Mediterranean Diet and Mild Cognitive Impairment
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
ORIGINAL CONTRIBUTION
Mediterranean Diet and Mild Cognitive Impairment
Nikolaos Scarmeas, MD; Yaakov Stern, PhD; Richard Mayeux, MD;
Jennifer J. Manly, PhD; Nicole Schupf, PhD; Jose A. Luchsinger, MD
Background: Higher adherence to the Mediterranean follow-up of 4.5 (2.7) years (range, 0.9-16.4 years). Com-
diet (MeDi) may protect from Alzheimer disease (AD), pared with subjects in the lowest MeDi adherence tertile,
but its association with mild cognitive impairment (MCI) subjects in the middle tertile had 17% less risk (hazard
has not been explored. ratio [HR] = 0.83; 95% confidence interval [CI], 0.62-
1.12; P =.24) of developing MCI and those in the high-
Objective: To investigate the association between the est tertile had 28% less risk (HR = 0.72; 95% CI, 0.52-
MeDi and MCI. 1.00; P=.05) of developing MCI (trend HR=0.85; 95%
CI, 0.72-1.00; P for trend = .05). There were 482 sub-
Design, Setting, and Patients: In a multiethnic com-
jects with MCI, 106 of whom developed AD during a mean
munity study in New York, we used Cox proportional haz-
(SD) follow-up of 4.3 (2.7) years (range, 1.0-13.8 years).
ards to investigate the association between adherence to
Compared with subjects in the lowest MeDi adherence
the MeDi (0-9 scale; higher scores indicate higher adher-
ence) and (1) the incidence of MCI and (2) the progres- tertile, subjects in the middle tertile had 45% less risk
sion from MCI to AD. All of the models were adjusted for (HR=0.55; 95% CI, 0.34-0.90; P=.01) of developing AD
cohort, age, sex, ethnicity, education, APOE genotype, ca- and those in the highest tertile had 48% less risk
loric intake, body mass index, and duration between base- (HR=0.52; 95% CI, 0.30-0.91; P=.02) of developing AD
line dietary assessment and baseline diagnosis. (trend HR=0.71; 95% CI, 0.53-0.95; P for trend=.02).
Main Outcome Measures: Incidence of MCI and pro- Conclusions: Higher adherence to the MeDi is associ-
gression from MCI to AD. ated with a trend for reduced risk of developing MCI and
with reduced risk of MCI conversion to AD.
Results: There were 1393 cognitively normal partici-
pants, 275 of whom developed MCI during a mean (SD) Arch Neurol. 2009;66(2):216-225
T
HE CONCEPT OF MILD COG- take of fish, vegetables, legumes, fruits, ce-
nitive impairment (MCI) reals, and unsaturated fatty acids [mostly
was developed to identify in the form of olive oil], low intake of dairy
subjects who are in the products, meat, and saturated fatty acids,
transitional stage between and a regular but moderate intake of al-
normal aging and dementia or Alzheimer cohol3) is associated with lower AD risk.4,5
disease (AD). Because of the high conver- Some studies have investigated the effect
sion rates, subjects with MCI constitute a of individual elements of the MeDi (ie, al-
population suited for study of demen- cohol, fatty acids, and fish) in MCI and age-
tia-AD risk factor epidemiology and for in- related cognitive decline6-12 and have found
Author Affiliations:
Departments of Neurology vestigation of possible behavioral or phar- conflicting results. Nevertheless, poten-
(Drs Scarmeas, Stern, Mayeux, macological preventive interventions. tial associations between the entire MeDi
and Manly) and Medicine Among behavioral traits, diet may play an pattern and MCI have not been explored.
(Dr Luchsinger), the important role in the cause and preven- We examined the association between the
Gertrude H. Sergievsky Center tion of AD. However, epidemiological data MeDi and MCI using data from the Wash-
(Drs Scarmeas, Stern, Mayeux, on diet and AD have been conflicting.1,2 ington Heights–Inwood Columbia Aging
Manly, and Schupf ), and the Moreover, there is a paucity of research on Project (WHICAP). We hypothesized that
Taub Institute for Research in
the effect of dietary factors on both rates cognitively normal participants with higher
Alzheimer’s Disease and the
Aging Brain (Drs Scarmeas,
of development of MCI and rates of MCI adherence to the MeDi would have a lower
Stern, Mayeux, Manly, Schupf, conversion to AD. risk of future development of MCI and that
and Luchsinger), Columbia We recently demonstrated that higher participants with MCI and higher MeDi ad-
University Medical Center, adherence to the Mediterranean diet herence would have a lower risk of devel-
New York, New York. (MeDi) (a diet characterized by high in- oping future AD.
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
216
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.METHODS clusive MCI subtypes: (1) MCI with objective memory impair-
ment (with or without objective impairment in other cognitive
domains), and (2) MCI without objective memory impairment
SAMPLE AND DIAGNOSES (objective impairment in ⱖ1 of the 3 nonmemory domains but
a memory domain composite score within norms). Dietary data
The sample for the current study has been described in detail in were not available to the consensus panel and were not consid-
recent studies exploring the frequency and course of MCI in our ered in the MCI diagnostic process. Subjects were followed up
cohorts.13,14 The study included participants of 2 related co- at intervals of approximately 1.5 years, repeating the baseline ex-
horts recruited in 1992 (WHICAP 1992) and 1999 (WHICAP amination and consensus diagnosis at each follow-up.
1999) who were identified (via ethnicity and age stratification
processes) from a probability sample of Medicare beneficiaries
residing in an area of 3 contiguous census tracts within a geo- PREDICTORS
graphically defined area of northern Manhattan, New York.15 The
same assessments and study procedures were used in both co- Diet
horts. At entry, a physician elicited each subject’s medical and
neurological history and conducted a standardized physical and Dietary data regarding average food consumption during the past
neurological examination. All available ancillary information year were obtained using a 61-item version of the semiquantita-
(medical records, computed tomographic scans, or magnetic reso- tive food frequency questionnaire by Willett et al25 (Channing
nance images) was considered in the evaluation. Laboratory, Cambridge, Massachusetts). Trained interviewers ad-
Each subject also underwent a structured in-person inter- ministered the semiquantitative food frequency questionnaire in
view including an assessment of health and function and a neu- English or Spanish. We have previously reported validity (using
ropsychological battery. Functional assessment of instrumental two 7-day food records) and reliability (using two 3-month fre-
activities of daily living included a disability and functional limi- quency assessments) of various components of the semiquanti-
tations scale.16,17 The neuropsychological battery18 contained tests tative food frequency questionnaire in the WHICAP.26-28
of memory (short- and long-term verbal and nonverbal), orien- Similar to our previous work,4,5,29 we followed a method pre-
tation, abstract reasoning (verbal and nonverbal), language (nam- viously described3 for the construction of the MeDi score. More
ing, verbal fluency, comprehension, and repetition), and con- specifically, we first regressed caloric intake (in kilocalories) and
struction (copying and matching). A global summary score on calculated the derived residuals of daily gram intake30 for each of
the Clinical Dementia Rating (CDR)19 was also assigned. the following 7 categories3: dairy, meat, fruits, vegetables, le-
A consensus diagnosis for the presence or absence of demen- gumes, cereals, and fish. A value of 0 or 1 was assigned to each of
tia was made at a diagnostic conference of neurologists and neu- the 7 groups using sex-specific medians as cutoffs. For benefi-
ropsychologists where information of all the above evaluations cial components (fruits, vegetables, legumes, cereals, and fish),
was presented. Evidence of cognitive deficit (based on the neu- persons whose consumption was below the median were as-
ropsychological scores as described earlier), evidence of impair- signed a value of 0 and persons whose consumption was at or
ment in social or occupational function (as assessed by the Blessed above the median were assigned a value of 1. For components
Dementia Rating Scale, the Schwab and England Activities of Daily presumed to be detrimental (meat and dairy products), persons
Living Scale, and the physician’s assessment), and evidence of whose consumption was below the median were assigned a value
cognitive and social-occupational function decline were the cri- of 1 and persons whose consumption was at or above the me-
teria used for the diagnosis of dementia as required by the Di- dian were assigned a value of 0. For fat intake (eighth food cat-
agnostic and Statistical Manual of Mental Disorders, Revised Third egory), we used the ratio of daily consumption (in grams) of mono-
Edition.20 The type of dementia was subsequently determined. unsaturated lipids to saturated lipids3 (again using sex-specific
For the diagnosis of probable or possible AD, the criteria of the median cutoffs for assignment values of 0 for low and 1 for high).
National Institute of Neurological and Communicative Disor- For alcohol intake (ninth food category), subjects were assigned
ders and Stroke–Alzheimer Disease and Related Disorders As- a score of 0 for either no consumption (0 g/d) or more than mod-
sociation21 were used. erate consumption (ⱖ30 g/d) and a value of 1 for mild to mod-
Because the current study had started before the concept of erate alcohol consumption (⬎0 to ⬍30 g/d). This is in agree-
MCI was developed, diagnosis of MCI was not part of the stan- ment with previous reports3 that consider a moderate amount of
dard consensus conference procedure but was retrospectively ap- alcohol consumption as another characteristic component of the
plied after the consensus conference for each visit among non- MeDi. We also classified alcohol consumption dichotomously be-
demented individuals. Details on the MCI definition have been cause of the skewed distribution of alcohol consumption in our
previously provided.13,14 Briefly, consistent with standard crite- population (68% reporting no alcohol intake, 31% reporting ⬍30
ria,22 subjects considered for MCI were required to have the fol- g/d [mild to moderate intake], and 1% reporting ⱖ30 g/d [heavy
lowing. First, they had a subjective memory complaint (using intake]). The MeDi score was generated for each participant by
items from the Disability and Functional Limitations Scale16,17 adding the scores in the food categories (theoretically ranging from
and the Blessed Functional Activities Scale23). Second, they had 0-9) with a higher score indicating higher adherence to the MeDi.
objective impairment in at least 1 cognitive domain. Using se- We used the MeDi score from the first time the dietary as-
lected items from the neuropsychological battery, 4 cognitive do- sessment was performed as the main predictor in the survival
mains (memory, executive, language, and visuospatial) were de- analyses. Because the cognitively normal and MCI definitions were
fined.13,14 Impairment was defined based on the average of the partly based on availability of neuropsychological assessments,
scores on the neuropsychological measures within that domain their ascertainment was not always synchronous with the di-
and a 1.5-SD cutoff using corrections for age, years of educa- etary assessments. For the incident MCI analyses, the time of the
tion, ethnicity, and sex and based on the previously established first dietary assessment coincided (±1.5 years) with the time of
norms. Third, they had essentially preserved activities of daily the first assessment of cognitively normal status for 82% of the
living (defined earlier). Fourth, they had no diagnosis of demen- subjects, was more than 1.5 years earlier for 14% of the sub-
tia at the consensus conference. To further explore the associa- jects, and was more than 1.5 years later for only 4%. For the in-
tion of the MeDi to MCI, in the view of the original criteria by cident AD analyses, the time of the first dietary assessment co-
Petersen et al22,24 (which focus on objective memory impair- incided (±1.5 years) with the time of the first assessment of MCI
ment), the overall MCI group was divided into 2 mutually ex- status for 84% of the subjects, was more than 1.5 years earlier
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
217
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.used as time-constant covariates. In additional analyses, we re-
calculated the models using the 2 different types of MCI as the
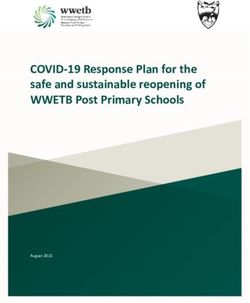
2364 Nondemented
outcomes: with and without memory impairment.
1800 Cognitively normal 564 With MCI MCI to Incident AD
184 Missing dietary 82 Missing dietary We calculated Cox proportional hazards models with AD as
data data
the dichotomous outcome. The time-to-event variable was the
time from the first MCI status to the first visit with an AD di-
223 With CDR of
0.5 agnosis. Subjects diagnosed with AD and then reverting back
to MCI were considered cases, and their first AD diagnostic visit
1393 With final finding 482 With final finding was considered the event visit. Therefore, censored subjects never
of cognitively normal of MCI developed AD at any of their follow-up visits. Persons who did
not develop AD were censored at the time of their last fol-
low-up (ie, all of the subject visits before the last follow-up were
Figure 1. Flowchart describing the sample. MCI indicates mild cognitive used in the analyses). Predictors and covariates were the same
impairment; CDR, Clinical Dementia Rating.
as in the earlier-described models for cognitively normal to in-
cident MCI. In additional analyses, we recalculated the mod-
for 11% of the subjects, and was more than 1.5 years later for els using the 2 different types of MCI (with and without memory
only 5%. To summarize, the timing of the MeDi adherence as- impairment) as the starting point.
sessment and the cognitively normal or MCI assessments over-
lapped to a significant degree. Despite this, in all of the survival
models we included a term adjusting for the difference in the RESULTS
time between the first dietary assessment and the first cognitive
status assessment. MISSING DATA ANALYSES
Covariates Among all of the potential participants in both WHICAP
cohorts, 2364 individuals were considered for this study
Age (in years), education (in years), caloric intake (in kilocalo- because of sufficient data for MCI diagnosis and available
ries), and body mass index (BMI) (weight in kilograms divided follow-up14 (Figure 1). As previously reported,14 in com-
by height in meters squared)31 were used as continuous vari- parison with 1329 subjects who were not considered be-
ables. We also considered cohort (1992 cohort as the reference) cause of missing data or lack of follow-up, these 2364 sub-
and sex (men as the reference). Ethnic group was based on self-
report using the format of the 1990 census.32 Participants were
jects were slightly younger, were more likely to be women,
then assigned to 1 of 4 groups: black (non-Hispanic), Hispanic, and had higher cognitive performance but did not differ
white (non-Hispanic), or other. Ethnicity was used as a dummy in ethnicity. Among the 2364 subjects, 1800 were cogni-
variable with white (non-Hispanic) as the reference. Apolipopro- tively normal (nondemented, non-MCI) at the initial evalu-
tein E (APOE) genotype was used dichotomously: absence of the ation (serving for calculation of the effect of the MeDi on
ε4 allele vs presence of either 1 or 2 ε4 alleles. the incidence of MCI) and 564 were diagnosed with MCI
at the initial evaluation (serving for calculation of the effect
STATISTICAL ANALYSES of the MeDi on the MCI conversion to AD).
Baseline characteristics of subjects by missing dietary data, by Cognitively Normal to Incident MCI Analyses
outcome of interest, and by MeDi adherence tertiles were com-
pared using t test or analysis of variance for continuous vari- Among the 1800 subjects who were cognitively normal
ables and 2 test for categorical variables. at the initial evaluation, dietary information was missing
for 184 subjects (partly because the dietary assessment com-
Cognitively Normal to Incident MCI ponent was added after initiation of the study) (Figure 1).
To have an even cleaner sample for the incident MCI analy-
We calculated Cox proportional hazards models with MCI as
the dichotomous outcome. The time-to-event variable was the
ses, we additionally excluded 223 subjects who, despite
time from the first cognitively normal status to the first visit not meeting our MCI criteria, had a CDR of 0.5 at the first
with an MCI diagnosis. Subjects diagnosed with MCI and then evaluation. Compared with the 184 subjects with miss-
reverting back to normal were considered cases, and their first ing dietary information, the 1393 cognitively normal sub-
MCI diagnostic visit was considered the event visit. Persons who jects (with a CDR of 0.0 and available dietary informa-
did not develop MCI were censored at the time of their last fol- tion) used for the incident MCI analyses had lower BMIs
low-up (ie, all subject visits before the last follow-up were used (28.5 vs 27.5, respectively; P=.02) and borderline higher
in the analyses). The main predictor was the MeDi score (from cognitive performance (composite cognitive z score, 0.37
the first dietary evaluation) as a continuous variable initially vs 0.46, respectively; P=.05). The groups did not differ in
and in tertiles subsequently (used for trend test calculation). sex, age, ethnicity, education, or APOE status. As ex-
We simultaneously adjusted for the following variables: co-
hort, age at intake in the study, sex, ethnicity, education, APOE
pected, compared with the 223 subjects with a CDR of 0.5,
genotype, BMI, and time between the first dietary assessment the 1393 cognitively normal subjects (with a CDR of 0.0
and the first cognitive status assessment. Although caloric intake– and available dietary information) used for the incident
adjusted residuals were used in the MeDi score calculation, we MCI analyses were younger (79.0 vs 76.7 years, respec-
also included caloric intake as a covariate in the models (as rec- tively; P⬍.001), were more educated (6.8 vs 10.8 years
ommended by Willett and Stampfer30). All of the predictors were of school, respectively; P⬍.001), had higher cognitive per-
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
218
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.Table 1. Demographic and Clinical Characteristics During the First Evaluation for All Subjects
Cognitively Normal MCI All Subjects
Characteristic (n=1393) (n = 482) (n = 1875) P Value
Men, No. (%) 447 (32) 156 (32) 603 (32) .91
Age, mean (SD), y 76.7 (6.5) 77.5 (6.6) 76.9 (6.5) .02
Ethnicity, No. (%)
White 434 (31) 124 (26) 558 (30)
Black 479 (34) 144 (30) 623 (33)
⬍.001
Hispanic 473 (34) 214 (44) 687 (36)
Other 7 (1) 0 7 (1)
Education, mean (SD), y 10.8 (4.6) 9.1 (4.9) 10.4 (4.7) ⬍.001
ⱖ1 ε4 allele, No. (%) 327 (27) 127 (30) 454 (28) .18
BMI, mean (SD) 27.5 (5.5) 27.2 (5.3) 27.4 (5.4) .34
Energy, mean (SD), kcal 1426.1 (498.0) 1421.8 (591.9) 1425.0 (523.6) .88
MeDi score, mean (SD) 4.37 (1.69) 4.31 (1.62) 4.36 (1.67) .47
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MCI, mild cognitive impairment;
MeDi, Mediterranean diet.
Table 2. Demographic and Clinical Characteristics During the First Evaluation for All Subjects
by Mediterranean Diet Adherence Tertiles
MeDi Adherence Tertile
Low Middle High
Characteristic (n=609) (n = 775) (n = 491) P Value
Men, No. (%) 442 (69) 532 (69) 318 (65) .23
Age, mean (SD), y 76.9 (6.6) 76.8 (6.5) 77.2 (6.2) .48
Ethnicity, No. (%)
White 182 (30) 223 (29) 153 (31)
Black 234 (38) 260 (33) 139 (26)
.001
Hispanic 190 (31) 289 (37) 208 (42)
Other 3 (1) 3 (1) 1 (1)
Education, mean (SD), y 10.5 (4.5) 10.3 (4.7) 10.4 (4.9) .77
ⱖ1 ε4 allele, No. (%) 146 (27) 179 (27) 129 (29) .70
BMI, mean (SD) 27.7 (5.8) 27.4 (5.2) 27.1 (5.3) .19
Energy, mean (SD), kcal 1494.9 (608.2) a 1395.4 (472.5) a 1385.1 (477.4) a ⬍.001
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MeDi, Mediterranean diet.
a P ⬍ .05 for all MeDi adherence tertiles according to post hoc Scheffé test.
formance (composite cognitive z score, −0.46 vs 0.46, re- be white (Table 1). Cognitively normal subjects and sub-
spectively; P⬍.001), and were more likely to be white (11% jects with MCI did not differ in sex, APOE genotype, BMI,
vs 31%, respectively) and less likely to be Hispanic (60% total caloric intake, and MeDi adherence.
vs 34%, respectively) (P⬍.001). The groups did not dif- Hispanic subjects adhered more to the MeDi, black
fer in sex, BMI, or APOE status. subjects adhered less, and white subjects’ adherence was
in between (Table 2). The higher the MeDi adherence
MCI to Incident AD Analyses was, the lower the total caloric intake was. There was no
association between the MeDi score and age, sex, edu-
Compared with the 82 subjects with MCI and missing cation, APOE genotype, or BMI.
dietary information, the 482 subjects with MCI and avail-
able dietary information included in the incident AD
analyses had borderline higher education (8.0 vs 9.1 years MeDi AND RISK FOR INCIDENT MCI
of school, respectively; P=.05) and borderline higher cog-
nitive performance (composite cognitive z score, −0.40 Despite somewhat lower scores in subjects with MCI (as
vs −0.27, respectively; P = .05). The groups did not dif- compared with cognitively normal subjects) at baseline
fer in sex, age, ethnicity, APOE status, or BMI. (Table 1), the groups did not significantly differ cross-
sectionally. Longitudinal analyses (particularly with use
CLINICAL, DEMOGRAPHIC, of survival models) are a much more powerful method
AND DIETARY CHARACTERISTICS of detecting predictor differences because they can com-
bine in a single statistic 2 different risk dimensions: (1)
At the first evaluation, compared with subjects who were the proportion of subjects who reach an event (convert
cognitively normal, subjects with MCI were older, less to MCI or AD), and (2) duration (how soon subjects con-
educated, more likely to be Hispanic, and less likely to vert or nonconvert to MCI or AD).
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
219
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
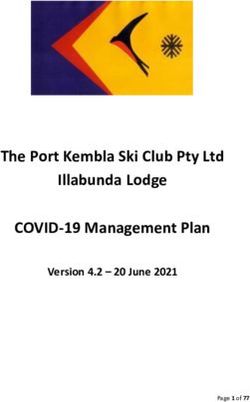
©2009 American Medical Association. All rights reserved.Table 3. Cox Proportional Hazard Ratios for Incidence 1.00
of Mild Cognitive Impairment for Subjects Who Were
Cognitively Normal at the First Evaluation 0.95
Cumulative Probability of Remaining MCI-Free
by Mediterranean Diet Score
0.90
Predictor HR (95% CI) P Value
0.85
Unadjusted a
MeDi continuous 0.93 (0.87-1.00) .06 0.80
MeDi tertile
Low 1 [Reference] NA 0.75
Middle 0.87 (0.66-1.14) .33
High 0.73 (0.53-1.00) .05 0.70
Trend 0.85 (0.73-1.00) .05
0.65 MeDi tertile
Adjusted b
Low
MeDi continuous 0.92 (0.85-0.99) .04 Middle
0.60
MeDi tertile High
Low 1 [Reference] NA
0.55
Middle 0.83 (0.62-1.12) .24 0 1 2 3 4 5 6 7 8 9 10
High 0.72 (0.52-1.00) .05 Time From Baseline, y
Trend 0.85 (0.72-1.00) .05
Figure 2. Survival curves based on Cox analysis comparing cumulative mild
Abbreviations: CI, confidence interval; HR, hazard ratio; cognitive impairment (MCI) incidence in subjects who were cognitively
MeDi, Mediterranean diet; NA, not applicable. normal at the first evaluation by each Mediterranean diet (MeDi) adherence
a A total of 1393 subjects were cognitively normal at the first evaluation;
tertile (P for trend = .05). The figure is derived from a model that is adjusted
275 subjects developed incident mild cognitive impairment. for cohort, age, sex, ethnicity, education, APOE genotype, caloric intake,
b A total of 1199 subjects were cognitively normal at the first evaluation;
body mass index, and time between the first dietary assessment and the first
241 subjects developed incident mild cognitive impairment. Adjusted models cognitive assessment. Duration of follow-up is truncated at 10 years. Results
include a slightly lower number of subjects because of missing data in some of log-rank tests for pairwise comparisons are as follows: middle vs low
of the covariates; they simultaneously control for cohort, age, sex, ethnicity, tertile, 2 = 0.91, P = .33; low vs high tertile, 2 = 3.72, P = .05; and middle vs
education, APOE genotype, caloric intake, body mass index, and time high tertile, 2 = 1.22, P = .26.
between the first dietary assessment and the first cognitive assessment.
ment and those in the highest tertile had an HR of 0.71
Subjects who were cognitively normal at the first evalu- (95% CI, 0.46-1.12; P =.14). The overall MeDi HR trend
ation were followed up (until MCI incidence or the last was 0.84 (95% CI, 0.67-1.05; P for trend=.13).
follow-up for subjects who remained cognitively nor-
mal) for a mean (SD) of 4.5 (2.7) years (range, 0.9-16.4 MeDi AND RISK FOR MCI CONVERSION TO AD
years). Overall, 275 subjects developed incident MCI.
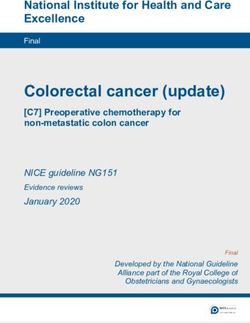
Higher adherence to the MeDi was associated with a Subjects with MCI at the first evaluation were followed up
borderline trend for lower risk of developing MCI (until AD incidence or last follow-up for subjects who did
(Table 3 and Figure 2). The results were similar in not develop AD) for a mean (SD) of 4.3 (2.7) years (range,
adjusted and unadjusted models. Each additional unit of 1.0-13.8 years). Overall, 106 subjects developed AD.
the MeDi score was associated with 8% less risk (P=.04) Higher adherence to the MeDi was associated with lower
of developing MCI. Compared with subjects in the low- risk of developing AD (Table 4 and Figure 3). The re-
est MeDi adherence tertile, subjects in the middle tertile sults were similar in adjusted and unadjusted models. Each
had 17% less risk (P= .24) of developing MCI and those additional unit of the MeDi score was associated with 11%
in the highest tertile had 28% less risk (P = .05) of devel- less risk (P=.09) of developing AD. Compared with sub-
oping MCI. Among the other covariates in the model, jects in the lowest MeDi adherence tertile, subjects in the
younger age and higher education were the only protec- middle tertile had 45% less risk (P=.01) of developing AD
tive factors for development of MCI. and those in the highest tertile had 48% less risk (P=.02)
The effect of the MeDi on development of different of developing AD. Among the other covariates in the model,
MCI subtypes is subject to power limitations but is still younger age, higher education, and higher BMI were the
worth exploring. Overall, 108 subjects developed inci- only protective factors for development of AD.
dent MCI with memory impairment. In fully adjusted At the first evaluation, 175 subjects had MCI with
models, as compared with subjects in the lowest MeDi memory impairment; 49 of them developed AD at follow-
adherence tertile, those in the middle tertile had a haz- up. In fully adjusted models, as compared with subjects
ard ratio (HR) of 0.90 (95% confidence interval [CI], 0.57- who had MCI with memory impairment belonging to the
1.40; P=.64) for developing MCI with memory impair- lowest MeDi adherence tertile, those who had MCI with
ment, whereas those in the highest tertile had an HR of memory impairment in the middle tertile had an HR of
0.71 (95% CI, 0.43-1.17; P = .18). The overall MeDi HR 0.48 (95% CI, 0.22-1.04; P =.06) for developing AD and
trend was 0.84 (95% CI, 0.66-1.03; P for trend=.18). A those who had MCI with memory impairment in the high-
total of 133 subjects developed MCI without memory im- est tertile had an HR of 0.71 (95% CI, 0.32-1.59; P=.41).
pairment. In fully adjusted models, as compared with sub- The overall MeDi HR trend was 0.84 (95% CI, 0.55-
jects in the lowest MeDi adherence tertile, those in the 1.29; P for trend=.45). At the first evaluation, 234 sub-
middle tertile had an HR of 0.79 (95% CI, 0.53-1.19; jects had MCI without memory impairment; 47 of them
P = .27) for developing MCI without memory impair- developed AD at follow-up. In fully adjusted models, as
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
220
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.Table 4. Cox Proportional Hazard Ratios for Incidence 1.00
of Alzheimer Disease for Subjects With Mild Cognitive
0.95
Impairment at the First Evaluation
by Mediterranean Diet Score 0.90
0.85
Predictor HR (95% CI) P Value
Cumulative Probability of Remaining AD-Free
0.80
Unadjusted a
MeDi continuous 0.95 (0.85-1.07) .48 0.75
MeDi tertile
0.70
Low 1 [Reference] NA
Middle 0.62 (0.39-0.98) .04 0.65
High 0.69 (0.41-1.14) .15
0.60
Trend 0.82 (0.63-1.07) .15
Adjusted b 0.55
MeDi continuous 0.89 (0.78-1.02) .09
0.50
MeDi tertile MeDi tertile
Low 1 [Reference] NA 0.45 Low
Middle 0.55 (0.34-0.90) .01 Middle
0.40 High
High 0.52 (0.30-0.91) .02
Trend 0.71 (0.53-0.95) .02 0.35
0 1 2 3 4 5 6 7 8 9 10
Time From Baseline MCI Diagnosis, y
Abbreviations: CI, confidence interval; HR, hazard ratio;
MeDi, Mediterranean diet; NA, not applicable.
a A total of 482 subjects had mild cognitive impairment at the first
Figure 3. Survival curves based on Cox analysis comparing cumulative
evaluation; 106 subjects developed incident Alzheimer disease. Alzheimer disease (AD) incidence in subjects with mild cognitive impairment
b A total of 409 subjects had mild cognitive impairment at the first
(MCI) at the first evaluation by Mediterranean diet (MeDi) adherence tertile
evaluation; 96 subjects developed incident Alzheimer disease. Adjusted (P for trend = .02). The figure is derived from a model that is adjusted for
models include a slightly lower number of subjects because of missing data cohort, age, sex, ethnicity, education, APOE genotype, caloric intake, body
in some of the covariates; they simultaneously control for cohort, age, sex, mass index, and time between the first dietary assessment and the first
ethnicity, education, APOE genotype, caloric intake, body mass index, and cognitive assessment. Duration of follow-up is truncated at 10 years. Results
time between the first dietary assessment and the first cognitive assessment. of log-rank tests for pairwise comparisons are as follows: middle vs low
tertile, 2 = 4.26, P = .03; low vs high tertile, 2 = 1.39, P = .23; and middle vs
high tertile, 2 = 0.12, P = .72.
compared with subjects who had MCI without memory
impairment in the lowest MeDi adherence tertile, those
who had MCI without memory impairment in the middle of 0.74 (95% CI, 0.53-1.04; P=.08), and the overall MeDi
tertile had an HR of 0.49 (95% CI, 0.24-1.01; P =.05) for tertile HR trend was 0.86 (95% CI, 0.72-1.02; P for
developing AD and those who had MCI without memory trend=.08). Including the comorbidity index (simulta-
impairment in the highest tertile had an HR of 0.25 (95% neously with all of the other covariates) in the incident
CI, 0.10-0.63; P = .003). The overall MeDi HR trend was AD analyses produced similar results: the middle tertile
0.50 (95% CI, 0.35-0.79; P for trend = .003). had an HR of 0.59 (95% CI, 0.36-0.97; P=.04), the high-
est tertile had an HR of 0.56 (95% CI, 0.32-0.97; P=.04),
SUPPLEMENTARY ANALYSES and the overall MeDi tertile HR trend was 0.74 (95% CI,
0.55-0.98; P for trend=.04).
Considering the possibility of an overall healthier life- In additional supplementary analyses, we used age
style behavior accounting for the MeDi effect, we consid- (rather than duration from cognitive assessment) as the
ered a measure of overall comorbidity in the analyses: a time-to–incident MCI variable. In these analyses, the di-
modified version33,34 of the Charlson Index of Comorbid- rectionality of the effect was similar but the strength was
ity.35 This measure includes items for myocardial infarct, significantly attenuated: the continuous MeDi HR was
congestive heart failure, peripheral vascular disease, hy- 0.94 (95% CI, 0.87-1.0; P=.09), the middle MeDi adher-
pertension, chronic renal disease, chronic obstructive pul- ence tertile had an HR of 0.91 (95% CI, 0.69-1.19; P=.49),
monary disease, arthritis, gastrointestinal disease, mild liver the highest tertile had an HR of 0.76 (95% CI, 0.56-
disease, diabetes, and systemic malignant neoplasms. There 1.04; P =.09), and the overall MeDi tertile HR trend was
was no difference in comorbidity index between subjects 0.87 (95% CI, 0.75-1.02; P for trend=.09).
who remained cognitively normal during follow-up and
those who developed MCI during follow-up (1.9 vs 1.9, COMMENT
respectively; P=.91) or between those who had MCI at base-
line and those who developed AD during follow-up (2.0 This study suggests that higher adherence to the MeDi is
vs 2.1, respectively; P=.66). Similarly, the comorbidity in- associated with a borderline reduction in the risk of de-
dex did not differ between levels of MeDi adherence: 1.9 veloping MCI and a reduction in the risk of conversion
for the lowest tertile, 1.9 for the middle tertile, and 1.9 for from MCI to AD. The gradual reduction in risks for higher
the highest tertile (P=.75). Including the comorbidity in- tertiles of MeDi adherence also suggests a possible dose-
dex (simultaneously with all of the other covariates) in the response effect. The associations between MeDi and the
incident MCI analyses did not appreciably change the re- risk of developing MCI and of MCI conversion to AD did
sults: the middle MeDi adherence tertile had an HR of 0.83 not attenuate even when simultaneously adjusting for many
(95% CI, 0.61-1.12; P=.23), the highest tertile had an HR commonly considered potential confounders such as age,
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
221
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.sex, ethnicity, education, APOE genotype, caloric intake, tein in multiple large observational52,90,91 and interven-
and BMI. Adherence to the MeDi did not seem to differ- tional55,81 studies. As another example, tyrosol and caf-
entially affect the risk of development of MCI with or with- feic acid, both found in extra-virgin olive oil and wine
out memory impairment. The association between higher (which are essential components of the MeDi), have been
adherence to the MeDi and lower risk of conversion to AD shown to significantly reduce interleukin 6 production
was much more prominent for subjects who had MCI with- from peripheral blood mononuclear cells of healthy vol-
out memory impairment. unteers.92 Higher adherence to the MeDi has been asso-
Higher adherence to the MeDi has been related to lower ciated with lower interleukin 6 levels in both observa-
risk of AD.4,5 Mild cognitive impairment has been de- tional52,91 and interventional55 studies. Higher adherence
scribed as a predictor or a transitional stage between nor- to the MeDi is in general associated with significant re-
mal cognition and AD.36,37 Thus, we expected that higher ductions in a series of other inflammatory markers in-
adherence to the MeDi would be related to MCI. The as- cluding white blood cell counts and others.52
sociation between adherence to the MeDi and MCI in- The potentially beneficial effect of the MeDi may be
cidence was similar for MCI with and without memory the result of some of its individual food components. For
impairment, whereas the protective MeDi effect for AD example, potentially beneficial effects for MCI or MCI
conversion was stronger for subjects who had MCI with- conversion to AD have been reported for alcohol,7,11 fish,10
out memory impairment. Vascular comorbidities, in- polyunsaturated fatty acids10,11 (also for age-related cog-
cluding diabetes, hypertension, dyslipidemia, and white nitive decline8), and lower levels of saturated fatty ac-
matter abnormalities, have been related to MCI,38-48 and ids.10 Interestingly, in other studies, alcohol,7,12 polyun-
it has been proposed that nonamnestic MCI in particu- saturated fatty acids,6 or other nutrients such as vitamin
lar may be related to cerebrovascular disease.36,37,49 There E93,94 have failed to be associated with protection for MCI
is increasing recognition of vascular comorbidity regard- or MCI conversion to AD. Differences in the definition
ing AD risk,50,51 and there is strong evidence relating the of the outcome (MCI [objective cognitive cutoffs in dif-
MeDi to a lower risk of vascular risk factors such as dys- ferent cognitive domains⫹memory complaint⫹absence
lipidemia,52,53 hypertension,52-55 and coronary heart dis- of functional impairment⫹absence of dementia] vs age-
ease.3,53,56,57 Therefore, the stronger effect of the MeDi for related cognitive decline [only a particular cognitive cut-
non-memory-impaired MCI conversion rates to AD may off on a summary cognitive score such as the Mini-
relate to underlying vascular mechanisms. Neverthe- Mental State Examination]) may partly account for the
less, nonvascular biological mediating mechanisms (ie, discrepancies. Nevertheless, it is also possible that a com-
metabolic, oxidative, and inflammatory) may also me- posite dietary pattern such as the MeDi may better cap-
diate the epidemiological MeDi-MCI associations.4 ture nutritional dimensions that may be missed by single
Both MCI and the MeDi have been associated with nutrients (ie, potential additive and interactive effects
metabolic abnormalities. Mild cognitive impairment has among nutritional components).
been linked to dysregulation of glucose and insulin ho- Although Hispanic subjects reported higher adher-
meostasis58-62 and diabetes.38-42 At the same time, accord- ence to the MeDi, they also have higher risks for MCI14
ing to the vast majority of the literature (but see the ar- and AD.95 A particular ethnic group may have a mixture
ticles by Ambring et al63 and Michalsen et al64), higher of multiple protective and risk factors, the overall inter-
adherence to the MeDi seems to improve carbohydrate action of which determines the probability of develop-
metabolism, and in interventional studies it has been as- ing a complex disease such as AD. For example, the His-
sociated with significant reductions in plasma glucose lev- panic subjects may be placed at risk by their low education
els,53,55 serum insulin levels, and insulin resistance.55,65 and SORL1 gene status,96 whereas they may be pro-
Oxidative stress could be another biological mecha- tected by their dietary habits and lack of a detrimental
nism relating MCI and the MeDi. Higher oxidative stress effect of the APOE genotype.95 At the same time, there
has been clearly invoked in MCI.66-71 Complex phenols may be multiple other genes or behavioral traits unique
and many other substances with important antioxidant to the Hispanic subjects that may contribute to AD, re-
properties such as olive oil,72,73 wine, fruits and veg- sulting in an overall higher risk in this ethnic group.
etables, vitamin C, vitamin E, and carotenoids74-79 are Study limitations regarding duration of follow-up and
found in high concentrations in the typical components demographics of subjects with either missing data for MCI
of the MeDi.80 Typical Mediterranean meals81 or meals diagnostic assignment or missing follow-up have been dis-
rich in typical Mediterranean food elements82,83 have been cussed in detail in a previous article.14 Subjects excluded
shown to increase enzymes with antioxidant properties from the present analyses because of missing dietary in-
such as paroxonase and plasma carotenoids.81 Interven- formation had slightly lower cognitive performance, were
tion studies with Mediterranean-type foods have indi- less educated, and had higher BMIs. Worse cognition and
cated significant reductions of markers of oxidative stress a lower educational level indicate that these subjects were
such as isoprostanes.80,84 more likely at higher risk for MCI and AD, but a higher
Finally, the protective effect of the MeDi for MCI may BMI indicates the opposite. Most important, these sub-
be mediated via inflammatory pathways. Links between jects did not differ in most other characteristics. Potential
MCI and higher inflammatory states have been demon- confounding from associations between adherence to the
strated.85-89 Two small studies reported no effect of the MeDi and total caloric intake or ethnicity was addressed
MeDi on inflammatory markers such as C-reactive pro- by adjusting for these factors. Limitations relating to the
tein63,64 or interleukin 6.63 Higher adherence to the MeDi construction of the MeDi score (eg, use of an a priori di-
has been associated with lower levels of C-reactive pro- etary pattern score, equal weighing of underlying food cat-
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
222
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.egories, and underestimation of total food and caloric in- complete and convincing picture of the conceivably im-
take) have been discussed in detail in previous articles.4,5 portant role of a healthy diet in the risk of cognitive im-
All of the models were adjusted for total caloric intake pairment and AD.
(largely determined by metabolic efficiency, BMI, and physi-
cal activity). Given that metabolic efficiency is unmeasur-
able and that BMI was included as a covariate, when we Accepted for Publication: September 3, 2008.
adjust for total caloric intake we essentially adjust for physi- Correspondence: Nikolaos Scarmeas, MD, Columbia Uni-
cal activity.30 Nevertheless, we cannot completely ex- versity Medical Center, 622 W 168th St, PH 19th Floor,
clude the possibility that physical activity may partly ac- New York, NY 10032 (ns257@columbia.edu).
count for some of the effect of the MeDi. Although Author Contributions: Study concept and design: Scarmeas,
adherence to the MeDi was not related to education or to Manly, and Luchsinger. Acquisition of data: Scarmeas,
the overall level of medical comorbidities in our data, it is Stern, Mayeux, and Manly. Analysis and interpretation of
possible that a better diet is related to higher socioeco- data: Scarmeas, Schupf, and Luchsinger. Drafting of the
nomic status or to other habits or characteristics related manuscript: Scarmeas and Luchsinger. Critical revision of
to better health. Therefore, despite adjusting for multiple the manuscript for important intellectual content: Stern,
variables, the study is observational and we cannot com- Mayeux, Manly, and Schupf. Statistical analysis: Scarmeas.
pletely exclude residual confounding or “healthy person Obtained funding: Mayeux, Manly, Schupf, and Luchsinger.
bias” (that can be addressed only via the randomization Administrative, technical, and material support: Stern,
of an interventional study). In conservative (for the study Mayeux, Manly, and Schupf. Study supervision: Scarmeas.
size and follow-up) models using age as the timing vari- Financial Disclosure: None reported.
able of survival models, the associations were signifi- Funding/Support: This work was supported by grants
cantly attenuated. Although age was not related to the AG028506, P01-AG07232, and RR00645 from the Na-
MeDi, we cannot completely exclude the possibility that tional Institute on Aging.
the noted associations are confounded by age. Finally, be-
cause the current study started before the concept of MCI REFERENCES
was developed, diagnosis of MCI was retrospectively ap-
plied in data that had already been collected (rather than 1. Luchsinger JA, Mayeux R. Dietary factors and Alzheimer’s disease. Lancet Neurol.
2004;3(10):579-587.
being applied synchronously with the diagnostic consen- 2. Luchsinger JA, Noble JM, Scarmeas N. Diet and Alzheimer’s disease. Curr Neu-
sus conference). rol Neurosci Rep. 2007;7(5):366-372.
Because of the synchronous timing of dietary and cog- 3. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediter-
nitive assessments and the relatively short follow-up, we ranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):
cannot completely exclude reverse causation (ie, di- 2599-2608.
4. Scarmeas N, Stern Y, Mayeux R, Luchsinger JA. Mediterranean diet, Alzheimer
etary habits being affected by cognitive status rather than disease, and vascular mediation. Arch Neurol. 2006;63(12):1709-1717.
the opposite). Nevertheless, in 2 previous articles4,5 using 5. Scarmeas N, Stern Y, Tang MX, Mayeux R, Luchsinger JA. Mediterranean diet
a subset of 390 subjects with repeated (2-4) dietary as- and risk for Alzheimer’s disease. Ann Neurol. 2006;59(6):912-921.
sessments over a course of approximately 8 (and up to 6. Solfrizzi V, Colacicco AM, D’Introno A, et al. Dietary fatty acids intakes and rate
of mild cognitive impairment: the Italian Longitudinal Study on Aging. Exp Gerontol.
13) years, we demonstrated that adherence to the MeDi 2006;41(6):619-627.
is remarkably stable over time. Therefore, we consider 7. Solfrizzi V, D’Introno A, Colacicco AM, et al. Alcohol consumption, mild cognitive
it more likely that the reported MeDi adherence reflects impairment, and progression to dementia. Neurology. 2007;68(21):1790-1799.
our population’s longstanding dietary habits. Finally, be- 8. Solfrizzi V, Panza F, Torres F, et al. High monounsaturated fatty acids intake pro-
cause this is the first study to our knowledge demon- tects against age-related cognitive decline. Neurology. 1999;52(8):1563-1569.
9. Panza F, Solfrizzi V, Colacicco AM, et al. Mediterranean diet and cognitive decline.
strating an association between the MeDi and MCI, rep- Public Health Nutr. 2004;7(7):959-963.
lication in other populations is necessary. 10. Eskelinen MH, Ngandu T, Helkala EL, et al. Fat intake at midlife and cognitive
Confidence in our findings is strengthened by the fol- impairment later in life: a population-based CAIDE study. Int J Geriatr Psychiatry.
lowing factors. The study is community-based and the 2008;23(7):741-747.
11. Anttila T, Helkala EL, Viitanen M, et al. Alcohol drinking in middle age and sub-
population is multiethnic, increasing the external valid- sequent risk of mild cognitive impairment and dementia in old age: a prospec-
ity of the findings. Dietary data were collected with an in- tive population based study. BMJ. 2004;329(7465):539.
strument that has been previously validated and has been 12. Espeland MA, Gu L, Masaki KH, et al. Association between reported alcohol in-
used widely in epidemiological studies. The diagnosis of take and cognition: results from the Women’s Health Initiative Memory Study.
MCI and AD took place in a university hospital with ex- Am J Epidemiol. 2005;161(3):228-238.
13. Manly JJ, Bell-McGinty S, Tang MX, Schupf N, Stern Y, Mayeux R. Implement-
pertise in such disorders and was based on comprehen- ing diagnostic criteria and estimating frequency of mild cognitive impairment in
sive assessments and standard research criteria. The pa- an urban community. Arch Neurol. 2005;62(11):1739-1746.
tients were followed up prospectively at relatively short 14. Manly JJ, Tang MX, Schupf N, Stern Y, Vonsattel JP, Mayeux R. Frequency and
intervals. Measures for multiple potential confounders were course of mild cognitive impairment in a multiethnic community. Ann Neurol.
2008;63(4):494-506.
carefully recorded and adjusted for in the analyses. 15. Scarmeas N, Levy G, Tang MX, Manly J, Stern Y. Influence of leisure activity on
Overall, the effects of dietary habits in MCI have not the incidence of Alzheimer’s disease. Neurology. 2001;57(12):2236-2242.
been adequately explored. These results provide sup- 16. Golden RR, Teresi JA, Gurland BJ. Development of indicator scales for the Com-
port that MeDi-type habits may affect risk for both de- prehensive Assessment and Referral Evaluation (CARE) interview schedule.
veloping MCI and MCI conversion to AD. Possible bio- J Gerontol. 1984;39(2):138-146.
17. Gurland B, Kuriansky J, Sharpe L, Simon R, Stiller P, Birkett P. The Comprehen-
logical mechanisms underlying this association remain sive Assessment and Referral Evaluation (CARE): rationale, development and
to be investigated. Exploration of such mechanisms and reliability. Int J Aging Hum Dev. 1977;8(1):9-42.
potential future interventional studies will provide a more 18. Stern Y, Andrews H, Pittman J, et al. Diagnosis of dementia in a heterogeneous
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
223
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.population: development of a neuropsychological paradigm-based diagnosis of brain morphologic correlates of mild cognitive impairment in the National Heart,
dementia and quantified correction for the effects of education. Arch Neurol. 1992; Lung, and Blood Institute Twin Study. Arch Neurol. 2001;58(4):643-647.
49(5):453-460. 48. Wolf H, Ecke GM, Bettin S, Dietrich J, Gertz HJ. Do white matter changes contrib-
19. Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for ute to the subsequent development of dementia in patients with mild cognitive im-
the staging of dementia. Br J Psychiatry. 1982;140:566-572. pairment? a longitudinal study. Int J Geriatr Psychiatry. 2000;15(9):803-812.
20. American Psychiatric Association. Diagnostic and Statistical Manual of Mental 49. Gauthier S, Reisberg B, Zaudig M, et al. Mild cognitive impairment. Lancet. 2006;
Disorders. 3rd ed, revised. Washington, DC: American Psychiatric Association; 367(9518):1262-1270.
1987. 50. Breteler MM. Vascular risk factors for Alzheimer’s disease: an epidemiologic
21. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical perspective. Neurobiol Aging. 2000;21(2):153-160.
diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group un- 51. Luchsinger JA, Mayeux R. Cardiovascular risk factors and Alzheimer’s disease.
der the auspices of Department of Health and Human Services Task Force on Curr Atheroscler Rep. 2004;6(4):261-266.
Alzheimer’s Disease. Neurology. 1984;34(7):939-944. 52. Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C. Adherence
22. Petersen RC, Doody R, Kurz A, et al. Current concepts in mild cognitive impairment. to the Mediterranean diet attenuates inflammation and coagulation process in
Arch Neurol. 2001;58(12):1985-1992. healthy adults: the ATTICA Study. J Am Coll Cardiol. 2004;44(1):152-158.
23. Blessed G, Tomlinson BE, Roth M. The association between quantitative mea- 53. Singh RB, Dubnov G, Niaz MA, et al. Effect of an Indo-Mediterranean diet on pro-
sures of dementia and of senile change in the cerebral grey matter of elderly gression of coronary artery disease in high risk patients (Indo-Mediterranean Diet
subjects. Br J Psychiatry. 1968;114(512):797-811. Heart Study): a randomised single-blind trial. Lancet. 2002;360(9344):1455-1461.
24. Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cog- 54. Psaltopoulou T, Naska A, Orfanos P, Trichopoulos D, Mountokalakis T, Tricho-
nitive impairment: clinical characterization and outcome. Arch Neurol. 1999; poulou A. Olive oil, the Mediterranean diet, and arterial blood pressure: the Greek
56(3):303-308. European Prospective Investigation into Cancer and Nutrition (EPIC) study. Am
25. Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semi- J Clin Nutr. 2004;80(4):1012-1018.
quantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51-65. 55. Esposito K, Marfella R, Ciotola M, et al. Effect of a Mediterranean-style diet on
26. Luchsinger JA, Tang MX, Shea S, Mayeux R. Caloric intake and the risk of Alz- endothelial dysfunction and markers of vascular inflammation in the metabolic
heimer disease. Arch Neurol. 2002;59(8):1258-1263. syndrome: a randomized trial. JAMA. 2004;292(12):1440-1446.
27. Luchsinger JA, Tang MX, Shea S, Mayeux R. Antioxidant vitamin intake and risk 56. de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterra-
of Alzheimer disease. Arch Neurol. 2003;60(2):203-208. nean diet, traditional risk factors, and the rate of cardiovascular complications
28. Luchsinger JA, Tang MX, Siddiqui M, Shea S, Mayeux R. Alcohol intake and risk after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation.
of dementia. J Am Geriatr Soc. 2004;52(4):540-546. 1999;99(6):779-785.
29. Scarmeas N, Luchsinger JA, Mayeux R, Stern Y. Mediterranean diet and Alzhei- 57. Knoops KT, de Groot LC, Kromhout D, et al. Mediterranean diet, lifestyle factors,
mer disease mortality. Neurology. 2007;69(11):1084-1093. and 10-year mortality in elderly European men and women: the HALE project.
30. Willett W, Stampfer M. Implications of total energy intake for epidemiological JAMA. 2004;292(12):1433-1439.
analyses. In: Willett W, ed. Nutritional Epidemiology. New York, NY: Oxford Uni- 58. Odetti P, Piccini A, Giliberto L, et al. Plasma levels of insulin and amyloid beta 42
versity Press; 1998:273-301. are correlated in patients with amnestic mild cognitive impairment. J Alzhei-
31. Kuczmarski RJ, Carroll MD, Flegal KM, Troiano RP. Varying body mass index mers Dis. 2005;8(3):243-245.
cutoff points to describe overweight prevalence among U.S. adults: NHANES III 59. Reger MA, Watson GS, Green PS, et al. Intranasal insulin administration dose-
(1988 to 1994). Obes Res. 1997;5(6):542-548. dependently modulates verbal memory and plasma amyloid-beta in memory-
32. US Census Bureau. Census of Population and Housing Summary Tape File 1: impaired older adults. J Alzheimers Dis. 2008;13(3):323-331.
Technical Documentation. Washington, DC: US Census Bureau; 1991. 60. Reger MA, Watson GS, Green PS, et al. Intranasal insulin improves cognition
33. Scarmeas N, Brandt J, Albert M, et al. Delusions and hallucinations are associated and modulates beta-amyloid in early AD. Neurology. 2008;70(6):440-448.
with worse outcome in Alzheimer disease. Arch Neurol. 2005;62(10):1601-1608. 61. Watson GS, Cholerton BA, Reger MA, et al. Preserved cognition in patients with
34. Scarmeas N, Albert M, Brandt J, et al. Motor signs predict poor outcomes in Alz- early Alzheimer disease and amnestic mild cognitive impairment during treat-
heimer disease. Neurology. 2005;64(10):1696-1703. ment with rosiglitazone: a preliminary study. Am J Geriatr Psychiatry. 2005;
35. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying 13(11):950-958.
prognostic comorbidity in longitudinal studies: development and validation. 62. Zhao Z, Xiang Z, Haroutunian V, Buxbaum JD, Stetka B, Pasinetti GM. Insulin
J Chronic Dis. 1987;40(5):373-383. degrading enzyme activity selectively decreases in the hippocampal formation
36. Petersen RC. Mild cognitive impairment: current research and clinical implications. of cases at high risk to develop Alzheimer’s disease. Neurobiol Aging. 2007;
Semin Neurol. 2007;27(1):22-31. 28(6):824-830.
37. Luis CA, Loewenstein DA, Acevedo A, Barker WW, Duara R. Mild cognitive im- 63. Ambring A, Johansson M, Axelsen M, Gan L, Strandvik B, Friberg P. Mediterranean-
pairment: directions for future research. Neurology. 2003;61(4):438-444. inspired diet lowers the ratio of serum phospholipid n-6 to n-3 fatty acids, the
38. Yaffe K, Blackwell T, Whitmer RA, Krueger K, Barrett Connor E. Glycosylated he- number of leukocytes and platelets, and vascular endothelial growth factor in
moglobin level and development of mild cognitive impairment or dementia in healthy subjects. Am J Clin Nutr. 2006;83(3):575-581.
older women. J Nutr Health Aging. 2006;10(4):293-295. 64. Michalsen A, Lehmann N, Pithan C, et al. Mediterranean diet has no effect on
39. Yaffe K, Krueger K, Cummings SR, et al. Effect of raloxifene on prevention of markers of inflammation and metabolic risk factors in patients with coronary ar-
dementia and cognitive impairment in older women: the Multiple Outcomes of tery disease. Eur J Clin Nutr. 2006;60(4):478-485.
Raloxifene Evaluation (MORE) randomized trial. Am J Psychiatry. 2005;162 65. Jula A, Marniemi J, Huupponen R, Virtanen A, Rastas M, Rönnemaa T. Effects
(4):683-690. of diet and simvastatin on serum lipids, insulin, and antioxidants in hypercho-
40. Yaffe K, Blackwell T, Kanaya AM, Davidowitz N, Barrett-Connor E, Krueger K. lesterolemic men: a randomized controlled trial. JAMA. 2002;287(5):598-605.
Diabetes, impaired fasting glucose, and development of cognitive impairment in 66. Butterfield DA, Sultana R. Redox proteomics identification of oxidatively modi-
older women. Neurology. 2004;63(4):658-663. fied brain proteins in Alzheimer’s disease and mild cognitive impairment: in-
41. Das SK, Bose P, Biswas A, et al. An epidemiologic study of mild cognitive im- sights into the progression of this dementing disorder. J Alzheimers Dis. 2007;
pairment in Kolkata, India. Neurology. 2007;68(23):2019-2026. 12(1):61-72.
42. Luchsinger JA, Reitz C, Patel B, Tang MX, Manly JJ, Mayeux R. Relation of dia- 67. Ding Q, Dimayuga E, Keller JN. Oxidative damage, protein synthesis, and protein
betes to mild cognitive impairment. Arch Neurol. 2007;64(4):570-575. degradation in Alzheimer’s disease. Curr Alzheimer Res. 2007;4(1):73-79.
43. Solomon A, Kareholt I, Ngandu T, et al. Serum cholesterol changes after midlife 68. Keller JN, Schmitt FA, Scheff SW, et al. Evidence of increased oxidative damage
and late-life cognition: twenty-one-year follow-up study. Neurology. 2007;68 in subjects with mild cognitive impairment. Neurology. 2005;64(7):1152-1156.
(10):751-756. 69. Lovell MA, Markesbery WR. Oxidative damage in mild cognitive impairment and
44. Tervo S, Kivipelto M, Hanninen T, et al. Incidence and risk factors for mild cog- early Alzheimer’s disease. J Neurosci Res. 2007;85(14):3036-3040.
nitive impairment: a population-based three-year follow-up study of cognitively 70. Mecocci P. Oxidative stress in mild cognitive impairment and Alzheimer dis-
healthy elderly subjects. Dement Geriatr Cogn Disord. 2004;17(3):196-203. ease: a continuum. J Alzheimers Dis. 2004;6(2):159-163.
45. Lopez OL, Jagust WJ, Dulberg C, et al. Risk factors for mild cognitive impair- 71. Rinaldi P, Polidori MC, Metastasio A, et al. Plasma antioxidants are similarly de-
ment in the Cardiovascular Health Study Cognition Study: part 2. Arch Neurol. pleted in mild cognitive impairment and in Alzheimer’s disease. Neurobiol Aging.
2003;60(10):1394-1399. 2003;24(7):915-919.
46. DeCarli C. Mild cognitive impairment: prevalence, prognosis, aetiology, and 72. Fitó M, Cladellas M, de la Torre R, et al. Antioxidant effect of virgin olive oil in
treatment. Lancet Neurol. 2003;2(1):15-21. patients with stable coronary heart disease: a randomized, crossover, con-
47. DeCarli C, Miller BL, Swan GE, Reed T, Wolf PA, Carmelli D. Cerebrovascular and trolled, clinical trial. Atherosclerosis. 2005;181(1):149-158.
(REPRINTED) ARCH NEUROL / VOL 66 (NO. 2), FEB 2009 WWW.ARCHNEUROL.COM
224
Downloaded from www.archneurol.com at New York State Psychiatric Institute, on May 17, 2010
©2009 American Medical Association. All rights reserved.You can also read