Challenges and Opportunities for Diabetes Prevention - Listening to Public Health Professionals and Partners in Minnesota
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Challenges and
Opportunities for
Diabetes Prevention
Listening to Public Health
Professionals and Partners
in Minnesota
Facilitated by the Minnesota Department of Health
and the Minnesota Diabetes ProgramChallenges and Opportunities for Diabetes Prevention
Challenges and Opportunities for Diabetes Prevention:
Listening to Public Health Professionals and Partners in Minnesota
Financial support was provided through a
Cooperative Agreement (U32/CCU500347) with the
Centers for Disease Control and Prevention (CDC)
This report was developed by the Minnesota Diabetes Program (MDP)
at the Minnesota Department of Health
For more information, contact:
Minnesota Diabetes Program
Minnesota Department of Health
PO Box 64882
85 East 7th Place, Suite 400
St. Paul, MN 55164-0882
651-201-5435
Website: http://www.health.state.mn.us/diabetes
Suggested Citation:
Minnesota Diabetes Program (2006). Challenges and Opportunities for Diabetes Prevention: Listening
to Public Health Professionals and Partners in Minnesota. St. Paul, Minnesota: Minnesota Department
of Health.
Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
Executive Summary
One in 5 Minnesotans is at high risk of developing diabetes. One in three infants born in the U.S.
during the year 2000 will develop diabetes during their lifetime. But diabetes can be delayed or
prevented. In September 2004, the Minnesota Diabetes Program (MDP) completed the Minnesota
Diabetes Prevention Planning Project (MN-DPPP). The MN-DPPP offered a timely opportunity to
strengthen the diabetes prevention theme in the Minnesota Diabetes Plan 2010 (the Plan), launched in
October 2003.
More than 50 diabetes prevention stakeholders contributed their expertise to the MN-DPPP, while over
350 diabetes stakeholders from across the state participated in developing the Plan recommendations.
This report summarizes the results of the MN-DPPP for Minnesota stakeholders and brings those
results together with the prevention-related recommendations from the Plan, to provide a vision
and a call to action for diabetes prevention in Minnesota that is grounded in the expertise of a broad
spectrum of diabetes stakeholders (Table 1). This document also summarizes the MN-DPPP’s impact
since completion, along with recent developments and opportunities for diabetes prevention in
Minnesota.
MN-DPPP participants cited roles in diabetes prevention for government, private industry, health care
systems, health care providers and communities. Roles were diverse and overlapping, suggesting the
importance of partnerships. The most important resources needed were: leadership, funding, staff,
data and expertise. Policy changes were recommended in four areas: health care, schools, worksites,
and the built environment.
The MN-DPPP identified important tensions among four key issues: 1) the boundaries of scientific
evidence for diabetes prevention; 2) enthusiasm or “pent-up demand” among our partners; 3) the
realities of collaborative practice; and 4) scarce resources for prevention. The biggest challenge remains
determining an appropriate scope for diabetes prevention efforts. Research has demonstrated that
diabetes can be prevented or delayed among those who are glucose intolerant, overweight or obese, and
25 years or older. But a tension exists between this evidence and the pragmatic realities of engaging
diverse partners, especially communities, who prefer a broader target audience. Efforts seeking to
maximize broad organizational participation need to balance these different perspectives.
Collaboration for prevention was cited as an important potential benefit of diabetes prevention. MN-
DPPP participants expressed great enthusiasm for “moving upstream” and shared optimism that
collaboration to address risk factors will create synergy and leverage resources. However, many pointed
out that in practice, collaboration itself requires resources, especially time, and that both strategies and
resources are needed for motivating potential partners to come to the table. Securing adequate and
stable resources will be critical to diabetes prevention efforts.
Challenges and Opportunities for Diabetes Prevention
Since this project was completed in 2004, a number of actions are underway, influenced to various degrees
by the MN-DPPP. MDH has hired a chronic disease epidemiologist, begun a workplace wellness initiative
and used the MN-DPPP results to argue for continued chronic disease prevention funding. In addition, new
funding has come through two CDC grants: Steps to a Healthier U.S. and the Diabetes Primary Prevention
Initiative (DPPI). Several new diabetes prevention measures have been piloted in Minnesota’s Behavioral
Risk Factor Surveillance Survey (BRFSS). The Minnesota Diabetes Steering Committee has formed a work
group to address diabetes prevention, which will incorporate MN-DPPP recommendations into their work.
Participants strongly emphasized that any new diabetes prevention work should build on existing efforts,
and there are several opportunities for such collaboration in Minnesota, including: Steps to a Healthier
U.S.; Indian Health Service prevention grants and prediabetes guidelines; the Blue Cross Blue Shield dou
campaign to promote everyday physical activity; the American Diabetes Association’s work with members of
the Minnesota business community; the Fit City and Fit School award programs; federally mandated school
wellness policies; the Minnesota Child Obesity Task Force; the newly released Eagle Books, which aim to
prevent diabetes in American Indian youth; worksite wellness strategies being piloted at the Minnesota
Department of Health, and local public health priorities for addressing obesity, nutrition and physical
activity.
We urge individuals, communities and organizations to take an active role in preventing the future burden
of diabetes and we look forward to engaging partners in taking action on diabetes prevention in Minnesota.
Table 1. Diabetes Prevention Goals, Recommendations and Potential Projects
Goal: Encourage Healthy Lifestyle Behaviors for Youth
Recommendations
• Work with state and local school officials to improve school policies and curricula-related issues impacting students’ health,
particularly those affecting physical education, nutrition education and food services
• Encourage communities to develop and implement community-based recreation programs for youth, which provide opportunities for
physical activity and healthy eating
Potential Projects
• Promote awareness of the Action for Healthy Kids (AFHK) guidelines for healthy school food environments
• Survey schools on policies and curricula that affect students’ eating and physical activity
Goal: Create Healthier Environments
Recommendations
• Work with state and local community partners to identify and implement changes in the built environment and community policies
that will facilitate healthy lifestyle behaviors
• Develop relationships with industries that impact diabetes risk, such as fast food and soda producers and vending machine
operators, and influence them to improve their products
• Work with employers and business partners to improve worksite health promotion policies, such as providing showers at workplaces
and time off for physical activity
• Promote or provide access and address barriers to physical activities
Potential Projects
• Improve signage for shared walking and biking paths in communities
• Work with employers to improve work place environments to support healthy lifestyle choices
• Design physical activity promotions that build on new immigrants’ traditional activities to help increase their activity levels
Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
Table 1. Diabetes Prevention Goals, Recommendations and Potential Projects
Goal: Maximize and Effectively Use Diabetes Resources
Recommendations
• Identify and provide incentives to collaborate and share resources for diabetes prevention
• Secure adequate and stable resources for diabetes prevention
• Provide prevention funding to local communities
Potential Projects
• Cultivate relationships with the private sector and make an effective business case for investments in prevention
• Work with advocacy organizations to lobby state and federal legislators to increase funding for diabetes prevention
• Make collaboration part of position descriptions and annual reviews at the Minnesota Department of Health
Goal: Create Political Capital for Diabetes Prevention
Recommendations
• Build support for diabetes legislative action, including prevention resources
• Advocate for health insurance benefit structures that reward healthy behaviors
• Make a persuasive cost/benefit case for putting resources toward prevention
Potential Projects
• Convene a forum on diabetes prevention with Minnesota employers, purchasers, insurers, providers and policymakers
• Create a bipartisan chronic disease prevention advocacy group (legislative caucus)
Goal: Raise Public Awareness about Diabetes Care and Prevention
Recommendations
• Implement public awareness campaigns to promote healthy lifestyle behaviors, with these characteristics:
o simple, consistent messages
o cutting edge communications and marketing strategies
o tailored to specific audiences
o sustained over time
Potential Projects
• Conduct diabetes prevention awareness campaigns focused on:
o high-risk groups
o policy makers
o business sector, and
o the general public
Goal: Foster Community-Based Collaboration and Communication
Recommendations
• Convene forums, coordinate communication and strategies, align and focus goals, leverage resources and foster collaboration
among programs, organizations and communities motivated to address diabetes prevention and chronic disease risk factors
• Support community-based programs to prevent diabetes and reduce chronic disease risk factors in Minnesota utilizing effective
strategies
Potential Projects
• Develop a chronic disease fact sheet
• Publish a quarterly bulletin focused on chronic disease prevention
• Convene an annual conference focused on chronic disease prevention
• Develop a document describing intersections among statewide chronic disease plans
Goal: Integrate Diabetes Prevention into Health Systems
Recommendations
• Promote collaboration between community groups, health systems, and other stakeholders to prevent diabetes and improve
outcomes
• Create and build consensus for guidelines, standards, protocols and best practices for improving risk behaviors and risk factors as
well as prediabetes care
• Identify, flag, notify and refer those with high glucose levels and ensure adequate follow-up
• Implement programs to change behaviors and attitudes about diabetes prevention and management and empower people to stay
healthy, self-assess and ask for screening
Potential Projects
• Develop and validate practical models for prediabetes screening and treatment
• Translate the Diabetes Prevention Program lifestyle intervention from the context of a controlled research into real-world settings
• Ensure follow-up for women with pregnancies complicated by gestational diabetesChallenges and Opportunities for Diabetes Prevention
Introduction
Diabetes and obesity represent linked epidemics.1 Driven largely by increases in obesity, diabetes
prevalence in the U.S. is expected to grow by 165% in the next 50 years.2 One in three U.S. infants born
in the year 2000 will develop diabetes during their lifetime.3 Diagnosed diabetes in Minnesota has
increased nearly 50% in the last 10 years, from 3.8% in 1994 to 5.5% in 2003. One in 5 Minnesotans is at
high risk of developing diabetes. Diabetes multiplies the risk of heart disease two to four-fold and is the
leading cause of blindness, kidney failure, and lower-limb amputations in Minnesota. Diabetes is the
sixth leading cause of death and its direct and indirect costs to the state total an estimated $2.3 billion
annually.
And yet there is promising news: Diabetes can be delayed or prevented. Research has consistently
shown that physical activity reduces diabetes risk.4 Three independent, randomized, controlled trials
conducted in three different countries, China, Finland and the U.S., have shown that changes in
lifestyle can reduce diabetes risk.5-7 In the U.S., the Diabetes Prevention Program (DPP), showed that
diet, exercise and losing a little weight (about 10%) can reduce the risk of type 2 diabetes by 58% among
those at high risk.5 In the DPP, participants of all ages and ethnic groups were able to prevent or delay
type 2 diabetes with modest lifestyle changes.
The DPP also found that metformin reduced the incidence of diabetes by 31%.5 Along with metformin,
troglitazone, rosiglitazone, acarbose and orlistat have been shown to decrease the risk of progression
to diabetes.8, 9 However, pharmacological approaches may be less cost-effective, less likely to have
sustained benefits, more likely to induce serious side effects, and most useful for more targeted
segments of the population, such as those free of heart disease.10
The challenge is to translate the evidence from controlled trials into realistic clinical and population
health practices.
Background
In September 2003, the Minnesota Diabetes Program (MDP), along with five other states: Kansas,
Massachusetts, Michigan, North Carolina and Virginia, received funding to plan for diabetes
prevention. The MDP had recently launched the Minnesota Diabetes Plan 2010 (the Plan), our second
statewide strategic plan for diabetes. More than 350 diabetes stakeholders participated from across the
state, and more than two years (2001 – 2003) were invested in gathering their input and developing
the Plan’s goals and recommendations. But much of this work preceded publication of the DPP results.
Given this timing, the Minnesota Diabetes Prevention Planning Project (MN-DPPP) offered a timely
opportunity to strengthen the diabetes prevention focus in the Plan. However, we anticipated that
enthusiasm for additional planning efforts would be at low ebb among our partners, so we designed the
MN-DPPP to be focused on producing realistic, actionable projects to address diabetes prevention in
Minnesota.
Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
Our goal for the MN-DPPP was to learn from our partners. Our primary research questions were:
• What should be the scope of diabetes prevention efforts?
• Who should be involved in diabetes prevention and what are their roles?
• What resources are needed to implement diabetes prevention activities?
• What policies are needed to prevent diabetes?
• What are the barriers and how can they be overcome?
• How should we begin?
This report summarizes these results and the project’s impact since completion, along with recent
developments and opportunities for moving forward with diabetes prevention in Minnesota.
Methods
We conducted 14 interviews, held 6 focus groups and convened 3 working meetings with a total of 56
MDH staff, MDH managers and non-MDH partners (Table 1). We held interviews at participants’ place
of work; all other meetings took place at St. Paul MDH locations.
Table 1. Participation
State Department of Health Non-MDH Partners
Staff Managers Total
Interviews 5 4 5 14
Focus Groups
A 4 4 8 16
B 11 4 11 26
Total 20 12 24 56
We recruited participants for their knowledge, experience, organizational capacity and interest in
diabetes prevention. MDH programs represented a balance between management and staff and the
spectrum of chronic disease and prevention programs. Among non-MDH participants, both urban
and rural areas of the state and Minnesota’s diverse racial and ethnic communities were represented.
Appendix 1 lists participating organizations. Appendix 2 provides further details on data collection
and analysis.
A particularly important research question was the appropriate scope for a diabetes prevention
program. Thus, we asked participants to consider the following scenarios: 1) Prevention programs
targeting people with pre-diabetes (impaired fasting glucose or impaired glucose tolerance)11; and 2)
Programs targeting persons with one or more risk factor for diabetes, including age, overweight, race or
ethnicity, family history of diabetes, history of gestational diabetes, etc.12
Challenges and Opportunities for Diabetes Prevention
Results
Prominent themes in the interview and focus group results are summarized below, including those where
MDH staff, MDH managers and external partners had different views.
What should be the scope of diabetes prevention efforts?
Participants, particularly MDH staff and managers, emphasized the Table 2. Scope
need to clearly define the scope of diabetes prevention but differed
• Participants differed on appropriate
widely on the appropriate target audience for diabetes prevention
target audience:
(Table 2). MDH Managers and some non-MDH partners felt that, o High risk
given limited resources, efforts must target high-risk populations. o Children
However, many MDH staff and non-MDH partners tended to think of o Everyone
• Few clear differences between
diabetes prevention more broadly, to include the entire population—
prevention strategies for prediabetes
particularly primary prevention of obesity in children. vs. the general population
Table 3. Key Partners and Roles
In general, participants identified similar
Government strategies for diabetes prevention among those
• Promote reimbursement for prevention
with prediabetes and those with one or more
• Build public health infrastructure
• Promote physical activity risk factor. Even when we asked specifically
• Connect people with resources about differences between these two target
• Develop & support consistent diabetes prevention messages audiences, participants felt either that
• Promote guidelines
strategies would be similar, or that strategies
• Convene stakeholders & build partnerships
• Translate research for prediabetes might be more clinically
• Seek funding focused.
Private Industry
Who are the key partners who should be
• Fund public awareness campaigns
• Influence benefit structures involved in diabetes prevention; what are
• Reach people where they are their roles? Participants outlined roles for
a broad spectrum of partners (Table 3),
Health Care
including specific roles for government, private
• Advocate for reimbursement for prevention
• Create guidelines industry, health care, and communities. Roles
• Empower people to be healthy, self-assess and ask for were diverse and overlapping, suggesting the
screening importance of partnerships.
• Develop systems that support screening and referral
• Ensure support for newly diagnosed
Government was seen as a primary source
Communities of prevention resources, but participants
• Reach people where they are mentioned private industry as an additional
• Make prevention relevant
source of funds, especially for public awareness
• Ensure consistent diabetes prevention messages
• Promote physical activity campaigns. Other roles for private industry
• Connect people with self-care and health care resources included influencing benefit structures
• Empower people to be healthy, self-assess and ask for toward prevention, and providing avenues to
screening
reach people where they are, for example, at
• Ensure support for newly diagnosed
worksites or retail outlets.
Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
Roles for government, including the federal, state and local levels, were focused on providing
infrastructure and funding. Specific roles identified for MDP and MDH (hereafter “the state”)
focused on leadership and coordination. Participants felt the state should play the role of convener by
coordinating partners and organizing communities. Non-MDH partners particularly valued the state’s
capacity to organize forums and conferences. A key role for the state was to keep current on relevant
research, translate research into practice and provide successful models for community partners.
Participants also emphasized the importance of seeking input from diverse partners when designing a
diabetes prevention program, especially keeping health professionals “in the loop”.
Key partners for diabetes prevention within the MDH included heart disease and other chronic disease
programs; epidemiologists and analysts; health education, community health and health economics
programs; the MDH communications office; MDH library; MDH management and the Executive
Office. Participants emphasized working with a broad spectrum of internal partners to communicate,
collaborate and share resources.
MDH staff and non-MDH partners brought slightly different yet complimentary perspectives to
the discussion of the state’s role in diabetes prevention. MDH staff and managers emphasized
the importance of obtaining the Commissioner of Health’s support. With the support of MDH
management and the Commissioner, they felt that the MDP could more effectively advocate for
additional resources for diabetes prevention. Non-MDH partners valued the state’s population-based
approach. They also wanted MDH to seek funding for diabetes prevention.
Participants felt that health care systems and providers should advocate for investment in prevention,
including reimbursement structures that promote preventive care. They should create and promote
diabetes prevention guidelines, standards and protocols. They should design systems of care that
empower people to be healthy, self-assess their diabetes risk factors and ask for screening. In addition,
health care systems should develop protocols to identify, flag, notify and refer those with high glucose
levels. After screening, they should assure follow-up that connects people with the resources they need
to prevent or manage diabetes. Most importantly, they should provide support for behavior change
among those newly screened or diagnosed.
Participants suggested involving community members to ensure that diabetes prevention efforts are
relevant, effective and appropriately focused for real people. Communities should work to ensure
consistent prevention messages for the general public and for high-risk groups and seek funding to
sustain the messages. Communities have a role in providing access to physical activities and can also
connect people with the health care system and self-care resources. Communities can empower people
to self-assess their diabetes risk factors and ask their health providers for screening. Participants felt
that support for behavior change among those newly screened or diagnosed could also be community-
based.
Challenges and Opportunities for Diabetes Prevention
What resources are needed to
implement diabetes prevention Table 4. Resources Needed and Why
activities? • Leadership
Participants stressed the importance of o “Start the charge”
o Create and leverage political will
resources, and explained how they would help o Obtain resources
(Table 4). Strong leadership for prevention was o Bring people together
considered the most important resource: o Resolve priority conflicts
People who are influential, who could be
• Funding
leaders and be on your side, so to speak. o Enable community participation
Some people in the legislature, who are o Conducting evaluation to show effectiveness
behind your cause or people at state agency o Sustain programs
levels, who really believe that what you’re o Enable marketing
o Conduct needs assessment
doing should be done and want to make it a o Pay for staff
priority. –MDH Manager o Influence policy
o Providing local training and capacity building
Leadership was seen as an important catalyst
• Staff
that would be needed to create and leverage o Program coordinator/evaluator – convene partners;
political will and obtain resources to address the translate research
problem of preventing diabetes. Leadership was o Chronic disease epidemiologist – identify leverage
also needed to bring people together at the state points; bridge chronic disease programs
and community levels, create linkages between • Data
sectors and stakeholders and resolve priority o Identify prediabetes population
conflicts. o Assess the burden
o Demonstrate progress
o Build business case
After leadership, funding was seen as most
important: • Expertise
We need resources, at the state level for o Behavioral science - behavior change
coordinating training, capacity building o Clinical care - “buy-in” from medical community
o Economics - business case
at the local level, training for schools, o Communications - effective messages
implementation of effective programs, o Coordination - align expertise and resources
interacting with partners and building among partners; build trust and relationships
relationships, money for all those things. with diverse communities; translate successful
programs; and attract resources.
–MDH Manager
Participants felt stable funding was needed not only to sustain and evaluate programs but also to
enable broad participation and build partnerships with community organizations, which would be
crucial to any diabetes prevention effort. Participants said that stable funding would also help to show
effectiveness.
Staff positions and staff time were important resources that participants felt were needed, including
a program coordinator/evaluator and a chronic disease epidemiologist. A coordinator would convene
partners and learn what other programs and organizations are doing related to prevention. This staff
person could also become expert in what programs, interventions and tools are effective for diabetes
10 Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
prevention, and help translate prevention research into practice for communities. A chronic disease
epidemiologist would collect information and review research on the best leverage points to address
diabetes prevention. This staff person would also be knowledgeable about research that could bridge
between categorical chronic disease programs.
Staff time in general came across as a significant issue for participants. Participants frequently
mentioned coordination and pooling funds or efforts to stretch limited resources. However, they felt
that “synergy” could go only so far and should not be seen as a substitute for new resources to address
a significant new challenge. Many remarked that increasing demands on their time, as well as their
partners’ time, had the effect of limiting collaboration. These comments often came back to the topic
of funding.
“You can get a long ways with enthusiasm and volunteers, but ultimately, to reach people on
an individual level, what you need to do to try and get behavior changed, is influence policy,
and I think you need money to do that.” –MDH Staff
They stressed that asking partners—who also have loaded plates and limited resources—to volunteer
their time is not always an effective option:
“Bringing partners to the table from the community, we often ask them to do in-kind and
voluntary, but…[given] all the things they might be involved with, if they’re not going to
be compensated for their time at least to some small degree, they might be less likely to
participate.” –MDH Staff
“…[Our] partners…are in need of time efficiency and effective use of their time. They’re also
burning out, I think, in terms of the multitude of things they’re dealing with.” –MDH Manager
After staff time, participants felt that the most important resource was data, especially on surveillance,
program evaluation and cost-effectiveness. Data were seen as important to: identify prediabetes
population and assess the burden, “so that we know what is going on right now”; indicate what’s
working and not working and show progress, especially for initial efforts; build business case by
showing “a return on the health care dollar”; and “give advocates something to fight with” to increase
the investment in prevention.
“If you’re going to affect any policy changes, in the community and health system, you want
to know that this is something that works, but is affordable, and in the long term, it’s going
to be cost effective.” –Non-MDH Partner
Finally, participants felt that diabetes prevention called for particular expertise, for example, in
behavioral research, clinical care, economics and communications. A behavioral scientist would be able
to develop theory based-programs that lead to behavior change. An expert in clinical care could help
secure “buy-in” from the medical community. Someone with expertise in economics could help make
the business case. A communications expert could craft effective messages for the public or partners.
Additional skills that participants deemed important included the ability to align expertise and
11Challenges and Opportunities for Diabetes Prevention
resources among partners; build trust and relationships with diverse communities; spread successful
programs; and attract resources.
What policies are needed to prevent diabetes?
Participants recommended policy changes in four areas
Table 5. Policies Needed
(Table 5). School policy changes received the highest • Healthy lifestyles in schools
priority: o Healthy lifestyle/skills curricula
“I think we’re going to need programs in the school o Mandatory physical education
o Food service improvements
systems related to nutrition, exercise, obesity and
diabetes and those programs—if they ever existed— • Healthy built environment
have been slashed with budget cuts. But that’s going o Neighborhood safety
to be critical I think for this epidemic, to get that o Urban planning to promote active
lifestyles
funding back somehow.” –Non-MDH Partner
• Access to preventive health care
Secondly, participants emphasized policies that create o Coverage and reimbursement
healthy built environments: o No penalties for prediabetes
diagnosis
“…safer housing, safer neighborhoods, green spaces
for exercise…farmer’s markets….I think it’s going to • Healthy worksite policies
cost communities less and you get people connected. It o Incentives and support for physical
builds social capital enormously and building social activity and healthy eating
capital saves money.” –MDH Staff
Participants felt that changes to the built environment would have several benefits, including:
increased opportunities for healthy eating and physical activity; lowering diabetes risk; building social
capital; making prevention part of communities; and ultimately, saving money.
Health care access and reimbursement for prevention were also frequently mentioned as an important
area for policy change:
“Access—even within a health plan—to dietitian services is pretty abysmal in most cases,
even if you’re diagnosed. So to get access when you’re not diagnosed with anything, that’s a
huge problem.” –Non-MDH Partner
Finally, participants saw worksites as a venue for policy changes to prevent diabetes, and one
participant felt their employer set a good example:
“At [my employer] we have sick leave for fitness. People can improve sick time and they can
trade in [so many] dollars a year for health club memberships, home fitness equipment.”
–Non-MDH Partner
12 Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
What are the barriers to implementing a diabetes prevention program and how
can they be overcome?
Table 6 lists the most important barriers to diabetes prevention and strategies for overcoming them.
Rationales for the strategies are detailed below.
For participants, making a persuasive case for prevention
Table 6. Barriers and Strategies meant demonstrating program effectiveness and
effectively communicating successful programs. They
Barriers
• Inadequate resources also felt it would be helpful to emphasize the synergistic
• Thin evidence base effects of diabetes prevention efforts, such as reductions in
• Unclear mandate for prevention depression, cardiovascular disease and cancer.
• Complexity of prevention interventions
• Competing political and economic interests
“When the cost of the system as a whole becomes
primary then we’ll see that sort of collective action.”
Strategies for Overcoming Barriers –MDH Manager
• Making a persuasive case for prevention
• Creating supportive environments
Making the case also included identifying policymakers
• Specifying target audiences
• Integrating prediabetes care into health care who can be advocates for prevention. MDH managers also
• Building on existing resources and programs. felt that diabetes advocacy groups should expand their
• Rapid translation of new research roles and responsibilities to include prevention.
Participants felt that creating supportive environments
can influence individual behavior. This strategy included persuading insurers and employers to provide
incentives such as subsidized health club memberships or permission to use sick leave for exercise, and
motivating individual behavior change through success stories and practical suggestions.
“[Bring in] people who can say, “I lowered my blood glucose level by doing these things,” and
give examples of what it took to feel motivated to do it—using, tapping into that. Motivation
is a hard thing, especially when we live in a dark, cold place!” –MDH Staff
Non-MDH participants, in particular, emphasized the need to clearly specify target audiences and “go
to where the people are”. They also suggested working with vending machine operators and fast food
and soda manufacturers—industries that impact diabetes risk behaviors:
“PepsiCo changed. Their whole baked line of chips is their fastest growing product line right
now. They took out the trans fatty acids and it’s just become really popular. It was a huge
gamble for them, and they must have felt like it was important enough to try and obviously
they had to put resources into the development of that product, and PepsiCo is a big
company, so they can afford to do it.” –Non-MDH Partner
I think that some of those big companies are getting a lot smarter about understanding
the impact on the health care dollar and how they may play a role in it. But it’s basically
looking at how could we all pool our resources and work together, because there’s not any
one industry that is solely responsible for the epidemic of diabetes and…there’s not any one
industry that’s solely responsible for fixing it either. We all play a role in why it’s here and
we all have to play a role in dealing with it. –Non-MDH Partner
13Challenges and Opportunities for Diabetes Prevention
Integrating prediabetes care into health care was a strategy strongly put forward by non-MDH
participants.
“If you want [dibetes prevention] to be successful, change the health care system so that it
rewards identifying people earlier and putting them into some type of a lifestyle program.”
–Non-MDH Partner
They emphasized being clear about what prediabetes is and how it can be addressed. They also
suggested expanding the roles and responsibilities of health professionals to accommodate diabetes
prevention care.
“Nursing has a holistic theoretical framework. I think most of the public think nurses just
take care of sick people, but we were all educated to do more than that, and we haven’t had
opportunities…in most clinical settings. We just take care of sick people. But a lot of nursing
schools are going back to those roots again and looking at dusting off the holistic framework
and saying, “This is why we’re created.” We used to do nutrition and exercise and wellness
and stress reduction and—but nobody pays for that.” –Non-MDH Partner
“We tend to reserve nutrition information for dietitians only, and we need to rethink that.
There’s some nutrition information that other people can provide.” –Non-MDH Partner
Finally, all participants felt that an important strategy would be to build on existing resources and
programs by leveraging existing knowledge and relationships.
“So how can we use those programs so that we don’t reinvent the wheel, but we can make
them usable for the community?” –Non-MDH Partner
Some examples of this strategy were: leveraging common interests (such as reducing shared risk
factors), successful wellness programs, and MDH credibility with potential partners:
“Knowledge of the organizations or communities. Trust. A good reputation for MDH.
Hopefully, a history where organizations outside have dealt with MDH and feel like it’s a
good use of their time…[and] that they’ve gotten something out of the relationship in the
past.” –MDH Manager
14 Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
What objectives, indicators, benchmarks and outcomes are needed to assess
progress?
At working meetings, participants brainstormed and ranked objectives, indicators, benchmarks and
outcomes for a potential Minnesota Diabetes Prevention Program (Table 7).
Table 7. Top-Ranked Objectives, Indicators, Outcomes, and Benchmarks
Objectives for a Minnesota Diabetes Prevention Program
• Promote access to health care for those at risk for diabetes
• Collect data on those at risk for diabetes, evaluate programs & disseminate data
• Collaborate and effectively engage local communities
• Increase activity and improve diet in at risk populations
• Achieve cultural competency with an active role in recruitment; ensure diversity
Indicators
• Prevalence and incidence of diabetes and prediabetes including mortality and age of onset
• Risk factor data for prediabetes (age, weight, family history, lipids, glucose)
• Data that includes ethnicity/culture/race and geography
• Data on physical activity levels of Minnesotans of all ages
Performance Benchmarks
• Coordinated approach to working with health plans and worksites
• Coverage for nutrition, weight and exercise counseling
• Integrated monitoring system for prediabetes and its risk factors
• Decrease rate of obesity among children
• Increase in number of people making lifestyle changes
Outcomes
• Decrease/slowdown rate of obesity/overweight in children and adults
• Increase population awareness and screening risk factors, including family history
• Reduce diabetes incidence in sub-populations (Latinos, African Americans, Native Americans, African immigrants,
gestational diabetes)
• Integrated monitoring system for chronic disease risk factors in place
How should we begin to address diabetes prevention?
MN-DPPP participants created eight arenas of action and 19 specific projects within those arenas.
These projects reflected the major issues, themes and opportunities identified in the MN-DPPP results.
While diverse in scope and content, the projects were also intended to be concrete and actionable.
Some were designed to relate to or expand upon initiatives already being planned.
More than 50 diabetes prevention stakeholders contributed their expertise to the MN-DPPP, while over
350 diabetes stakeholders from across the state participated in developing the Plan recommendations.
These two planning initiatives produced goals, recommendations and strategies for diabetes prevention
based on expertise from diabetes stakeholders across the state. The smaller, more focused MN-DPPP
planning process echoed recommendations from the Plan, but brought added detail and depth to the
roles, resources, policy changes and challenges for diabetes prevention. Table 8 integrates results from
the MN-DPPP and the Plan, summarizing goals, recommendations and potential projects to address
15
diabetes prevention.Challenges and Opportunities for Diabetes Prevention
Table 8. Diabetes Prevention Goals, Recommendations and Potential Projects*
Goal: Encourage Healthy Lifestyle Behaviors for Youth
Recommendations
• Work with state and local school officials to improve school policies and curricula-related issues impacting students’ health,
particularly those affecting physical education, nutrition education and food services
• Encourage communities to develop and implement community-based recreation programs for youth, which provide
opportunities for physical activity and healthy eating
Potential Projects
• Promote awareness of the Action for Healthy Kids (AFHK) guidelines for healthy school food environments
• Survey schools on policies and curricula that affect students’ eating and physical activity
Goal: Create Healthier Environments
Recommendations
• Work with state and local community partners to identify and implement changes in the built environment and community
policies that will facilitate healthy lifestyle behaviors
• Develop relationships with industries that impact diabetes risk, such as fast food and soda producers and vending machine
operators, and influence them to improve their products
• Work with employers and business partners to improve worksite health promotion policies, such as providing showers at
workplaces and time off for physical activity
• Promote or provide access and address barriers to physical activities
Potential Projects
• Improve signage for shared walking and biking paths in communities
• Work with employers to improve work place environments to support healthy lifestyle choices
• Design physical activity promotions that build on new immigrants’ traditional activities to help increase their activity levels
Goal: Maximize and Effectively Use Diabetes Resources
Recommendations
• Identify and provide incentives to collaborate and share resources for diabetes prevention
• Secure adequate and stable resources for diabetes prevention
• Provide prevention funding to local communities
Potential Projects
• Cultivate relationships with the private sector and make an effective business case for investments in prevention
• Work with advocacy organizations to lobby state and federal legislators to increase funding for diabetes prevention
• Make collaboration part of position descriptions and annuals reviews at the Minnesota Department of Health
Goal: Create Political Capital for Diabetes Prevention
Recommendations
• Build support for diabetes legislative action, including prevention resources
• Advocate for health insurance benefit structures that reward healthy behaviors
• Make a persuasive cost/benefit case for putting resources toward prevention
Potential Projects
• Convene a forum on diabetes prevention with Minnesota employers, purchasers, insurers, providers and policymakers
• Create a bipartisan chronic disease prevention advocacy group (legislative caucus)
16 Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
Table 8. Diabetes Prevention Goals, Recommendations and Potential Projects*
Goal: Raise Public Awareness about Diabetes Care and Prevention
Recommendations
• Implement public awareness campaigns to promote healthy lifestyle behaviors, with these characteristics:
o simple, consistent messages
o cutting edge communications and marketing strategies
o tailored to specific audiences
o sustained over time
Potential Projects
• Conduct diabetes prevention awareness campaigns focused on:
o high-risk groups
o policy makers
o business sector, and
o the general public
Goal: Foster Community-Based Collaboration and Communication
Recommendations
• Convene forums, coordinate communication and strategies, align and focus goals, leverage resources and foster
collaboration among programs, organizations and communities motivated to address diabetes prevention and chronic
disease risk factors
• Support community-based programs to prevent diabetes and reduce chronic disease risk factors in Minnesota utilizing
effective strategies
Potential Projects
• Develop a chronic disease fact sheet
• Publish a quarterly bulletin focused on chronic disease prevention
• Convene an annual conference focused on chronic disease prevention
• Develop a document describing intersections among statewide chronic disease plans
Goal: Integrate Diabetes Prevention into Health Systems
Recommendations
• Promote collaboration between community groups, health systems, and other stakeholders to prevent diabetes and
improve outcomes
• Create and build consensus for guidelines, standards, protocols and best practices for improving risk behaviors and risk
factors as well as prediabetes care
• Identify, flag, notify and refer those with high glucose levels and ensure adequate follow-up
• Implement programs to change behaviors and attitudes about diabetes prevention and management and empower people
to stay healthy, self-assess and ask for screening
Potential Projects
• Develop and validate practical models for prediabetes screening and treatment
• Translate the DPP lifestyle intervention from the context of a controlled research into real-world settings
• Ensure follow-up for women with pregnancies complicated by gestational diabetes
*Minnesota Diabetes Program staff created Table 8 based on the overlap between the MN-DPPP results and the prevention-related Plan
recommendations (Appendix 3). Table 8 has also been reviewed and validated by outside stakeholders.
17Challenges and Opportunities for Diabetes Prevention
Discussion
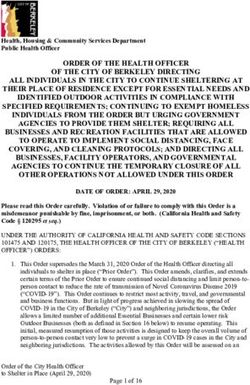
Figure 1
The MN-DPPP identified important tensions among
four key issues: 1) the boundaries of scientific
evidence for diabetes prevention; 2) enthusiasm
or “pent-up demand” for prevention among our
partners; 3) the realities of collaboration in practice;
and 4) scarce resources for prevention (Figure 1).
Science. Determining an appropriate scope for
diabetes prevention remains a challenge. The DPP
demonstrated that diabetes can be prevented or
delayed among those who are glucose intolerant,
overweight or obese and 25 years or older. But
a tension exists between this evidence and the
pragmatic realities of engaging diverse partners, especially communities, who prefer a broader target
audience. Efforts seeking to maximize broad organizational participation need to balance these
different perspectives.
Enthusiasm. Collaboration for prevention was cited as an important potential benefit of diabetes
prevention. Participants expressed great enthusiasm for “moving upstream” and shared optimism that
collaboration to address risk factors will create synergy and leverage resources.
“What might be unique about diabetes prevention is targeting those specific groups that
are at special risk for diabetes. But by doing it well, it becomes a model that could then be
adapted for the rest of the population as well. So I think there’s a real opportunity for a
leadership role, in the diabetes prevention program, in terms of how we address obesity and
physical activity.” ~ MDH Manager
Practice. Participants pointed out that in practice, collaboration itself requires resources, especially
time, and that both strategies and resources are needed for motivating potential partners to come to
the table. Existing workloads tend to crowd out collaboration as a priority and participants expressed
frustration about being asked to do more with less, as well as redundancy in efforts.
Resources. Having adequate and stable resources is critical. A non-MDH participant stated simply:
“Resources to do what has been prescribed by the science of the diabetes prevention trial are…
beyond our imagination.” However, since this study was completed, a cost-effectiveness analysis
of the DPP interventions found that, compared with metformin, the lifestyle intervention cost less
($1,100 vs. $31,300 per QALY, or quality adjusted life year) and yielded better outcomes. The authors
cited previous research suggesting that interventions that cost less than $20,000 per QALY are an
appropriate use of resources. This research argues strongly in favor of implementing DPP-style lifestyle
interventions with people at high risk of developing diabetes.10
18 Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramListening to Public Health Professionals and Partners in Minnesota
Actions Underway. The MN-DPPP’s impact since its completion can be illustrated by examples
in three key areas: partnerships, actions and accomplishments. Through the MN-DPPP, the MDP
demonstrated capacity in the area of convening partners—a role specified by participants for the
state—and strengthened relationships in several key areas. The project also led to new partnerships
among participating organizations, consistent with recommendations regarding sharing and building
on existing resources.
Since this project was completed in 2004, a number of specific actions outlined by the participants
are underway or have been accomplished. MDH hired a chronic disease epidemiologist. This staff
has convened an interest group on chronic disease epidemiology to explore data partnerships and is
developing a chronic disease fact sheet focused on common modifiable risk factors such as poor diet,
physical inactivity and obesity. Another new fact sheet, developed with the MDH Genomics Program,
emphasizes family history as a risk factor for diabetes, and provides recommendations for people who
have this risk factor. MDH has also implemented a workplace wellness initiative, designed to model
what can be accomplished toward employee health promotion on a limited budget.
Results from the MN-DPPP have been used to develop public health goals related to prediabetes for
Minnesota. The MN-DPPP recommendations have strengthened the diabetes prevention component
of the Plan. The Minnesota Diabetes Steering Committee has formed a work group to address diabetes
prevention, which will incorporate these recommendations into their work. Data to identify those at
risk, define the burden and track progress was cited as a key resource needed. In 2004, MDH piloted
BRFSS diabetes prevention measures on glucose screening, diagnosed high blood glucose, and family
history of diabetes.
Finally, several key milestones have been accomplished related to resources. MDH leadership has
used the MN-DPPP results to argue for continued state-level chronic disease prevention funding, and
new federal funding has come through two CDC grants: Steps to a Healthier U.S. and the Diabetes
Primary Prevention Initiative (DPPI). Minnesota’s Steps to a Healthier US grant (2004-2008) funds
diabetes, obesity, and asthma prevention by addressing physical inactivity, poor nutrition, and tobacco
use. Partners include the Minnesota Department of Education and multiple MDH Programs and four
Minnesota communities: Minneapolis, St. Paul, Rochester and Willmar.
Through the DPPI, the CDC has made funds available for diabetes prevention pilot projects in five
states: California, Massachusetts, Michigan, Minnesota and Washington. Table 9 describes the DPPI’s
three focus areas:
Table 9. Focus Areas of the CDC-Funded Diabetes Primary Prevention Initiative (DPPI)
Intervention: Piloting the use of the Improvement Model and the Chronic Care Model to support planning and implementation
of diabetes prevention intervention(s) in diverse settings.
Surveillance: Piloting development of a diabetes primary prevention surveillance system.
Systems Modeling: Pilot testing the utility of system dynamics modeling in support of diabetes goal setting and decision
making.
19Challenges and Opportunities for Diabetes Prevention
All five states are funded for the Intervention focus area. Three (California, Massachusetts and
Minnesota) are funded for the Surveillance focus area, and two (California and Minnesota) are funded
for the Systems Modeling focus area. Funding began in September of 2005. Participating states and
CDC collaborated to define the scope of work and activities. Continued DPPI funding is anticipated
through March of 2008.
The Intervention focus area has created a set of resources and tools for state Diabetes Prevention
and Control Program (DPCPs) to work with key audiences for diabetes prevention: businesses,
communities, consumers, health systems and policy makers. Over the next year, this focus area
will pilot the performance of the tools to enhance existing diabetes prevention efforts. Each of the 5
states will select one or more key audiences and pilot intervention strategies to serve as models for
future programmatic efforts. Surveillance focus area work has involved identifying the prediabetes
population, selecting appropriate indicators for diabetes prevention and determining how to measure
them. As part of this project, Minnesota has continued piloting BRFSS prevention measures during
2006. The System Modeling focus area concerns a computer model of the social, economic and
epidemiological dynamics that give rise diabetes incidence, prevalence, morbidity and mortality. Work
over the next year will involve piloting the model and accompanying learning lab to support decision-
making for diabetes prevention.
Future Opportunities
Participants strongly emphasized that any new diabetes prevention work should build on existing
efforts, and there are several opportunities for such collaboration in Minnesota, including: Steps to a
Healthier U.S.; Indian Health Service prevention grants and prediabetes guidelines; the Blue Cross Blue
Shield dou campaign to promote everyday physical activity; the American Diabetes Association’s work
with members of the Minnesota business community; the Fit City and Fit School award programs;
federally mandated school wellness policies; the Minnesota Child Obesity Task Force; the Eagle Books,
which aim to prevent diabetes in American Indian youth; worksite wellness strategies being piloted at
the Minnesota Department of Health, and local public health priorities for addressing obesity, nutrition
and physical activity.
Minnesota’s Steps to a Healthier US communities are working with schools, workplaces, health care
settings, community-based organizations and community media outlets on a variety of projects to
prevent diabetes. These include school-based walking programs for students (Willmar) and staff (St.
Paul); distributing WIC vouchers for fresh, locally grown produce from the Rochester Downtown
Farmers’ Market; television programs on diabetes prevention created by Emergency and Community
Health Outreach (ECHO) in St. Paul; and a summer health promotion program, Step Up to Health,
with the Minneapolis Park and Recreation Board.
In April 2005, Indian Health Service released the first comprehensive care guidelines in the U.S. for
prediabetes in clinical settings. These guidelines specify who to test, how to test, how to diagnose,
how to document/code, how to manage, what to manage (including goals) and how often to follow up.
20 Facilitated by the Minnesota Department of Health and the Minnesota Diabetes ProgramYou can also read