, 2, 101–109. Robertson, D. Macmillan, R. W. Blamey
7 V. A. Funari and S. S. Jeffrey, in and I. O. Ellis, Int. J. Cancer, 2005, 116,
implemented clinically. Different signa- Advanced therapy of breast disease, ed. 340–350.
tures are reported by different studies of S. E. Singletary, G. L. Robb and G. N. 20 N. Turner, A. Tutt and A. Ashworth,
the same disease,100–104 resulting in clas- Hortobagyi, B. C. Decker, Hamilton, Nat. Rev. Cancer, 2004, 4, 814–819.
Ontario, Canada, 2nd edn, 2004, ch. 8, 21 L. A. Carey, C. M. Perou, C. A. Livasy,
sifiers with little overlap between pp 845–858. L. G. Dressler, D. Cowan, K. Conway,
predictive gene lists for the same 8 S. S. Jeffrey, P. E. Lonning and G. Karaca, M. A. Troester, C. K. Tse,
Open Access Article. Published on 05 June 2007. Downloaded on 11/17/2021 1:24:38 PM.
cancer,103–106 even when the same micro- B. E. Hillner, J. Natl. Compr. Cancer S. Edmiston, S. L. Deming, J. Geradts,
array platform is used. Among the many Network, 2005, 3, 291–300. M. C. Cheang, T. O. Nielsen, P. G.
9 C. M. Perou, S. S. Jeffrey, M. van de Moorman, H. S. Earp and R. C. Millikan,
limitations to deriving a stable molecular Rijn, C. A. Rees, M. B. Eisen, D. T. Ross, JAMA, J. Am. Med. Assoc., 2006, 295,
predictor for new cases of breast cancer is A. Pergamenschikov, C. F. Williams, 2492–2502.
variability in technique platform,105 S. X. Zhu, J. C. Lee, D. Lashkari, 22 T. O. Nielsen, F. D. Hsu, K. Jensen,
D. Shalon, P. O. Brown and D. Botstein, M. Cheang, G. Karaca, Z. Hu,
sample size,107,108 patient selection Proc. Natl. Acad. Sci. U. S. A., 1999, 96, T. Hernandez-Boussard, C. Livasy,
criteria,40–42,109 statistical methods of 9212–9217. D. Cowan, L. Dressler, L. A. Akslen,
data analysis,110 noise and bias analy- 10 C. M. Perou, T. Sorlie, M. B. Eisen, J. Ragaz, A. M. Gown, C. B. Gilks,
sis,111 and prediction rules. In most M. van de Rijn, S. S. Jeffrey, C. A. Rees, M. van de Rijn and C. M. Perou, Clin.
J. R. Pollack, D. T. Ross, H. Johnsen, Cancer Res., 2004, 10, 5367–5374.
studies, the sample size (number of L. A. Akslen, O. Fluge, 23 T. Sorlie, Y. Wang, C. Xiao, H. Johnsen,
tumors assayed) is an order of magnitude A. Pergamenschikov, C. Williams, S. X. B. Naume, R. R. Samaha and A. L.
smaller than the number of genes ana- Zhu, P. E. Lonning, A. L. Borresen-Dale, Borresen-Dale, BMC Genomics, 2006, 7,
P. O. Brown and D. Botstein, Nature, 127.
lyzed, leading to a lack of statistical 2000, 406, 747–752. 24 A. V. Kapp, S. S. Jeffrey, A. Langerød,
power. Moreover, when large numbers 11 T. Sorlie, C. M. Perou, R. Tibshirani, A. Børresen-Dale, W. Han, D. Noh,
of genes are analyzed, traditional T. Aas, S. Geisler, H. Johnsen, T. Hastie, I. Bukholm, M. Nicolau, P. O. Brown
approaches to multiple hypothesis M. B. Eisen, M. van de Rijn, S. S. Jeffrey, and R. Tibshirani, BMC Genomics, 2006,
T. Thorsen, H. Quist, J. C. Matese, 7, 231; (Erratum in: BMC Genomics,
correction are too conservative, finding P. O. Brown, D. Botstein, P. E. Lonning 2007, 8(1), 101).
few if any significant genes; alternative and A. L. Borresen-Dale, Proc. Natl. 25 I. J. Fidler, Nat. Rev. Cancer, 2003, 3,
approaches use permutation methods to A c ad . S c i. U. S . A. , 2 0 01 , 9 8 , 453–458.
10869–10874. 26 A. F. Chambers, A. C. Groom and
estimate false discovery rates.112 Other 12 T. Sorlie, R. Tibshirani, J. Parker, I. C. MacDonald, Nat. Rev. Cancer,
approaches involve the use of gene sets to T. Hastie, J. S. Marron, A. Nobel, 2002, 2, 563–572.
scale down the numbers of genes being S. Deng, H. Johnsen, R. Pesich, 27 D. Tarin, J. E. Price, M. G. Kettlewell,
tested and using the biological strength S. Geisler, J. Demeter, C. M. Perou, R. G. Souter, A. C. Vass and B. Crossley,
P. E. Lonning, P. O. Brown, A. L. Br. Med. J. (Clin. Res. Ed.)., 1984, 288,
across a gene set to increase statistical Borresen-Dale and D. Botstein, Proc. 749–751.
power,113,114 or using mathematical mod- Natl. Acad. Sci. U. S. A., 2003, 100, 28 D. Tarin, A. C. Vass, M. G. Kettlewell
eling to determine only the pathological 8418–8423. and J. E. Price, Invasion Metastasis, 1984,
13 C. Sotiriou, S. Y. Neo, L. M. McShane, 4, 1–12.
component of high dimensional data.115 E. L. Korn, P. M. Long, A. Jazaeri, 29 I. J. Fidler, J. Natl. Cancer Inst., 1970, 45,
Because of the molecular heterogeneity P. Martiat, S. B. Fox, A. L. Harris and 773–782.
of breast cancer, future large-scale clin- E. T. Liu, Proc. Natl. Acad. Sci. U. S. A., 30 M. D. Cameron, E. E. Schmidt,
ical validation trials will, by necessity, be 2003, 100, 10393–10398. N. Kerkvliet, K. V. Nadkarni, V. L.
14 K. Yu, C. H. Lee, P. H. Tan, G. S. Hong, Morris, A. C. Groom, A. F. Chambers
collaborative and multi-institutional. S. B. Wee, C. Y. Wong and P. Tan, and I. C. MacDonald, Cancer Res., 2000,
They must be guided by sound trial Cancer Res., 2004, 64, 2962–2968. 60, 2541–2546.
design and use analytic methods that 15 K. Yu, C. H. Lee, P. H. Tan and P. Tan, 31 L. J. van’t Veer, H. Dai, M. J. van de
Clin. Cancer Res., 2004, 10, 5508–5517. Vijver, Y. D. He, A. A. Hart, M. Mao,
incorporate developed rules of evi-
16 Z. Hu, C. Fan, D. S. Oh, J. S. Marron, H. L. Peterse, K. van der Kooy,
dence116 prior to their acceptance into X. He, B. F. Qaqish, C. Livasy, M. J. Marton, A. T. Witteveen,
routine clinical practice. L. A. Carey, E. Reynolds, L. Dressler, G. J. Schreiber, R. M. Kerkhoven,
A. Nobel, J. Parker, M. G. Ewend, C. Roberts, P. S. Linsley, R. Bernards
L. R. Sawyer, J. Wu, Y. Liu, R. Nanda, and S. H. Friend, Nature, 2002, 415,
References M. Tretiakova, A. R. Orrico, D. Dreher, 530–536.
J. P. Palazzo, L. Perreard, E. Nelson, 32 M. J. van de Vijver, Y. D. He, L. J. van’t
1 A. Jemal, R. Siegel, E. Ward, T. Murray, M. Mone, H. Hansen, M. Mullins, Veer, H. Dai, A. A. Hart, D. W. Voskuil,
J. Xu, C. Smigal and M. J. Thun, Ca J. F. Quackenbush, M. J. Ellis, G. J. Schreiber, J. L. Peterse, C. Roberts,
Cancer J. Clin., 2006, 56, 106–130. O. I. Olopade, P. S. Bernard and M. J. Marton, M. Parrish, D. Atsma,
2 R. Peto, J. Boreham, M. Clarke, C. M. Perou, BMC Genomics, 2006, 7, 96. A. Witteveen, A. Glas, L. Delahaye,
C. Davies and V. Beral, Lancet, 2000, 17 S. H. Cheng, C. F. Horng, M. West, T. van der Velde, H. Bartelink,
355, 1822. E. Huang, J. Pittman, M. H. Tsou, S. Rodenhuis, E. T. Rutgers, S. H. Friend
3 Early Breast Cancer Trialists’ Collabo- H. Dressman, C. M. Chen, S. Y. Tsai, and R. Bernards, New Engl. J. Med.,
rative Group (EBCTCG), Lancet, 2005, J. J. Jian, M. C. Liu, J. R. Nevins and 2002, 347, 1999–2009.
365, 1687–1717. A. T. Huang, J. Clin. Oncol., 2006, 24, 33 Y. Wang, J. G. Klijn, Y. Zhang,
4 R. W. Carlson and B. McCormick, 4594–4602. A. M. Sieuwerts, M. P. Look, F. Yang,
J. Natl. Compr. Cancer Network, 2005, 18 A. Langerød, H. Zhao, Ø. Borgen, D. Talantov, M. Timmermans, M. E.
3, S7–S11. J. M. Nesland, I. R. K. Bukholm, Meijer-van Gelder, J. Yu, T. Jatkoe,
470 | Mol. BioSyst., 2007, 3, 466–472 This journal is ß The Royal Society of Chemistry 2007View Article Online
E. M. Berns, D. Atkins and J. A. 53 H. F. Dvorak, New Engl. J. Med., 1986, 72 A. J. Minn, G. P. Gupta, P. M. Siegel,
Foekens, Lancet, 2005, 365, 671–679. 315, 1650–1659. P. D. Bos, W. Shu, D. D. Giri, A. Viale,
34 H. Y. Chang, D. S. Nuyten, J. B. 54 M. J. Bissell and D. Radisky, Nat. Rev. A. B. Olshen, W. L. Gerald and
Sneddon, T. Hastie, R. Tibshirani, Cancer, 2001, 1, 46–54. J. Massague, Nature, 2005, 436, 518–524.
T. Sorlie, H. Dai, Y. D. He, L. J. van’t 55 H. Y. Chang, J. B. Sneddon, A. A. 73 B. Fisher, J. Bryant, N. Wolmark,
Veer, H. Bartelink, M. van de Rijn, Alizadeh, R. Sood, R. B. West, E. Mamounas, A. Brown, E. R. Fisher,
P. O. Brown and M. J. van de Vijver, K. Montgomery, J. T. Chi, M. van de D . L . W i c k e r h am , M . B e g o v i c ,
Proc. Natl. Acad. Sci. U. S. A., 2005, 102, Rijn, D. Botstein and P. O. Brown, PLoS A. DeCillis, A. Robidoux, R. G.
3738–3743. Biol., 2004, 2, E7. Margolese, A. B. Cruz, J. L. Hoehn,
35 E. T. Liu, Proc. Natl. Acad. Sci. U. S. A., 56 C. W. Elston and I. O. Ellis, A. W. Lees, N. V. Dimitrov and H. D.
2005, 102, 3531–3532. Histopathology, 1991, 19, 403–410. Bear, J. Clin. Oncol., 1998, 16,
36 B. E. Hillner, ACP J. Club, 2003, 138, 82. 57 C. W. Elston and I. O. Ellis, 2672–2685.
37 G. Sauter and R. Simon, New Engl. Histopathology, 2002, 41, 151. 74 E. Rivera, F. A. Holmes, D. Frye,
Open Access Article. Published on 05 June 2007. Downloaded on 11/17/2021 1:24:38 PM.
J. Med., 2002, 347, 1995–1996. 58 M. H. Galea, R. W. Blamey, C. E. Elston V. Valero, R. L. Theriault, D. Booser,
38 A. Kallioniemi, New Engl. J. Med., 2002, and I. O. Ellis, Breast Cancer Res. Treat., R. Walters, A. U. Buzdar, K. Dhingra,
347, 2067–2068. 1992, 22, 207–219. G. Fraschini and G. N. Hortobagyi,
39 B. Weigelt, A. M. Glas, L. F. Wessels, 59 J. Brown, M. Jones and E. A. Benson, Cancer (N. Y., NY, U. S.), 2000, 89,
A. T. Witteveen, J. L. Peterse and Breast Cancer Res. Treat., 1993, 25, 283. 2195–2201.
L. J. van’t Veer, Proc. Natl. Acad. Sci. 60 X. J. Ma, R. Salunga, J. T. Tuggle, 75 N. Wolmark, J. Wang, E. Mamounas,
U. S. A., 2003, 100, 15901–15905. J. Gaudet, E. Enright, P. McQuary, J. Bryant and B. Fisher, J. Natl. Cancer
40 K. Mikhitarian, W. E. Gillanders, J. S. T. Payette, M. Pistone, K. Stecker, Inst. Monogr., 2001, 30, 96–102.
Almeida, R. H. Martin, J. C. Varela, B. M. Zhang, Y. X. Zhou, H. Varnholt, 76 A. K. Nowak, N. R. Wilcken, M. R.
J. S. Metcalf, D. J. Cole and M. Mitas, B. Smith, M. Gadd, E. Chatfield, Stockler, A. Hamilton and D. Ghersi,
Clin. Cancer Res., 2005, 11, 3697–3704. J. Kessler, T. M. Baer, M. G. Erlander Lancet Oncol., 2004, 5, 372–380.
41 M. Buyse, S. Loi, L. van’t Veer, G. Viale, and D. C. Sgroi, Proc. Natl. Acad. Sci. 77 R. W. Carlson, E. Brown, H. J. Burstein,
M. Delorenzi, A. M. Glas, M. S. U. S. A., 2003, 100, 5974–5979. W. J. Gradishar, C. A. Hudis,
d’Assignies, J. Bergh, R. Lidereau, 61 C. Sotiriou, P. Wirapati, S. Loi, A. Harris, C. Loprinzi, E. P. Mamounas, E. A.
P. Ellis, A. Harris, J. Bogaerts, S. Fox, J. Smeds, H. Nordgren, Perez, K. Pritchard, P. Ravdin, A. Recht,
P. Therasse, A. Floore, M. Amakrane, P. Farmer, V. Praz, B. Haibe-Kains, G. Somlo, R. L. Theriault, E. P. Winer
F. Piette, E. Rutgers, C. Sotiriou, C. Desmedt, D. Larsimont, F. Cardoso, and A. C. Wolff, (National
H. Peterse, D. Nuyten, M. Buyse, Comprehensive Cancer Network),
F. Cardoso and M. J. Piccart, J. Natl.
M. J. Van de Vijver, J. Bergh, M. Piccart J. Natl. Compr. Cancer Network, 2006,
Cancer Inst., 2006, 98, 1183–1192.
and M. Delorenzi, J. Natl. Cancer Inst., 4, S1–S26.
42 R. Simon, J. Natl. Cancer Inst., 2006, 98,
2006, 98, 262–272. 78 K. Iwao-Koizumi, R. Matoba, N. Ueno,
1169–1171.
62 C. Desmedt and C. Sotiriou, Cell Cycle, S. J. Kim, A. Ando, Y. Miyoshi,
43 T. K. Jenssen and E. Hovig, Lancet, 2005,
2006, 5, 2198–2202. E. Maeda, S. Noguchi and K. Kato,
365, 634–635.
63 A. V. Ivshina, J. George, O. Senko, J. Clin. Oncol., 2005, 23, 422–431.
44 J. A. Foekens, D. Atkins, Y. Zhang,
B. Mow, T. C. Putti, J. Smeds, 79 J. C. Chang, E. C. Wooten, A. Tsimelzon,
F. C. Sweep, N. Harbeck, A. Paradiso,
T. Lindahl, Y. Pawitan, P. Hall, S. G. Hilsenbeck, M. C. Gutierrez,
T. Cufer, A. M. Sieuwerts, D. Talantov, R. Elledge, S. Mohsin, C. K. Osborne,
H. Nordgren, J. E. Wong, E. T. Liu,
P. N. Span, V. C. Tjan-Heijnen, A. F. G. C. Chamness, D. C. Allred and
J. Bergh, V. A. Kuznetsov and
Zito, K. Specht, H. Hoefler, R. Golouh, L. D. Miller, Cancer Res., 2006, 66, P. O’Connell, Lancet, 2003, 362, 362–369.
F. Schittulli, M. Schmitt, L. V. Beex, 10292–10301. 80 J. D. Brenton and C. Caldas, Lancet,
J. G. Klijn and Y. Wang, J. Clin. Oncol., 2003, 362, 340–341.
64 S. P. Leong, B. Cady, D. M. Jablons,
2006, 24, 1665–1671. J. Garcia-Aguilar, D. Reintgen, J. Jakub, 81 M. Ayers, W. F. Symmans, J. Stec,
45 V. R. Grann, A. B. Troxel, N. J. Zojwalla, S. Pendas, L. Duhaime, R. Cassell, A. I. Damokosh, E. Clark, K. Hess,
J. S. Jacobson, D. Hershman and M. Gardner, R. Giuliano, V. Archie, M. Lecocke, J. Metivier, D. Booser,
A. I. Neugut, Cancer (N. Y., NY, U. S.), D. Calvin, L. Mensha, S. Shivers, N. Ibrahim, V. Valero, M. Royce,
2005, 103, 2241–2251. C. Cox, J. A. Werner, Y. Kitagawa and B. Arun, G. Whitman, J. Ross,
46 C. Schairer, P. J. Mink, L. Carroll and M. Kitajima, Cancer Metastasis Rev., N. Sneige, G. N. Hortobagyi and
S. S. Devesa, J. Natl. Cancer Inst., 2004, 2006, 25, 221–232. L. Pusztai, J. Clin. Oncol., 2004, 22,
96, 1311–1321. 65 A. Stevanovic, P. Lee and N. Wilcken, 2284–2293.
47 M. Kaufmann and A. Rody, J. Cancer Aust. Fam. Physician, 2006, 35, 309–312. 82 M. Ellis and K. Ballman, J. Clin. Oncol.,
Res. Clin. Oncol., 2005, 131, 487–494. 66 T. A. DiMeo and C. Kuperwasser, Breast 2004, 22, 2267–2269.
48 H. F. Kennecke, I. A. Olivotto, C. Speers, Cancer Res., 2006, 8, 301. 83 J. C. Chang, E. C. Wooten, A. Tsimelzon,
B. Norris, S. K. Chia, C. Bryce and 67 A. J. Minn, Y. Kang, I. Serganova, S. G. Hilsenbeck, M. C. Gutierrez,
K. A. Gelmon, Ann. Oncol., 2007, 18, G. P. Gupta, D. D. Giri, M. Doubrovin, Y. L. Tham, M. Kalidas, R. Elledge,
45–51. V. Ponomarev, W. L. Gerald, R. Blasberg S. Mohsin, C. K. Osborne, G. C.
49 G. L. Semenza, Trends Mol. Med., 2002, and J. Massague, J. Clin. Invest., 2005, Chamness, D. C. Allred, M. T. Lewis,
8, S62–S67. 115, 44–55. H. Wong and P. O’Connell, J. Clin.
50 J. T. Erler, K. L. Bennewith, M. Nicolau, 68 Y. Kang, P. M. Siegel, W. Shu, Oncol., 2005, 23, 1169–1177.
N. Dornhofer, C. Kong, Q. T. Le, M. Drobnjak, S. M. Kakonen, 84 O. Thuerigen, A. Schneeweiss, G. Toedt,
J. T. Chi, S. S. Jeffrey and A. J. Giaccia, C. Cordon-Cardo, T. A. Guise and P. Warnat, M. Hahn, H. Kramer,
Nature, 2006, 440, 1222–1226. J. Massague, Cancer Cell, 2003, 3, B. Brors, C. Rudlowski, A. Benner,
51 J. T. Chi, Z. Wang, D. S. Nuyten, 537–549. F. Schuetz, B. Tews, R. Eils, H. P. Sinn,
E. H. Rodriguez, M. E. Schaner, 69 U. Woelfle, J. Cloos, G. Sauter, C. Sohn and P. Lichter, J. Clin. Oncol.,
A. Salim, Y. Wang, G. B. Kristensen, L. Riethdorf, F. Janicke, P. van Diest, 2006, 24, 1839–1845.
A. Helland, A. L. Borresen-Dale, R. Brakenhoff and K. Pantel, Cancer 85 E. Huang, S. Ishida, J. Pittman,
A. Giaccia, M. T. Longaker, T. Hastie, Res., 2003, 63, 5679–5684. H. Dressman, A. Bild, M. Kloos,
G. P. Yang, M. J. Vijver and P. O. Brown, 70 M. Smid, Y. Wang, J. G. Klijn, M. D’Amico, R. G. Pestell, M. West
PLoS Med., 2006, 3, e47. A. M. Sieuwerts, Y. Zhang, D. Atkins, and J. R. Nevins, Nat. Genet., 2003,
52 N. C. Denko, L. A. Fontana, K. M. J. W. Martens and J. A. Foekens, J. Clin. 34(2), 226–30.
Hudson, P. D. Sutphin, S. Raychaudhuri, Oncol., 2006, 24, 2261–2267. 86 A. H. Bild, G. Yao, J. T. Chang,
R. Altman and A. J. Giaccia, Oncogene, 71 S. L. Kominsky and N. E. Davidson, Q. Wang, A. Potti, D. Chasse, M. B.
2003, 22, 5907–5914. J. Clin. Oncol., 2006, 24, 2227–2229. Joshi, D. Harpole, J. M. Lancaster,
This journal is ß The Royal Society of Chemistry 2007 Mol. BioSyst., 2007, 3, 466–472 | 471View Article Online
A. Berchuck, J. A. Olson, J. R. Marks, Erlander, J. Clin. Oncol., 2006, 24, 103 L. Ein-Dor, I. Kela, G. Getz, D. Givol
H. K. Dressman, M. West and J. R. 4611–4619. and E. Domany, Bioinformatics, 2005, 21,
Nevins, Nature, 2006, 439, 353–357. 96 X. J. Ma, Z. Wang, P. D. Ryan, 171–178.
87 J. Downward, Nature, 2006, 439, S. J. Isakoff, A. Barmettler, A. Fuller, 104 R. Simon, M. D. Radmacher, K. Dobbin
274–275. B. Muir, G. Mohapatra, R. Salunga, and L. M. McShane, J. Natl. Cancer
88 A. H. Bild, A. Potti and J. R. Nevins, J. T. Tuggle, Y. Tran, D. Tran, A. Tassin, Inst., 2003, 95, 14–18.
Nat. Rev. Cancer, 2006, 6, 735–741. P. Amon, W. Wang, W. Wang, 105 L. Pusztai, C. Mazouni, K. Anderson,
89 M. Cronin, M. Pho, D. Dutta, J. C. E. Enright, K. Stecker, E. Estepa-Sabal, Y. Wu and W. F. Symmans, Oncologist,
Stephans, S. Shak, M. C. Kiefer, B. Smith, J. Younger, U. Balis, 2006, 11, 868–877.
J. M. Esteban and J. B. Baker, Am. J. J. Michaelson, A. Bhan, K. Habin, 106 L. Shi, W. Tong, F. Goodsaid,
Pathol., 2004, 164, 35–42. T. M. Baer, J. Brugge, D. A. Haber, F. W. Frueh, H. Fang, T. Han, J. C.
90 L. A. Habel, S. Shak, M. K. Jacobs, M. G. Erlander and D. C. Sgroi, Cancer Fuscoe and D. A. Casciano, Expert Rev.
A. Capra, C. Alexander, M. Pho, Cell, 2004, 5, 607–616. Mol. Diagn., 2004, 4, 761–777.
Open Access Article. Published on 05 June 2007. Downloaded on 11/17/2021 1:24:38 PM.
J. Baker, M. Walker, D. Watson, 97 M. P. Goetz, V. J. Suman, J. N. Ingle, 107 J. F. Reid, L. Lusa, L. De Cecco,
J. Hackett, N. T. Blick, D. Greenberg, A. M. Nibbe, D. W. Visscher, D. Coradini, S. Veneroni, M. G.
L. Fehrenbacher, B. Langholz and C . A. R e yn o l d s, W. L . L i n gl e , Daidone, M. Gariboldi and M. A.
C. P. Quesenberry, Breast Cancer Res., M. Erlander, X. J. Ma, D. C. Sgroi, Pierotti, J. Natl. Cancer Inst., 2005, 97,
2006, 8, R25. E. A. Perez and F. J. Couch, Clin. Cancer 927–930.
91 S. Paik, S. Shak, G. Tang, C. Kim, Res., 2006, 12, 2080–2087. 108 J. P. Ioannidis, Lancet, 2005, 365,
J. Baker, M. Cronin, F. L. Baehner, 454–455.
98 M. P. Jansen, J. A. Foekens, I. L.
M. G. Walker, D. Watson, T. Park, 109 S. Michiels, S. Koscielny and C. Hill,
van Staveren, M. M. Dirkzwager-Kiel,
W. Hiller, E. R. Fisher, D. L. Lancet, 2005, 365, 488–492.
K. Ritstier, M. P. Look, M. E. Meijer-
Wickerham, J. Bryant and N. Wolmark, 110 R. Shen, D. Ghosh and A. M.
van Gelder, A. M. Sieuwerts,
New Engl. J. Med., 2004, 351, 2817–2826. Chinnaiyan, BMC Genomics, 2004, 5, 94.
H. Portengen, L. C. Dorssers, J. G. Klijn
92 S. Paik, G. Tang, S. Shak, C. Kim, 111 P. G. Febbo and P. W. Kantoff, J. Clin.
and E. M. Berns, J. Clin. Oncol., 2005,
J. Baker, W. Kim, M. Cronin, F. L. Oncol., 2006, 24, 3719–3721.
Baehner, D. Watson, J. Bryant, J. P. 23, 732–740. 112 F. Dudbridge, A. Gusnanto and B. P.
Costantino, C. E. Geyer, D. L. 99 J. Lamb, E. D. Crawford, D. Peck, Koeleman, Hum. Genomics, 2006, 2,
Wickerham and N. Wolmark, J. Clin. J. W. Modell, I. C. Blat, M. J. 310–317.
Oncol., 2006, 24, 3726–3734. Wrobel, J. Lerner, J. P. Brunet, 113 A. Subramanian, P. Tamayo, V. K.
93 F. J. Esteva, A. A. Sahin, M. Cristofanilli, A. Subramanian, K. N. Ross, M. Reich, Mootha, S. Mukherjee, B. L. Ebert,
K. Coombes, S. J. Lee, J. Baker, H. H i e r o n y m u s , G . W e i , S . A . M. A. Gillette, A. Paulovich, S. L.
M. Cronin, M. Walker, D. Watson, Armstrong, S. J. Haggarty, P. A. Pomeroy, T. R. Golub, E. S. Lander
S. Shak and G. N. Hortobagyi, Clin. Clemons, R. Wei, S. A. Carr, and J. P. Mesirov, Proc. Natl. Acad. Sci.
Cancer Res., 2005, 11, 3315–3319. E. S. Lander and T. R. Golub, Science, U. S. A., 2005, 102, 15545–15550.
94 S. Paik, G. Tang, S. Shak, C. Kim, 2006, 313, 1929–1935. 114 B. Efron and R. Tibshirani, On testing
J. Baker, W. Kim, M. Cronin, F. L. 100 A. A. Ahmed and J. D. Brenton, Breast the significance of sets of genes, 2006,
Baehner, D. Watson, J. Bryant, J. P. Cancer Res., 2005, 7, 96–99. http://stat.stanford.edu/ybrad/papers/
Costantino, C. E. Geyer, D. L. 101 C. Fan, D. S. Oh, L. Wessels, B. Weigelt, genesetpaper.pdf.
Wickerham and N. Wolmark, J. Clin. D. S. Nuyten, A. B. Nobel, L. J. van’t 115 M. Nicolau, R. Tibshirani, A. L.
Oncol., 2006, 24, 3726–3734. Veer and C. M. Perou, New Engl. J. Børresen-Dale and S. S. Jeffrey,
95 X. J. Ma, S. G. Hilsenbeck, W. Wang, Med., 2006, 355, 560–569. Bioinformatics, 2007, 23, 957–265.
L. Ding, D. C. Sgroi, R. A. Bender, 102 J. A. O’Shaughnessy, New Engl. J. Med., 116 D. F. Ransohoff, Nat. Rev. Cancer, 2004,
C. K. Osborne, D. C. Allred and M. G. 2006, 355, 615–617. 4, 309–314.
472 | Mol. BioSyst., 2007, 3, 466–472 This journal is ß The Royal Society of Chemistry 2007You can also read