SHC Clinical Pathway: Inpatient Management of Urinary Tract Infections - Adult Patients
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
SHC Clinical Pathway: Inpatient Management of Urinary Tract Infections – Adult Patients
I. Background: We have adapted national guidelines to assist in the management of adult with UTIs in the inpatient
setting.
II. Exclusion: Prostatitis and acute pyelonephritis complicated by an abscess or nephrolithiasis is outside of the scope of
this guideline. Please consider an infectious disease (ID) or urology consult as appropriate.
III. Procedures/Guidelines:
1) Definitions:
i. Acute uncomplicated UTI: occur in otherwise healthy, non-pregnant, pre-menopausal women with normal
urinary tract anatomy.
ii. Acute complicated UTI: occur in those with risk factors that increase the risk of failing therapy including urinary
tract obstruction, functional or anatomic abnormality of the urinary tract, renal failure, diabetes mellitus,
immunosuppression, hospital-acquired infection, and renal transplant.
iii. Acute uncomplicated pyelonephritis: upper tract infection in otherwise healthy, non-pregnant, pre-menopausal
women with normal urinary tract anatomy.
iv. Acute complicated pyelonephritis: upper tract infection that is complicated by an abscess, nephrolithiasis,
papillary necrosis, or emphysematous pyelonephritis
2) Symptoms:
i. Cystitis: dysuria, urinary frequency, urinary urgency, suprapubic pain, hematuria
ii. Pyelonephritis: fever (>38oC), chills, flank pain, costovertebral angle tenderness, and nausea/vomiting
3) Diagnosis: A positive urine culture may confirm a UTI, but it may also reflect asymptomatic bacteriuria or a urine
sample that was contaminated by bacteria during collection. Urine cultures are most useful if they are only obtained
for patients with high clinical suspicion of UTI. They should not be obtained for asymptomatic patients with dirty-
appearing or smelly urine samples. For patients with an indwelling urinary catheter, samples should be obtained
from newly placed catheter (eg within 5 days) or straight catherization.
1Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
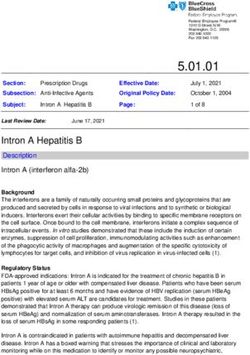
Table 1. 2020 SHC data for E.coli isolated from urine cultures – inpatient setting and emergency department (ED)
No. of Amoxicillin/
Species Ampicillin Cefazolin Ceftriaxone Nitrofurantoin TMP/SMX Cirpofloxacin Levofloxacin
isolates clavulanate
349 45.2% 75.7% 74.9% 79.5% 94% 69.3% 63.6% 58.9%
Inpatient
(332) (333) (343) (332) (349) (332) (332) (333)
Emergency 1063 50.7% 81.8% 84.3% 86.6% 96.6% 71.3% 72.6% 68%
department (992) (992) (1058) (992) (1063) (990) (991) (992)
4) Antibiotic selection:
i. Empiric antibiotic selection is directed at E. coli (the most common uropathogen) and should take into
consideration local resistance patterns (Table 1), recent exposure to antibiotics, and recent history of multi-
drug resistant organisms (MDROs).
1. If a MDRO is identified or the patient has a history of UTIs secondary to MDROs, see the MDRO-
directed antibiotic selection table below (section 5).
Clinical
Treatment Options* Duration** Comments
Syndrome
Pregnant patients: • Fluoroquinolones and doxycycline
are contraindicated throughout
1st line: cephalexin 500 mg PO QID for 7 days (if active pregnancy.
based on urine culture) • TMP/SMX is contraindicated during
the first 8 weeks of pregnancy.
2nd line: Macrobid 100 mg PO BID for 5 days (if active
based on urine culture) • Interpretive criteria for fosfomycin
susceptibility can only be provided
3rd line: fosfomycin 3g PO once (restricted) (if active for E. coli or E. faecalis, as CLSI has
based on urine culture) not established clinical breakpoints
for other organisms.
Asymptomatic
bacteriuria (ASB) Prior to urologic procedures: • Treatment of ASB is indicated prior
to urologic surgeries that break the
1nd line: cefazolin 2 gram IV/IM once 30-60 minutes prior mucosal barrier (i.e. TURP,
to the procedure ureteroscopy including lithotripsy,
percutaneous stone surgery).10
2nd line: ciprofloxacin 400 mg IV once 30-60 minutes
• Treatment is not recommended for
prior to the procedure
urologic procedures that do not
break the mucosal barrier (i.e.
catheter exchange, cystoscopy,
etc.).10
Kidney transplant patients (within 30 days of • Macrobid should be avoided if CrCl <
transplantation only): 30 mL/min.
• Interpretive criteria for fosfomycin
susceptibility can only be provided
2Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
Beyond the intial 30 days post kidney transplant, for E. coli or E. faecalis, as CLSI has
there is evidence to recommend against treatment not established clinical breakpoints
of ASB.10 for other organisms.
1st line: cephalexin 500 mg PO BID for 5 days (if active
based on urine culture)
2nd line: Macrobid 100 mg PO BID for 5 days (if active
based on urine culture)
3rd line: ciprofloxacin 250 mg PO BID for 3 days (if
active based on urine culture)
4th line: fosfomycin 3g PO once (restricted) (if active
based on urine culture)
Clinical
Treatment Options* Duration** Comments
Syndrome
Macrobid 100 mg PO BID 5 days • Often has acitivity against MDROs,
such as ESBLs and VRE.
(preferred based on local resistance • Avoid in elderly women with CrCl
rates, tolerability, and low cost)Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
Ciprofloxacin 250 mg PO BID 3 days • Avoid enteral administration with
antacids.
(should be reserved for use in patients • ADRs: QTc prolongation, black box
who have no alternative treatment warnings (tendinitis, peripheral
options) neuropathy, CNS effects), C.Difficile,
etc.
Levofloxacin 250 mg PO daily 3 days
(should be reserved for use in patients
who have no alternative treatment option)
Clinical
Treatment Options* Duration** Comments
Syndrome
Macrobid 100 mg PO BID 7 days • Often has acitivity against MDROs,
such as ESBLs and VRE.
(preferred based on local resistance • Avoid in elderly women with CrCl
rates, tolerability, and low cost)Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
(should be reserved for use in patients • ADRs: QTc prolongation, black box
who have no alternative treatment warnings (tendinitis, peripheral
options) neuropathy, CNS effects), C.Difficile,
etc.
Levofloxacin 750 mg PO or IV daily 7 days
(should be reserved for use in patients
who have no alternative treatment
options)
Ceftriaxone 1 gram IV daily 7 days • Oral options preferred if the patient is
clinically stable and tolerating orals.
Clinical Treatment Options* Duration** Comments
Syndrome
Ceftriaxone 1 gram IV daily 7 days • Following at least one dose of an IV
beta lactam, step-down to oral
(may be followed by step-down to a PO cephalexin 500 mg PO QID or
agent following initial IV therapy) amoxicillin-clavulanate 875/125 mg
PO BID may be reasonable.
Ciprofloxacin 500 mg PO BID or 400 mg 7 days • Avoid enteral administration with
IV BID antacids.
• ADRs: QTc prolongation, black box
Uncomplicated (Avoid empiric use as there is increasing warnings (tendinitis, peripheral
pyelonephritis resistance to E.coli) neuropathy, CNS effects), C.Difficile,
etc.
Levofloxacin 750 mg PO or IV daily 7 days
(Avoid empiric use as there is increasing
resistance to E.coli)
TMP/SMX 1-2 DS tablets PO BID 10-14 days • ADRs: rash, hyperkalemia, elevated
BUN/SCr, bone marrow suppression.
(Avoid empiric use as there is increasing
resistance to E.coli)
Clinical
Treatment Options* Duration** Comments
Syndrome
Ceftriaxone 2 grams IV daily 7-10 days
5Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
Cefepime 1 gram EI IV every 8 hours*** 7-10 days • It is generally recommended to start
with an intravenous (IV) antibiotic for
initial treatment. Step-down to an
oral agent if active is recommended.
Piperacillin/tazobactam 3.375 gram EI IV 7-10 days
See SHC GNR bacteremia de-
every 8 hours***
escalation guide for pathogen-
directed oral step-down therapy
considerations.
Ciprofloxacin 500 mg PO BID or 400 mg 7 days • Avoid enteral administration with
IV BID*** antacids.
Complicated
• ADRs: QTc prolongation, black box
pyelonephritis or (Avoid empiric use as there is increasing warnings (tendinitis, peripheral
bacteremia resistance to E.coli) neuropathy, CNS effects), C.Difficile,
secondary to a
etc.
urinary source Levofloxacin 750 mg PO or IV daily*** 7 days
(Avoid empiric use as there is increasing
resistance to E.coli)
Pyelonephritis: TMP/SMX 2 DS tablets 10 days • ADRs: rash, hyperkalemia, elevated
PO BID BUN/SCr, bone marrow suppression.
Bacteremia secondary to urinary source:
TMP/SMX 8-10mg/kg/day PO divided in 2
or 3 doses (if MIC ≤20)
(Avoid empiric use as there is increasing
resistance to E.coli)
EI = extended infusion
*Doses should be adjusted based on renal function and other clinical characteristics, please refer to the SHC renal dosing guideline.
**Select high-risk patient populations (i.e. immunocompromised) may require prolonged durations of therapy.
***Pseudomonal dosing is recommended if the patient has a confirmed Pseudomonas infection. Please refer to the SHC renal dosing guideline.
6Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
5) MDRO-directed antibiotic selection:
Pathogen Treatment Options* Duration** Comments
Macrobid 100 mg PO BID 5 days • Oral options are preferred for
uncomplicated cystitis if active.
(not active against P. mirabilis) • Treatment with penicillins, beta
lactam/beta lactamase inhibitors, and
TMP/SMX 1 DS tablet PO BID 3 days
cephalosporins may not be effective
for ESBL-producing organisms even if
Uncomplicated cystitis: 3 days
Ceftriaxone resistant reported as susceptible.7,8
Ciprofloxacin 250 mg PO BID
E.coli, • If piperacillin-tazobactam or cefepime
K.pneumoniae, or Complicated cystitis: Ciprofloxacin was initiated as empiric therapy and
P.mirabilis cystitis 500 mg PO BID or 400 mg IV BID clinical improvement occurs, no
change or extension of antibiotic
Uncomplicated cystitis: therapy is necessary.7
Levofloxacin 250 mg PO daily • Interpretive criteria for fosfomycin
susceptibility can only be provided for
Complicated cystitis: Levofloxacin E. coli, as CLSI has not established
750 mg PO or IV daily clinical breakpoints for K.pneumoniae
or P.mirabilis.
Fosfomycin 3g PO once (restricted) Once
Ertapenem 1 gram IV daily 7 days • It is recommended to start with an
intravenous (IV) carbapenem for
Meropenem 1 gram EI IV every 8 7 days initial treatment. Step-down to an
hours oral agent if active is
Ceftriaxone resistant recommended.
E.coli, Pyelonephritis: TMP/SMX 2 DS 7 days • Treatment with penicillins, beta
K.pneumoniae, or tablets PO BID lactam/beta lactamase inhibitors,
P.mirabilis and cephalosporins may not be
pyelonephritis or Bacteremia secondary to urinary effective for ESBL-producing
bacteremia source: TMP/SMX 8-10mg/kg/day organisms even if susceptible.7,8
secondary to a PO divided in 2 or 3 doses (if MIC • If piperacillin-tazobactam or
urinary source ≤20) cefepime was initiated as empiric
therapy and clinical improvement
Ciprofloxacin 500 mg PO BID or occurs, no change or extension of
7 days
400 mg IV BID
antibiotic therapy is necessary.7
Levofloxacin 750 mg PO or IV daily 7 days
Macrobid 100 mg PO BID 5 days • Many patients with CRE in the
Carbapenem-
urine have a history of recurrent
resistant
UTIs due to anatomical
7Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
Enterobacteriaceae TMP/SMX 1 DS tablet PO BID 3 days abnormalities, neurogenic bladder,
(CRE) cystitis etc. Ensure that patients are
symptomatic before treating.
Uncomplicated cystitis: 3 days
Ciprofloxacin 250 mg PO BID
Complicated cystitis: Ciprofloxacin
500 mg PO BID or 400 mg IV BID
Uncomplicated cystitis: 3 days
Levofloxacin 250 mg PO daily
Complicated cystitis: Levofloxacin
750 mg PO or IV daily
Carbapenem-
resistant
Enterobacteriaceae
Treatment options include ceftazidime-avibactam (restricted), cefiderocol (restricted),
(CRE) pyelonephritis
or meropenem-vaborbactam (non-formulary). ID consult recommended.
or bacteremia
secondary to a
urinary source
Macrobid 100 mg PO BID 5 days • Enterococci are normal flora of the GI
tract, often colonize the urinary tract
Doxycycline 100 mg PO BID 5 days and indwelling urinary catheters, and
Vancomycin treatment is not usually required.
resistant There is limited experience with the
Fosfomycin 3g PO once (restricted) Once
Enterococcus (VRE) use of tetracyclines for urinary tract
cystitis infections.9
• Interpretive criteria for fosfomycin
susceptibility can only be provided for
E. faecalis, as CLSI has not
established clinical breakpoints for E.
faecium.
EI = extended infusion
*Doses should be adjusted based on renal function and other clinical characteristics, please refer to the SHC renal dosing guideline.
**Select high-risk patient populations (i.e. immunocompromised) may require prolonged durations of therapy.
8Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
IV. References
1) Gupta, et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and
Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society
for Microbiology and Infectious Diseases Clinical Infectious Diseases 2011;52(5):e103–e120
2) Grigoryan L, Trautner BW, Gupta K. Diagnosis and management of urinary tract infections in the outpatient setting:
a review. JAMA. 2014 Oct 22-29;312(16):1677-84. doi: 10.1001/jama.2014.12842. Review. PubMed PMID:
25335150.
3) Metlay JP, Strom BL, Asch DA. Prior antimicrobial drug exposure:a risk factor for trimethoprim-sulfamethoxazole-
resistant urinary tract infections. J Antimicrob Chemother 2003; 51:963–70.
4) Pallin DJ, et al. 2014. Urinalysis in Acute Care of Adults: Pitfalls in Testing and Interpreting Results. Open Forum
Infect Dis. 1(1):ofu019. doi: 10.1093/ofid/ofu019
5) Wilson ML and Gaido L. 2004. Laboratory Diagnosis of Urinary Tract Infections in Adult Patients. Clin Infect Dis.
38 (8): 1150-1158. doi: 10.1086/383029
6) Huttner A, Kowalczyk A, Turjeman A, Babich T, Brossier C, Eliakim-Raz N, Kosiek K, Martinez de Tejada B, Roux
X, Shiber S, Theuretzbacher U, von Dach E, Yahav D, Leibovici L, Godycki-Cwirko M, Mouton JW, Harbarth S.
Effect of 5-Day Nitrofurantoin vs Single-Dose Fosfomycin on Clinical Resolution of Uncomplicated Lower Urinary
Tract Infection in Women: A Randomized Clinical Trial. JAMA. 2018 May 1;319(17):1781-1789. doi:
10.1001/jama.2018.3627. PMID: 29710295; PMCID: PMC6134435.
7) Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America
Guidance on the Treatment of Extended-Spectrum β-lactamase Producing Enterobacterales (ESBL-E),
Carbapenem-Resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with Difficult-to-Treat Resistance
(DTR-P. aeruginosa). Clin Infect Dis. 2020 Oct 27:ciaa1478. doi: 10.1093/cid/ciaa1478. Epub ahead of print. PMID:
33106864.
8) Harris PNA, Tambyah PA, Lye DC, Mo Y, Lee TH, Yilmaz M, Alenazi TH, Arabi Y, Falcone M, Bassetti M, Righi E,
Rogers BA, Kanj S, Bhally H, Iredell J, Mendelson M, Boyles TH, Looke D, Miyakis S, Walls G, Al Khamis M, Zikri
A, Crowe A, Ingram P, Daneman N, Griffin P, Athan E, Lorenc P, Baker P, Roberts L, Beatson SA, Peleg AY, Harris-
Brown T, Paterson DL; MERINO Trial Investigators and the Australasian Society for Infectious Disease Clinical
Research Network (ASID-CRN). Effect of Piperacillin-Tazobactam vs Meropenem on 30-Day Mortality for Patients
With E coli or Klebsiella pneumoniae Bloodstream Infection and Ceftriaxone Resistance: A Randomized Clinical
Trial. JAMA. 2018 Sep 11;320(10):984-994. doi: 10.1001/jama.2018.12163. Erratum in: JAMA. 2019 Jun
18;321(23):2370. PMID: 30208454; PMCID: PMC6143100.
9) Heintz BH, Halilovic J, Christensen CL. Vancomycin-resistant enterococcal urinary tract infections.
Pharmacotherapy. 2010 Nov;30(11):1136-49. doi: 10.1592/phco.30.11.1136. PMID: 20973687.
10) Lindsay E Nicolle, Kalpana Gupta, Suzanne F Bradley, Richard Colgan, Gregory P DeMuri, Dimitri Drekonja, Linda
O Eckert, Suzanne E Geerlings, Béla Köves, Thomas M Hooton, Manisha Juthani-Mehta, Shandra L Knight, Sanjay
Saint, Anthony J Schaeffer, Barbara Trautner, Bjorn Wullt, Reed Siemieniuk, Clinical Practice Guideline for the
Management of Asymptomatic Bacteriuria: 2019 Update by the Infectious Diseases Society of America, Clinical
Infectious Diseases, Volume 68, Issue 10, 15 May 2019, Pages e83–e110, https://doi.org/10.1093/cid/ciy1121.
9Stanford Antimicrobial Safety and Sustainability Program
Originally Developed: 11/14/2017
Revised:03/18/2021
V. Document Information
1) Original Author/Date: Marisa Holubar, MD MS & Lina Meng, PharmD
i. Revision Author/Date: Emily Fox, PharmD 2/5/2021
2) Gatekeeper: Antimicrobial Stewardship Program
3) Review and Renewal Requirement
This document will be reviewed every three years and as required by change of law or practice
4) Revision/Review History:
SASS team: 11/14/2017; 1/26/2017; 1/26/2021
5) Approvals
i. Antimicrobial Subcommittee: 11/16/2017; 03/18/2021
ii. P&T: approved 12/2017; 04/2021
This document is intended only for the internal use of Stanford Health Care (SHC). It may not be copied or otherwise used, in whole, or in part,
without the express written consent of SHC. Any external use of this document is on an AS IS basis, and SHC shall not be responsible for any
external use.
Stanford Health Care
Stanford, CA 94305
10You can also read